- Healthcare IT
- Revenue Cycle Management Market
"Designing Growth Strategies is in our DNA"

Revenue Cycle Management Market Size, Share & Industry Analysis, By Structure (In-house and Outsourced), By Type (Software and Services), By Function (Claims & Denial Management, Medical Coding & Billing, Clinical Documentation Improvement (CDI), Insurance, and Others), By End-user (Hospitals, Physician’s Office, and Others), and Regional Forecast, 2024-2032
Last Updated: July 15, 2024 | Format: PDF | Report ID: FBI100275
- Segmentation
- Methodology
- Infographics
- Request Sample PDF
KEY MARKET INSIGHTS
The global revenue cycle management market size was valued at USD 135.92 billion in 2023 and is projected to grow from USD 148.84 billion in 2024 to USD 361.86 billion by 2032, exhibiting a CAGR of 11.7% during the forecast period (2024-2032). Today’s healthcare systems face major challenges such as increasing complexity, rising treatment costs, and growing patient consumerism, among others. These market dynamics pose enormous stress on large hospitals and clinics, driving them to transform into Revenue Cycle Management (RCM) operations. This factor is defined as a process that hospitals design and implement to maximize patient revenue and its collection speed. Several regulatory mandates for the application of Electronic Health Records (EHR) in healthcare settings and preference toward integrated EHR/RCM software for the smooth workflow are surging the demand for this service globally.
Additionally, the increasing number of claim denials and the rising administrative cost for the management of the denied claims are expected to foster the demand for this service in the study period.
- For instance, as per an article published by Etactics, Inc. in February 2023, out of the total in-network claims submitted in 2021, the number of denied claims was 48.3 million. This number accounted for 16.6% of all claims. The insurer denial rates ranged from 1 to 80%.
- Similarly, according to a survey by the Change Healthcare in 2020, the U.S. hospitals experienced a remarkable hike of 23.0% for claim denials in 2020 as compared to 2016. Thus, increasing demand for this service among hospital administrations is bolstering the adoption rate and supporting market growth.
Moreover, medical billing complexity and rising healthcare costs created a drastic rise in demand for outsourcing revenue cycle management solutions across the globe.
The outbreak of COVID-19 had a negative impact on the market growth. Several key market players, including TH Medical and CERNER CORPORATION, witnessed a significant decline in revenue from their RCM services. Additionally, postponement of elective surgeries and a significant decrease in the number of non-COVID-19 patients impacted the revenue of the majority of the hospitals significantly during the pandemic. However, upliftment of lockdown restrictions, increasing non-COVID-19 patients in 2021, and the introduction of advanced software to manage revenue supported market growth in 2021. The market is anticipated to witness significant growth in the coming years.
Revenue Cycle Management Market Trends
Preferential Shift toward Outsourcing Model to Improve Financial Performance
An increasing number of patient admissions and rising complications during the management of operating revenues in healthcare settings are surging the demand and adoption of revenue cycle management. However, a preferential shift is observed in many healthcare facilities from in-house service to outsourcing service due to certain distinct advantages offered by outsourcing this service. The outsourcing model offers a significant improvement of the operational workflow compared to the in-house model while managing claim denials, medical billing & coding, and others. For instance, according to a 2022 PatientPay study from CWH Advisors, the demand for outsourcing RCM is increasing, and around 61% of providers are planning to use RCM tasks in the future. This study was conducted in November and December 2022.
Also, the implementation of artificial intelligence and machine learning to reduce recurrent errors in a claim denial is cost-effective in the outsourcing model compared to the in-house model. For instance, according to the data published by Change Healthcare LLC in 2022, 65.0% of the U.S. hospitals and other healthcare facilities are using AI in their revenue management. These benefits of this model encourage healthcare facilities to adopt the outsourcing model.
Request a Free sample to learn more about this report.
Revenue Cycle Management Market Growth Factors
Regulatory Mandates for Adoption of Electronic Health Records (EHR)/Electronic Medical Records (EMR) to Assist Revenue Cycle Management Market Growth
The introduction of EHRs revolutionized healthcare organizations in collecting, analyzing, and reporting patient data. However, according to an article by QWay Healthcare, Inc., in July 2021, 31.0% of the U.S. healthcare providers were using manual claim denial procedures and experiencing a huge amount of delay and recurrent errors while managing claim denials. Therefore, to reduce operational delay and manual errors, a rising number of healthcare administrations are adopting the EHR/EMR systems.
Eventually, in accordance with the EHR/EMR system, healthcare facilities are focusing on improving workflow of the revenue cycle management procedure. This factor may boost the demand for this service. Further, increasing healthcare spending and technological advancements in the software are expected to fuel the adoption rate and foster the market growth during the study period.
For instance, in July 2021, Access Healthcare introduced Echo, an artificial intelligence and Robotic Process Automation (RPA) platform for introducing automation in the procedure.
RESTRAINING FACTORS
Risks Associated with Healthcare IT Solutions and Budgetary Constraints to Restrain Market
Distinct advantages of the service and advancement of these systems are fueling the demand for this service. However, limited IT infrastructure and budget constraints play a crucial role in hindering market growth.
For instance, according to an article by HIT Consultant Media in 2021, it was reported that 60.0% of a surveyed population consider budget constraints as the root cause of not implementing AI and other advanced technology in the revenue management service.
Furthermore, rising security concerns while protecting the confidential data about patient and healthcare facilities is expected to limit the demand for this service during the study period. For instance, according to a report by IBM Security in June 2023, it was stated that the cost of healthcare data breaches increased from approximately USD 9.23 million in 2021 to USD 10.92 million in 2022 worldwide. These ambiguities are restricting the adoption rate of this service and subsequently restraining market growth.
Revenue Cycle Management Market Segmentation Analysis
By structure analysis.
In-house Segment to Dominate due to Increase in Patient Admissions
Based on structure, the market is segmented into in-house and outsourced. The in-house segment dominated the market share, owing to higher adoption of this service by hospitals to stabilize clinical and financial performance. Also, an increase in the number of patient admissions supports the in-house model's adoption rate. According to the American Hospital Association (AHA) survey, more than 33.0 million hospital admissions were recorded in 2021. Also, the developing hospital infrastructure and health insurance policies in emerging nations are also propelling the demand for these solutions. For instance, the America’s Health Insurance Plans (AHIP) implemented RCM solutions with an aim to lower patient out-of-pocket costs and streamline the financial encounter.
The outsourced segment is anticipated to witness fastest growth due to the shifting trend from in-house to outsourcing model in major countries such as the U.S, the U.K., India, and others. Also, the major cost difference between the software and hardware for the in-house and outsourcing model is responsible for strong CAGR over the forecast period. For instance, according to an article published by Advanced-Data Systems in March 2021, it was estimated that the cost of in-house software and hardware is around USD 8,000.0. However, in the case of the outsource segment, the total service cost is around USD 500.0.
To know how our report can help streamline your business, Speak to Analyst
By Type Analysis
Introduction of Technologically Advanced Software Led to its Dominant Market Share
Based on type, the market is segmented into software and services. The software segment dominates the market share, owing to the launch of advanced solutions to help improve revenue cycle management at hospitals, physician’s facilities, and others. Additionally, in light of the COVID-19 pandemic, several companies have generated lower revenues, which has encouraged them to consult financial advisors to have effective measures. For instance, in May 2020, Objective Capital Partners announced to serve as a financial advisor to RCM Technologies. The company advised them to adopt shareholders' rights plan, which is intended to protect and control the company's service.
The services segment is anticipated to emerge as the fastest-growing during the forecast period. Timely reimbursement, active focus on quality patient care, and reduction in the error while billing and coding are attributable to the growing demand for services such as outsourcing, medical coding and billing services, and others.
By Function Analysis
Claims & Denial Management Segment Dominates due to Launch of Advanced Solutions
On the basis of function, the market is segmented into claims & denial management, medical coding & billing, Clinical Documentation Improvement (CDI), insurance, and others. The claims & denial management segment holds the dominant position, owing to the launch of advanced solutions that reduce claim denials. For instance, in September 2021, Aspirion introduced a secure business intelligence client platform, Aspirion Intelligence, to monitor complex claims revenue cycle performance and reduce claim denials.
The medical coding & billing segment holds the second position, followed by the CDI segment. The high growth rate of this segment is attributable to the increasing demand for medical codes and billing services, owing to the complexities associated with financial management of the end-users.
By End-user Analysis
Hospital Segment to Dominate due to Rising Adoption of RCM Solutions in Hospitals
Based on end-user, the market is categorized into hospitals, physician’s office, and others. The hospitals segment dominated the market in 2023 in terms of market value and share. The dominance of this segment is attributable to rising patient admissions, thus generating higher revenue for hospitals. Hospitals adopt this solution to effectively manage a revenue collection process, thereby contributing to the segment's growth during the analysis period. For instance, according to a survey done by AKASA in 2021, it was stated that more than 78.0% of hospitals in the U.S. are using this service. Additionally, increasing collaborations between hospitals and technology providers further support the dominance of the segment. For instance, in January 2024, VHC Health signed 15-year RCM partnership agreement with Med-Metrix, LLC. This partnership includes all of VHC Health's revenue cycle functions.
The physician’s office segment is likely to grow at a faster rate during the study period. The primary reason for this is the gradual increase in the number of physicians globally. For instance, according to the American Medical Association, it was reported that approximately 49.1% of the total patient care physicians worked in physician offices in 2020. This prominent increase in the number of physicians in physician offices is fostering this solution's adoption rate and supporting the segment's growth.
REGIONAL INSIGHTS
North America Revenue Cycle Management Market Size, 2023 (USD Billion)
To get more information on the regional analysis of this market, Request a Free sample
North America was valued at USD 74.90 billion in 2023. This region accounted for the major revenue cycle management market share due to the presence of leading players. Further, the higher usage of the software/service in the U.S. will augment the regional market growth. Moreover, the launch of innovative solutions by the major players in this region also contributes to the growth of the market in North America. For example, in January 2020, a leading player, R1 RCM, launched the R1 Professional platform to expand its geographical reach. Also, the company, in collaboration with Intermountain Healthcare, launched an innovation center to carry these technology innovations.
Europe accounted for the second position in the global market. The provision of growth opportunities for start-ups to develop effective financial technology is propelling the region's adoption and launch of the service mentioned above. In addition, the majority of healthcare companies are constantly focusing on increasing investment in the development of information technology infrastructure. This factor is also expected to support market growth in this region during the study period. For instance, according to the data published by MedTech Europe in 2022, the European medical technology market accounted for around USD 157.7 billion in 2021, an increase of 6.6% from 2020. The top five biggest markets are Germany, France, the U.K., Spain, and Italy.
Asia Pacific is expected to emerge as the fastest-growing region during the forecast period, owing to increasing awareness about the advantages of RCM service among hospitals. Their rising adoption rate is responsible for the higher growth of the region.
Furthermore, Latin America and the Middle East & Africa markets are likely to witness considerably slower growth, owing to the gradual penetration of advanced solutions into the healthcare financial management systems.
List of Key Companies in Revenue Cycle Management Market
Innovative Solutions & End-to-End Service to Clients Help Players Gain Top Position
The market structure is fragmented, with several players operating in the market of revenue cycle management. Epic Systems Corporation accounts for the major share in the market. The company provides end-to-end service that focuses on efficiency, production, and budget needs. Also, the adoption of this company’s EHR and RCM system is assisting the company to sustain its dominant position.
For instance, in February 2020, Advent Health, a Florida-based health system of 50 hospitals, announced a partnership with Epic Systems to adopt its integrated EHR and RCM system for physician practice, ambulatory, urgent care, home health, and hospital facilities.
Other prominent players operating in the market are Allscripts Healthcare, LLC, Cerner Corporation, Conifer Health Solutions, LLC, GeBBS Healthcare Solutions, Inc., MEDHOST, McKesson Corporation, Medical Information Technology, Inc. (MEDITECH), Optum Inc., and R1 RCM, Inc.
LIST OF KEY COMPANIES PROFILED:
- Allscripts Healthcare, LLC (U.S.)
- Cerner Corporation (U.S.)
- Conifer Health Solutions, LLC (U.S.)
- Epic Systems Corporation (U.S.)
- GeBBS Healthcare Solutions (U.S.)
- MEDHOST (U.S.)
- McKesson Corporation (U.S.)
- Medical Information Technology, Inc. (MEDITECH) (U.S.)
- Optum Inc. (U.S.)
- R1 RCM, Inc. (U.S.)
KEY INDUSTRY DEVELOPMENTS:
- February 2024: Availity and Janus announced a strategic collaboration to improve revenue cycle operations in healthcare.
- November 2023: HFMA co-developed an adoption model for revenue cycle management technology.
- June 2023: OnPoint Healthcare and Office Ally partnered for the expansion of offerings to healthcare providers. Through this, OnPoint now offers the latter company’s advanced Revenue Cycle Management (RCM) solutions to hospitals, health systems, providers & Federally Qualified Health Centers (FQHCs).
- October 2022: Nym Technologies SA launched a radiology coding solution for revenue cycle management. This launch surged automation in emergency department, urgent care and radiology facilities, bringing Nym’s medical coding engine to three outpatient specialty areas.
- August 2022: Revecore Technologies acquired Kemberton and Cura Revenue Cycle Management, LLC, two specialized RCM firms. The acquisition has helped Revecore to drive improved outcomes for health systems in the U.S.
- June 2022: Olive launched its Autonomous Revenue Cycle (ARC), the company's flagship RCM suite of solutions. This launch helped Olive to focus more on patient care and easing employee pressure.
- October 2021: R1 RCM, Inc. announced that American Physician Partners extended its R1's revenue cycle management services partnership until 2031 to continue growth in emergency medicine.
- May 2021: Optum, Inc. collaborated with Bassett Healthcare Network to provide RCM services to Bassett's clinics and improve patient care in Central New York.
REPORT COVERAGE
An Infographic Representation of Revenue Cycle Management Market

To get information on various segments, share your queries with us
The revenue cycle management market research report covers a detailed analysis and overview. It focuses on key aspects such as competitive landscape, structure, type, function, end-user, and region. Moreover, it offers insights into the market drivers, market trends, market dynamics, and other key insights. In addition to the factors mentioned above, the report encompasses several factors that contributed to the market growth in recent years.
Report Scope & Segmentation
|
|
| 2019-2032 |
| 2023 |
| 2024 |
| 2024-2032 |
| 2019-2022 |
| CAGR of 11.7% from 2024 to 2032 |
| Value (USD billion) |
|
|
| |
| |
| |
|

Jignesh Rawal ( Assistant Manager -Healthcare )
Frequently Asked Questions
Fortune Business Insights says that the global market stood at USD 135.92 billion in 2023 and is projected to reach USD 361.86 billion by 2032.
In 2023, the North America market stood at USD 74.90 billion.
The market is expected to exhibit a CAGR of 11.7% during the forecast period (2024-2032).
The in-house segment is set to lead the market by structure.
Adoption of integrated EHR/RCM system among healthcare facilities will drive market growth.
Epic Systems Corporation, Cerner Corporation, and R1 RCM, Inc. are some of the leading players in the global market.
North America dominated the market in 2023.
Increasing patient volume and introduction of technologically advanced software are expected to drive the adoption of these products.
Seeking Comprehensive Intelligence on Different Markets? Get in Touch with Our Experts
- STUDY PERIOD: 2019-2032
- BASE YEAR: 2023
- HISTORICAL DATA: 2019-2022
- NO OF PAGES: 195
Personalize this Research
- Granular Research on Specified Regions or Segments
- Companies Profiled based on User Requirement
- Broader Insights Pertaining to a Specific Segment or Region
- Breaking Down Competitive Landscape as per Your Requirement
- Other Specific Requirement on Customization

Healthcare Clients

Related Reports
- Electronic Health Records (EHR) Market
- Telemedicine Market
- Connected Healthcare Market
Client Testimonials
“We are quite happy with the methodology you outlined. We really appreciate the time your team has spent on this project, and the efforts of your team to answer our questions.”
“Thanks a million. The report looks great!”
“Thanks for the excellent report and the insights regarding the lactose market.”
“I liked the report; would it be possible to send me the PPT version as I want to use a few slides in an internal presentation that I am preparing.”
“This report is really well done and we really appreciate it! Again, I may have questions as we dig in deeper. Thanks again for some really good work.”
“Kudos to your team. Thank you very much for your support and agility to answer our questions.”
“We appreciate you and your team taking out time to share the report and data file with us, and we are grateful for the flexibility provided to modify the document as per request. This does help us in our business decision making. We would be pleased to work with you again, and hope to continue our business relationship long into the future.”
“I want to first congratulate you on the great work done on the Medical Platforms project. Thank you so much for all your efforts.”
“Thank you very much. I really appreciate the work your team has done. I feel very comfortable recommending your services to some of the other startups that I’m working with, and will likely establish a good long partnership with you.”
“We received the below report on the U.S. market from you. We were very satisfied with the report.”
“I just finished my first pass-through of the report. Great work! Thank you!”
“Thanks again for the great work on our last partnership. We are ramping up a new project to understand the imaging and imaging service and distribution market in the U.S.”
“We feel positive about the results. Based on the presented results, we will do strategic review of this new information and might commission a detailed study on some of the modules included in the report after end of the year. Overall we are very satisfied and please pass on the praise to the team. Thank you for the co-operation!”
“Thank you very much for the very good report. I have another requirement on cutting tools, paper crafts and decorative items.”
“We are happy with the professionalism of your in-house research team as well as the quality of your research reports. Looking forward to work together on similar projects”
“We appreciate the teamwork and efficiency for such an exhaustive and comprehensive report. The data offered to us was exactly what we were looking for. Thank you!”
“I recommend Fortune Business Insights for their honesty and flexibility. Not only that they were very responsive and dealt with all my questions very quickly but they also responded honestly and flexibly to the detailed requests from us in preparing the research report. We value them as a research company worthy of building long-term relationships.”
“Well done Fortune Business Insights! The report covered all the points and was very detailed. Looking forward to work together in the future”
“It has been a delightful experience working with you guys. Thank you Fortune Business Insights for your efforts and prompt response”
“I had a great experience working with Fortune Business Insights. The report was very accurate and as per my requirements. Very satisfied with the overall report as it has helped me to build strategies for my business”
“This is regarding the recent report I bought from Fortune Business insights. Remarkable job and great efforts by your research team. I would also like to thank the back end team for offering a continuous support and stitching together a report that is so comprehensive and exhaustive”
“Please pass on our sincere thanks to the whole team at Fortune Business Insights. This is a very good piece of work and will be very helpful to us going forward. We know where we will be getting business intelligence from in the future.”
“Thank you for sending the market report and data. It looks quite comprehensive and the data is exactly what I was looking for. I appreciate the timeliness and responsiveness of you and your team.”
Get in Touch with Us
+1 424 253 0390 (US)
+44 2071 939123 (UK)
+91 744 740 1245 (APAC)
[email protected]
- Request Sample

Jignesh Rawal
Assistant manager - healthcare.
Jignesh is a skilled practitioner with over 8 years of extensive experience in market analysis and advisory services within the medical devices, pharmaceuticals, and life sciences & biotechnology sectors. His career journey has equipped him with a deep understanding of market dynamics and strategic insights that drive business growth. He specializes in research within various domains, including cardiology, cosmetics, neurology, and wound care, among others.
In addition to his experience in market analysis, Jignesh brings valuable experience in procurement and supply chain logistics management, gained during his 3 years with a pharmaceutical distribution company. This background enhances his strategic perspective, allowing him to offer comprehensive solutions that address both market trends and operational efficiencies. He has assisted numerous clients in product introduction and analysis of market scenarios.
Jignesh has also been instrumental in projects for leading companies such as Koninklijke Philips N.V., Novartis AG, Pfizer, and Siemens AG, among others. His ability to distill complex data into actionable insights has earned him a reputation as a trusted advisor among his peers and clients alike. Jignesh’s analytical acumen and strategic mindset position him as a valuable asset to any organization seeking to navigate the evolving landscape of the medical devices and life-science sectors.
Sharing this report over the email

The global revenue cycle management market size is projected to grow from $148.84 billion in 2024 to $361.86 billion by 2032, at a CAGR of 11.7%
Read More at:-

Optum opening new competitive terrain in Revenue Cycle Management
- November 21, 2021
- IN Payers , Providers
What is revenue cycle management?
Revenue cycle management (RCM) is the process of converting care delivery into cash. At its most comprehensive, services include:
- patient intake (scheduling/registration, coverage verification and financial counseling)
- claim submission (charge capture, coding, documentation, submission), and
- payment capture (payment processing, denials, customer service and collections).
Effective RCM is challenging because of:
- The variety of plans and benefits designs (what’s covered, patient co-pays, rates, etc.),
- Ambiguities of payer approval of specific clinical services (prior authorization, etc.),
- Requirements and opportunities in characterizing the care and patient risk (e.g., coding),
- Complexity of contracts (e.g., getting appropriate credit for value-based deals), and
- Evolving regulations (e.g., all the Covid emergency measures).
Given this complexity and importance of the ultimate deliverable (cash), providers spend a lot on RCM—between $50-100B overall.
RCM outsourcing small but growing
While only 20-30% of RCM is outsourced today, [1] that share is growing fast. Here’s why: as it is a back-office function, RCM is not usually seen by providers as a basis for strategic advantage. On the other hand, because expertise and technology are key to effective RCM, operational scale is critical. Therefore, consolidating RCM across multiple delivery systems onto a “utility” vendor operating on a white label basis can benefit each (by pooling scale) while harming none.
Logically enough, several of the largest delivery systems—Ascension, HCA, Tenet, and Bon Secours Mercy —have spun their internal RCM functions into subsidiary/co-owned companies (as R1, Parallon, Conifer, and Ensemble, respectively, making up 4 of the top 5 end-to-end RCM outsourcers) and sell services to other providers (with mixed success [2] ). Most often, these deals look like classic business process outsourcing (BPO), with the client’s RCM staff rebadging on the contract’s Day One to become employees of the vendor.
These vendors largely have remained stand-alone “pure plays.” Dimensions of competition have focused on adding scale, automation/digitization, and improving patient experience with the administration aspects of care. [3]
Optum using an RCM BPO anchor to build more strategic relationships
Optum360 is the outlier among the Big Five given its very different corporate parentage and sibling relationships (as a company within OptumInsight and part of UNH overall).
Historically, Optum360 played the game in end-to-end RCM BPO the same as the pure plays [4] and done well with it. [5]
In four recent deals involving RCM, however, OptumInsight has bundled additional services into RCM BPO drawn from the rest of its product portfolio:
- IT management services outsourcing (across two deals),
- Advanced analytics (across all four deals),
- Ambulatory case and care management plus strategic project management (Boulder Community Health), and
- Inpatient care management (SSM Health).

The IT services product seems similar to RCM in that the delivery system is swapping out a well-defined subscale back-office function for a better scaled vendor. The advanced analytics and care management services are different:
The analytics are described as providing the point of care with targeted care recommendations, serving up disparate patient SDoH information, and driving more consistent clinical decision-making. SSM, in particular, is expecting the analytics to “reduce care variation” and support a “new inpatient delivery model” to reduce length of stay (LOS) (perhaps tying in the SDoH data to facilitate more nuanced discharge planning).
The care management is a rebadging of client staff: Boulder is transitioning its nurse care managers, nurses, and social workers overseeing populations in the ambulatory setting (as well as directly engaging with patients) over to Optum career tracks. SSM is planning on transitioning ~300 of its inpatient care managers to the Optum organization.
Essentially, these systems are handing over some of the keys to operating key aspects of care within the delivery system, making the relationship more strategic.
Logic for the bundle
There are a lot of potential synergies from combining RCM, analytics, and care management. A few quick scenarios:
- Analytics flags SDoH barriers for a patient, RCM identifies resources to address them (e.g., out of a value-based agreement), and care management put the solutions in place,
- RCM identifies the payment model and benefit design for an admitted patient (e.g., % of charges, DRG, capitation) early enough so that case management can design a care plan which optimizes fixed cost/variable cost trade-offs and patient cost share,
- Case managers keep RCM in the loop on patients with upcoming procedures so RCM can expedite payer authorization, reducing payment uncertainty at discharge, [6]
- Analytics predicts a patient’s post-acute trajectory at admission, giving discharge planners plenty of time to tweak discharge timing and line up resources.
In any of these scenarios, rewiring of the cross-functional workflow is required. Carving care management over to Optum (in the case of Boulder and SSM) implies a few things:
- The change management challenges behind this rewiring can be addressed more easily if the insights and the execution are organizationally integrated,
- The ultimate fruits of this rewiring outweigh any frictions of having care management and care delivery report up different chains of command, and
- Optum likely has performance components in these agreements (a natural corollary to owning the execution), strengthening the strategic aspects of the partnership.
Not every delivery system will find a broader bundle attractive (John Muir and Bassett, for example, evidently wanted to keep control of execution). But the appeal of Optum’s offer also won’t just be for marginal or struggling systems either: SSM is a very large, $8B multi-regional system with its own health plan and PBM, well-respected by bond holders. And while it is usually the #2 in each of its markets, its average LOS is significantly less than its surrounding competitors (with comparable case mix indices) and average bed occupancy is marginally higher. Of course, aggregate data may mask targeted opportunities for improvement which Optum can surface. [7] SSM’s lower share of surgical cases relative to competitors suggests some opportunity for admission mix improvement. [8] See exhibit.

Implications
By expanding the scope of services from back-office into clinical, OptumInsight is building strategic relationships with delivery systems “from the inside out.” This pairs well with the relationship UNH’s health plan can build “from the outside in.” In the case of John Muir, for example, where there are several product alignments. [9]
Other RCM BPO vendors face a real threat. Right now, they cannot match OptumInsight’s analytical/care management bundles. If OptumInsight’s offer gains traction (and the SSM win is certainly a big reason to think that it will), these players will need new capabilities to compete (most likely inorganically). But even if they can acquire comparable capabilities, Optum is already a step ahead with ready to go outsourced hospitalist services (Sound Physicians) and post-acute optimization (naviHealth) as logical extensions on its analytically driven inpatient care management. [10]
More generally, Optum is setting up a powerful flywheel. The more services these systems buy from Optum, the more Optum effectively becomes the “Intel inside” of delivery system performance, the better these systems perform and the better value they deliver United’s health plan. Many of these delivery systems said they chose Optum to avoid having to join up with other systems, as a way to “stay independent.” Ultimately, however, these systems will become—despite their legal independence and non-profit status—de facto extensions of Optum’s influence on US healthcare.
Managing Partner
[1] The long tail of small-scale vendors and clients (such as small physician practices) make estimating the market size and outsourcing share challenging, so estimates vary widely. Data noted is taken from Ensemble Health (their S-1) at the lower end and from R1 (from analyst reports commenting on the company) at the upper end. An industry rule of thumb is that average RCM costs are about ~5% of revenues and 5-10% of a typical delivery systems’ employee base (when RCM is insourced).
[2] Sometimes, financial investors (e.g., going public or taking on private equity) take a share of the subsidiary to provide focus on the external growth agenda. And sometimes they don’t, and the vendor stays introspective: for example, Conifer is jointly owned by Tenet (76%) and CommonSpirit (24%) and the vast majority of Conifer’s $1.3B in revenues (83%) still come from its parents. Parallon is also widely regarded as focusing on internal customers. Notably, Tenet is reportedly planning on spinning out Conifer into a public offer in 2022.
[3] Over last few years, R1, for example, has:
- Acquired Intermedix (with a large physician practice ambulatory footprint) in 2018 and Cerner’s struggling RCM operation in August 2020, adding customers to its platform,
- Acquired SCI Solutions in April 2020, which supports digital front door strategies such as self-serve scheduling and patient access, and VisitPay in May 2021, a digital consumer payments platform, and
- Invested in digital transformation (launching a dedicated office in November 2018) and machine learning to support automation (first machine learning model implemented in 3Q in 2020).
[4] Optum360 made its big play for growth in 2013 with an alliance with Dignity, taking over its operations in return for a minority share in Optum360. See Marrying into the right family: the bets underlying United’s revenue cycle management joint venture with Dignity Health . CommonSpirit (which succeeded Dignity in its ownership share) recently reduced its ownership stake in Optum360 from 23% (a position which arose out of the September 2013 alliance) to 4.15% in March 2021 by selling shares back to UNH.
[5] See Marrying into the right family pays off! Update on revenue cycle management joint venturing .
[6] A few years ago, RCM outsourcer Parallon found that 24% of their client’s write-offs were for inpatient clients which remained unauthorized at point of discharge. Declining LOS leaves less time for busy case managers to secure payer approvals. Parallon—stuck in the RCM work scope—could only propose throwing more denial resolution bodies retroactively at the problem for marginal improvement. See Parallon “Preventing Denials through Teamwork, Innovation and Technology,” Perspective Brief white paper available on their website and dated 2015.
[7] For example: SSM’s second largest hospital, St. Anthony in Oklahoma City has occupancy of 74% vs. 67% for the local market and surgical share of care delivery of 31% of discharges vs. 36% of discharges for its competitors. If more bed capacity could be opened, St. Anthony’s might be able to increase its share of profitable surgeries in this market. Notably, St. Anthony’s surgical case mix index was also lower than the market average (3.06 vs. 3.15).
[8] To the extent that the Optum deals free up bed capacity, perhaps some other Optum assets could help their clients sort out the most profitable surgeries to fill those beds such as some of the Advisory Board analytical tools.
[9] These include:
- UNH’s Signature Value product in California couples John Muir in the Bay Area with its OptumCare delivery network in Southern California
- UNH uses Canopy Health (a John Muir joint ventured delivery network) to cover John Muir employees
- UNH launched the California Doctors Plan in 2020 with Canopy promising premium savings of up to 25%.
[10] Granted, these would likely take some work to put into reality. All the assets in the four deals discussed here are part of OptumInsight while Sound and naviHealth are part of OptumHealth. Despite the common parent and a lot of marketing spin about the UnitedHealth “family,” individual parts of Optum are very competitive and collaborating across BU’s does not always come naturally.
- Diagnostics
- Digital Health
- Medical Devices
- NEJM Highlights
- Irina Ahmad
- Nikhil Bhojwani
- Jason Brauner
- Sarah Dolman
- Marc Herant
- Alyssa Idusuyi
- David Kaufmann
- Tess Niewood
- Maggie Pickard
- Sophie Ranen
- Anja Schempf
- Harry Sultan
- Thomas Uhler
- Jacob Wiesenthal
- Lilian Zhang
July June May April February January
December November October September August July June May April March February January
December November October September August June March February January
December November October September August July June May April March January
December November October September July June May April March February January
December November October August July May April March February January
December October August July June May April March February January
December November October September August June May April March February January
November October September June May March
November October September August July April March
December October September August July June May April March February January
An opinionated take on NEJM highlights for the second quarter of 2024
Walmart Health didn’t test the opportunity in rural underserved markets
Beyond drug supply: BIOSECURE and early-stage drug R&D
An opinionated take on NEJM highlights for the first quarter of 2024

rcm business plan | rcm marketing plan 2021
Today we are going to discuss about the Rcm Business Plan in this article. We will discuss in detail what is Rcm business plan, how to join Rcm business plan, what are the benefits of Rcm marketing plan. We will also tell you what is Rcm Business.
How you can make money with little efforts under Rcm marketing plan 2021. Rcm is a direct selling MLM (Multi Level Marketing) Indian company. Rcm is a product based MLM company of India.
Before we start our article about the Rcm business plan, first we should know about the Rcm company history and profile and who owns Rcm company. So, let’s know about these questions.
Guys, as said above, Rcm is a direct selling MLM company of India . It was set up by a clothing trading company “Fashion Suitings Pvt Ltd.” at Bhilwara in Rajasthan since 1977 by the Chhabra Group. In 1986 Rcm business started its own production. It was founded by Trilok Chand Chhabra (Owner of Rcm Business).

Sh. Trilok Chand wants to remove all the intermediators between the manufacturer and the final customers, so that product may be available to customer at a low price. His idea was to start a direct selling company. As a result, the Fashion Suiting Pvt Ltd. Company transformed to an Rcm Business, a direct selling MLM company.
Today Rcm is manufacturing around 730 products, having 8 million distributors and 1000 Pickup Centre all over the India. Rcm Business currently manufacturing almost all types of products like health supplements and herbal medicines, food and grocery, clothing for children, women and men as well as a wide array of other stuff such as bags, stationery, tools and many more. Now let’s begin today’s article and learn about the Rcm business plan 2021.
Rcm Business Plan
Guys today we will learn about the Rcm business plan 2021 in detail and know that how you can earn money under Rcm business and marketing plan. Guys as discusses earlier Rcm business comes under Right Concept Marketing, which is a kind of multi-level networking business which is owned by Chhabra Group.
Guys as told; Rcm company is a product based direct selling multi-level marketing company. Now you may be thinking that why its important to join Rcm business plan and what are its benefits to us. So, let’s understand it with an example that what is the benefits to buy a product from Rcm business.
A XYZ company manufacture a product, whose manufacturing cost amounts up to Rs. 100. After that, when a company launch that product in the market, they need to do product promotion which amounts up to Rs. 50.
After that product goes to the selling agency which add their profit. Let’s assume they add Rs. 20 as their profit in the product cost. Now the product goes to wholesaler and then he will add his profit up to Rs. 20 and after that product goes to the retailer and he will also add his profit up to Rs. 10.
After add all these cost the product reaches to the final customer. Now product price which will customer need to pay for that product amounts Rs. 200 (Rs. 100 for manufacturing cost and company profit + Rs. 50 for product promotion + Rs. 20 as selling agency profit + Rs. 20 as wholesaler profit + Rs. 10 as retailer profit).
Guys, this is the big disadvantage of regular system which is followed by our Indian market. Rs. 100 amounting product is provided to the final customer in Rs. 200. You can easily see the drawback of this system. Whereas on other hand is direct selling method is here under Rcm business plan.
In direct selling company, all the extra cost like promotion cost, profits of selling agency, wholesalers and retailers. Under direct selling method, final customer gets the product at low price by eliminating the wasteful extra cost. Also, the Rcm group provide you 100% pure products and good quality products.
In this way, Rcm marketing plan is 100% beneficial for us as compare to buy the goods from the market because with direct selling system, Rcm business plan also allow us to earn some money, in the form of retail profit, performance bonus, royalty bonus, and technical bonus.
So, let’s know how to earn under Rcm marketing plan. To get benefits of Rcm marketing plan you first need to join Rcm business. So, below is the process of joining Rcm business. Let’s see it first.
First Step: First you need to visit official website of Rcm business i.e., www Rcmbusiness com or another way is just going to playstore and search for Rcm business official app and download /install it in your android smart phone.
Second Step: Then click on the direct seller option which will be showing on the left side of the website and then many options will be shown in front of you. You have to click on the e KYC application for New Direct Seller.
Third Step: Once you click on the e KYC application for New Direct Seller option then a registration form will open in front of you. Now you need to fill your detail in the form and submit it in the online mode. You need to fill following information.
Applicant Personal Details
As soon as you click, a new interface will appear in front of you, in which you have to enter the applicant personal details. First of all, it is the sponsor number, before filling it, it is necessary to know what it is.
Sponsor Number is the person under whom you are joining. Whose ID is at the bottom, below which you are joining is your sponsor number.
After this you need to enter Proposer Number, this number of the one, who proposes you to join Rcm business. Now you get to see Gender column under it. After this comes the marital status.
Now it is the turn of the name title, in this you will get Mr. or Mrs. Which you have to select. After filling this in Joining in Rcm Business Plan, you have to fill the Applicant Name in it.
After this, you have to upload applicant picture for the joining of the applicant in Rcm Business Plan. After this, the name of your father and after that the date of birth will have to be filled.
Applicant Nominee Details
After this comes Nominee details, in this you have to fill the information related to your Nominee. Like their name, date of birth and relation and address.
Applicant Communication Details
Then in next you need to enter your communication details joining in Rcm Business Plan. In this your address, state, district, tehsil, post office, city and pin code will be entered.
Along with this, you need to enter your mobile number, you have to fill the same number that you have with you while filling the form because you will get One Time Password on it and you will have to fill it.
After this you will also have to give an ID proof of yours. In this you can also give your Aadhar Card. Along with this, you will also have to upload a photo of your ID proof .
You can also give Pan Card and Driving License instead of Aadhaar Card. You can give your Aadhar card as Address Proof for joining in Rcm Business Plan. You need to upload both side of your Aadhar card.
Applicant Bank Details
After this comes Bank Details, in this you have to fill the name of the bank, bank branch name and your account number, after which you have to upload the first page of your bank account passbook on which the account number and IFSC code are given. Now you have to fill PAN card details. It’s your wish, you can fill it if you want.
Security Details
After this comes the Security Details. In this you have to make your password as per your wish and fill it. After that you have to confirm it by filling it again. In Joining in Rcm Business Plan, now select Hint Question as soon as you click on it, many options will come in front of you, you can take any one.
After this comes Hint answer, in this you have to write the answer to that question. This hint question will be asked from you when in future you forgot your password and wants to reset it.
Applicant Family Details
After this, in Joining in Rcm Business Plan, you get another option in which if any of your family member is already in Rcm then you have to fill the details related to it like their ID Number, if not then you can leave it.
At the end you will get that you have read all the terms and conditions and you agree to them. You have to select it. After this you have to click on Send OTP in Joining in Rcm Business Plan. Thus, OTP will come on the number that you entered. Your joining will start as soon as you fill form and submit it. After submitting your form, you will get a reference number.
Additional Read : Rcm Songs
In this way you can join under Rcm marketing plan. And now we will discuss what are the benefits you will get after join Rcm under Rcm marketing plan 2021. Following listed are the benefits of Rcm marketing plan 2021. We will also discuss them in detail.
List of Profits Under Rcm marketing plan 2021.
Retail Profit : One of the main benefits of Rcm Business plan 2021. You can buy the product from the Rcm pick up point at a discount rate up to 10-20% and then sell these products at M.R.P to other customers. In this way you earn profit which is known as retail profit. Let’s understand this with an example.
Let’s assume that you are a direct seller under Rcm business plan. Now you purchased a product from Rcm pickup point whose M.R.P is Rs. 100. You will get that product at a 20% discount price rate i.e., Rs. 80. Now if you sell this product at M.R.P then you get Rs. 20 as a retail profit.
Discount up to 10-20%: Under Rcm business plan 2021, you get the Rcm products at a discounted rate from the M.R.P. You get 10 to 20% of discount rate depending upon your BV (business volume). You just need to join Rcm business plan first and then enjoy the Rcm products at a discounted rate.
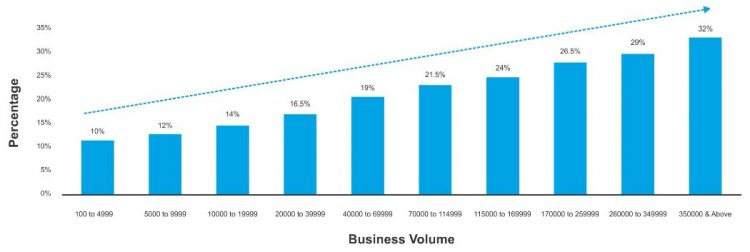
Performance Bonus
To know about this, you should first know about the BV because your performance bonus depends upon your BV points and your group BV.
BV stands for Business Volume. Every product that you buy from the Rcm has BV points. Yours and your groups BV points are added together in the end of the month and the commission is given to you as a performance bonus up to 32% depending up on your BV points.
Further you have to distribute this commission with your group . Business volume table is given below. Let’s see this and understand the calculation of Performance bonus with the help of an example given below the table of performance bonus.
| 100-4999 BV | 10% |
| 5000-9999 BV | 12% |
| 10,000-19,999 BV | 14% |
| 20,000-39,999 BV | 16.5% |
| 40,000-69,999 BV | 19% |
| 70,000-1,14,999 BV | 21.5% |
| 1,15,000-1,69,999 BV | 24% |
| 1,70,000-2,59,999 BV | 26.5% |
| 2,60,000-3,49,999 BV | 29% |
| 3,50,000 and above | 32% |
Calculation of Performance Bonus
Example: Purchase in A leg (group)= 80,000 B.V.
Purchase in B leg (group)= 16,000 B.V.
Purchase in C leg (group)= 14,000 B.V.
Self-purchase = 5,000 B.V.
Total Business Volume = 1,15,000 B.V.
Calculation of Performance Bonus:
Bonus of total group (1,15,000 x 24%) = 27,600/-
Less Bonus of A leg (80,000 x 21.5%) = 17,200/-
Less Bonus of B leg (16,000 x 14%) = 2,240/-
Less Bonus of C leg (14,000 x 14%) = 1,960/-
Net performance bonus = 6,200/-
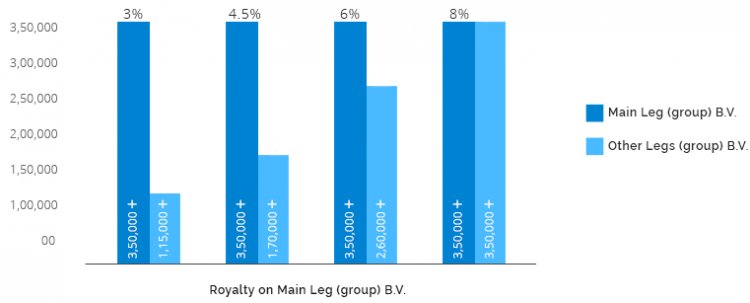
Royalty Bonus
Royalty Bonus is given up to 8% on the basis of your business volume points. Royalty Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Royalty is given on the basis of difference by deducting downline royalty from the total royalty. Royalty always calculated on monthly basis.
When a group other than the main group able to make their BV up to 3,50,000 BV or more, it is called second leg (group) and if the other group (other than the main and second group) make their BV points of 1 15,000 or more than they will also get royalty at the second group as per the applicable slab.
Additional Read : Royalty in 1 Month
The royalty slab table is given below you can see from the table that how much percentage of royalty bonus you will earn on the basis of your BV.
| Main leg business volume | Other Leg’s Business Volume | Royalty on business volume of main leg |
| 3,50,000 or more | 1,15,000 or more | 3% |
| 3,50,000 or more | 1,70,000 or more | 4.5% |
| 3,50,000 or more | 2,60,000 or more | 6% |
| 3,50,000 or more | 3,50,000 or more | 8% |
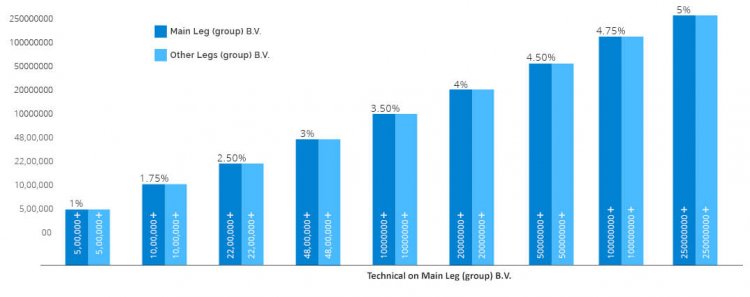
Technical Bonus
Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Also, he or she should be successfully earning the royalty income up to 8% percent for consecutive 3 months. Technical bonus is given on the basis of difference by deducting downline technical bonus from the total technical bonus. Technical bonus is always calculated on monthly basis.
When a group other than the main group able to make their BV up to 5,00,000 BV or more, it is called second group and if the other group (other than the main and second group) make their BV points of 5,00,000 or more than they will also get technical bonus at the second group as per the applicable slab.
Additional Read : Check Rcm Business Income
The technical slab table is given below you can see from the table that how much percentage of technical bonus you will earn on the basis of your BV.
| 5,00,000 or more | 5,00,000 or more | 1% |
| 10,00,000 or more | 10,00,000 or more | 1.75% |
| 22,00,000 or more | 22,00,000 or more | 2.50% |
| 48,00,000 or more | 48,00,000 or more | 3% |
| 100,00,000 or more | 100,00,000 or more | 3.50% |
| 200,00,000 or more | 200,00,000 or more | 4% |
| 500,00,000 or more | 500,00,000 or more | 4.50% |
| 1000,00,000 or more | 1000,00,000 or more | 4.75% |
| 2500,00,000 or more | 2500,00,000 or more | 5% |
Important Facts of Rcm business plan 2021
Here we will discuss some important facts about Rcm Business Plan. These are given below :
- Rcm (Rcm Business Plan) company includes 750 plus products.
- Rcm has more than 15000 thousand stores across India
- Rcm business headquarter is located in Bhilwara, Rajasthan.
- Rcm company has started opening Rcm Wonder World in big cities all over India, where you will get all the products at one place.
- Rcm (Rcm Business Plan) is a product based direct selling company.
- Rcm has very strong roots.
- Rcm is the only company that makes products based on Indian mindset.
- In Rcm you can earn lakhs of rupees in less time with less efforts.
- In Rcm (Rcm Business Plan), you can become a distributor of Rcm by buying a product worth one thousand rupees.
- Rcm (Rcm Business Plan) is Indian MLM (Multi-level Marketing) company.
- Direct Selling Rcm Business Benefiting its customers by providing them pure & genuine products.
- Cheap Product along with Bill for every single purchase. Rcm Business Plan provides a fare bill of even one rupee of purchase is made.
- Under Rcm marketing plan 2021 you get 10-20 percent discount. 10-32 percent performance bonus in your bank account, 3-8 percent royalty income generation, 1-5 percent technical income.
- Rcm business follows all the government rules and regulations and strictly follow the guidelines of govt. for direct selling company. They pay their total liable tax to the Government of India.
- Rcm marketing plan 2021 provides you self-employment opportunity.
Auspicious opportunity to fulfill all your dreams, being a participant in the progress of GDP of the country, also giving right direction to health with pure products. Awakening the spirit of helping each other.
What is Rcm Business?
Guys, Rcm business works on direct selling MLM method. This method is known as Right Concept Marketing. Friends we already have discuss about the benefit of direct selling method up on the regular method prevailing in Indian market.
Rcm business is one of the major role players in the industry of direct selling multi-level marketing. Let’s see how the Rcm business come into existence.
Rcm business earlier started as a clothing company known as “Fashion Suiting Pvt Ltd.” Which was establish in Rajasthan by the Chhabra Group in 1977. Further after some time Sh. Trilok Chand Chhabra realize that customers are getting exploited by the intermediators like selling agency, promotion cost, wholesalers and retailers.

Due to which product’s price rise and customer get the product at a high price. To solve this problem, Sh. Trilok Chand Ji (Owner and founder of Rcm business) started a direct selling system and reforms his existing clothing company to Rcm business group which is based up on direct selling product multi-level marketing method. He started Rcm business plan in 2000.
Now the Rcm come under top 10 direct selling multi-level marketing companies of India. Today Rcm is manufacturing around 730 products, having 8 million distributors and 1000 Pickup Centre all over the India.
Rcm Business currently manufacturing almost all types of products like health supplements and herbal medicines, food and grocery, clothing for children, women and men as well as a wide array of other stuff such as bags, stationery, tools and many more. This is all about the Rcm business, one should know before he or she join Rcm marketing plan 2021.
Additional Read : Check Business in Rcm Business
Then how to join the Rcm business and what are the benefits of Rcm business plan 2021 are already mentioned in the above topic. Hope you get that easily. Now let’s move further in the article Rcm business plan 2021.
Why Rcm Business is Important?
Guys earlier in Indian market, normal selling method is followed, where the final customers get exploited by the intermediators like selling agency, wholesaler, retailers. Looking for the welfare of society and for the benefits of the customers Sh. Trilok Chand Ji (owner and founder of Rcm business) transform their existing clothing company into Rcm business group owned by Trilok Chand Chhabra Ji at that time.
The motive of Rcm business was to start direct selling method in Indian Market. So, that the final customers need not to pay for wasteful expense like for product promotion, wholesaler’s and retailer’s profits and profit of selling agencies.
They add their profits to the product cost, as result low-cost products are provided to the final customers in a high cost. Why it is so? Let’s know its answer with the following example:
A XYZ company manufacture a product, whose manufacturing cost amounts up to Rs. 100. After that, when a company launch that product in the market, they need to do product promotion which amounts up to Rs. 50. After that product goes to the selling agency which add their profit.
Let’s assume they add Rs. 20 as their profit in the product cost. Now the product goes to wholesaler and then he will add his profit up to Rs. 20 and after that product goes to the retailer and he will also add his profit up to Rs. 10. After add all these cost the product reaches to the final customer.
Now product price which will customer need to pay for that product amounts Rs. 200 (Rs. 100 for manufacturing cost and company profit + Rs. 50 for product promotion + Rs. 20 as selling agency profit + Rs. 20 as wholesaler profit + Rs. 10 as retailer profit).
Guys, this is the big disadvantage of regular system which is followed by our Indian market. Rs. 100 amounting product is provided to the final customer in Rs. 200. You can easily see the drawback of this system.
Whereas on other hand is direct selling method is here under Rcm business plan. That’s the reason Trilok Chand Ji start a product based direct selling company, which is now manufacturing all kinds of products and providing them at a reasonable cost by eliminating the extra cost like product promotion cost, profits of selling agencies, wholesalers and retailers.
That’s why Rcm business is important for us. Rcm provides us all the product at a reasonable price with 100% purity. Rcm business plan or Rcm marketing plan 2021 also allow you to make some money by purchasing Rcm products, also it provides 3 types of other income like performance bonus, royalty bonus and technical bonus.
Additional Read : Online Shopping in Rcm Business
Friends, hope you now understood that why Rcm business plan is important for us. Now let’s discuss our next topic in the article of Rcm business plan.
Why Do Rcm Business?
Guys, to know the answer of this question, first you should know what is Rcm business and what is the benefits of Rcm business plan. So, as discussed earlier Rcm business is a product based direct selling multi-level marketing company of India, which comes in top 10 list of direct selling MLM companies of India.
So, the answer for the question that why do Rcm business is Rcm provides us number of benefits like it provide us performance bonus, royalty bonus and technical bonus when you buy Rcm products and sell them to other customers and make others as Rcm business plan consultants under your downline. Let’s study about the Rcm business benefits in detail. Following are the benefits of Rcm business plan.
100% Pure Products: Rcm business provide you 100% pure products. Unlike to all other product available in the market which are adulterated and of low quality, Rcm provide you 100% pure and good quality products.
Retail Profit: One of the main benefits of Rcm Business plan 2021. You can buy the product from the Rcm pick up point at a discount rate up to 10-20% and then sell these products at M.R.P to other customers. In this way you earn profit which is known as retail profit.
Discount up to 10-20%: Under Rcm business plan 2021, you get the Rcm products at a discounted rate from the M.R.P. You get 10 to 20% of discount rate depending upon your BV (business volume).
Performance Bonus (up to 32%): Every product that you buy from the Rcm has BV points. BV stands for Business Volume. Yours and your groups BV points are added together in the end of the month and the commission is given to you as a performance bonus up to 32% depending up on your BV points. Further you have to distribute this commission with your group.
Royalty Bonus (up to 8%): Royalty Bonus is given up to 8% on the basis of your business volume points. Royalty Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021. Royalty is given on the basis of difference by deducting downline royalty from the total royalty. Royalty always calculated on monthly basis.
Technical Bonus (up to 5%): Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Also, he or she should be successfully earning the royalty income up to 8% percent for consecutive 3 months. Technical bonus is given on the basis of difference by deducting downline technical bonus from the total technical bonus.
How to do Rcm Business?
Guys, might you be now thinking that how you can take advantage of Rcm marketing plan 2021. So, we are here to tell you that how to do Rcm business to take earn the income under the Rcm marketing plan 2021.
First you need to join the Rcm marketing plan 2021. So, to join Rcm business go to its official website and fill the form to become a direct seller. In the direct seller form you will fill have to enter first sponsor number then proposer number and then some personal details, bank details and security details.
After that submit your form after uploading all the necessary documents. Once you join Rcm marketing plan then you need to buy minimum 1000 rupees Rcm products. Then in next step you need to sell these products to others through which you can also earn retail profit also.
After that you have to make your own group. You have to add other people on your downline. You have to convince other people to join the Rcm marketing plan 2021 under you.
That’s all you need to do to earn under Rcm marketing plan in Rcm business. You need to be patience because to earn under Rcm business plan and earn commission.
How Does Rcm business make Money?
Guys, under Rcm marketing plan 2021 you can earn multiple income. You can make money in Rcm business in the form of Retail profit, because once you join the Rcm business you get Rcm products at a discounted price and then you can sell these products to other people at M.P.R price and earn retail profit.
Another way to make money in Rcm business is earning commission in the form of Performance bonus. You get up to 32% of performance bonus depending upon your BV. BV stands for business volume.
You also get commission in the form of Royalty. You get royalty bonus up to 8% depending upon your BV. Royalty Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Another commission which is given to you is Technical Bonus. Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Types of Income in Rcm Business?
Now guys, in this topic under Rcm business plan article, we will discuss about the income that you can earn under Rcm marketing plan 2021. Below listed are the types of income in Rcm business. Let’s understand these incomes in detail:
– Performance Income
BV stands for Business Volume. Every product that you buy from the Rcm has BV points. Yours and your groups BV points are added together in the end of the month and the commission is given to you as a performance bonus up to 32% depending up on your BV points. Further you have to distribute this commission with your group.
– Royalty Income
– technical income.
Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021. Also, he or she should be successfully earning the royalty income up to 8% percent for consecutive 3 months.
Technical bonus is given on the basis of difference by deducting downline technical bonus from the total technical bonus. Technical bonus is always calculated on monthly basis.
Rcm Business Slab Chart
Friends for you, we have given the chart slab of the incomes under the Rcm business plan or Rcm marketing plan 2021. From the following chart you can easily understood the percentage of commission you will get under different heads of Income depending upon your BV. Let’s have a look on the following chart slab of Rcm marketing plan 2021 incomes.
Performance Bonus Slab Chart :
Royalty Bonus Slab Chart :
Technical Bonus Slab Chart :
What to do in Rcm Business After Joining?
Guys, once you join Rcm marketing plan then you need to buy minimum 1000 rupees Rcm products. Then in next step you need to sell these products to others through which you can also earn retail profit also.
Bapon Das is the CEO (Chief Executive Officer) of Jayrcm. He is a YouTuber, Businessman, Trainer, Speaker and Developer. Bapon Das is famous on YouTube for Rcm Business Strategy. Bapon Das is helping People across the India in achieving their Rcm Business Goals.
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
RCM Business Process Transformation 2021 RadarView™
$ 1,995.00
- Description
The report helps enterprises identify key service providers to digitally transform their revenue cycle management (RCM) operations. It begins with a summary of key trends that are shaping the RCM space. We continue with a detailed assessment of 19 providers offering services in the RCM outsourcing domain. Each profile provides an overview of the service provider, their key IP assets for RCM, and a list of clients and partnerships, along with brief client case studies. Each profile concludes with analyst insights on the provider’s practice maturity, domain ecosystem, and investments and innovations.
Why read this RadarView?
Many healthcare providers are looking for end-to-end digital transformation of their RCM function. The demand for comprehensive engagements in the RCM domain is increasing, minimizing siloes between IT and business processes. Amid COVID-19, the significance of disruptive technologies in transforming the RCM function has emerged more than ever before. Many executives are striving to outsource the strategic and judgement-intensive RCM domain, as opposed to only transaction-intensive RCM operations.
The RCM Business Process Transformation 2021 RadarView highlights the key outsourcing trends in the RCM space and Avasant’s viewpoint on them. It aids companies in identifying top service providers to assist them in transforming their RCM operations. It also offers an analysis of each service providers’ capabilities in technology, domain expertise, and delivery-related support, thus enabling healthcare organizations to identify the right strategic partners for their RCM transformation.

Featured providers
This RadarView includes a detailed analysis of the following RCM service providers: Access Healthcare, AGS Health, Atos, Ciox, Cognizant, Conifer, Corrohealth, Ensemble Health, Exela Technologies, GeBBS, Genpact, HGS, IKS Health, nThrive, Omega Healthcare, Optum, R1 RCM, Sutherland, and Wipro.
Methodology
The industry insights and recommendations are based on our ongoing interactions with enterprise CXOs and other key executives; targeted discussions with service providers, subject matter experts, and Avasant Fellows, along with lessons learned from consulting engagements.
Our evaluation of service providers is based on primary input from the providers, focused briefings, public disclosures, validation from their clients, and our ongoing market interactions. The assessment is across the three dimensions of practice maturity, domain ecosystem, and investments and innovation, leading to our recognition of those service providers that have brought the most value to the market over the last 12 months.
Table of contents
About the report (page 3)
Executive summary (pages 5-7):
- Key RCM outsourcing trends shaping the market
- Avasant RCM Business Process Transformation 2021 RadarView
RCM business process transformation market trends (pages 8-22):
- Impact of COVID-19 on RCM
- Growth of RCM outsourcing
- Evolution of patients’ expectation and rise of healthcare consumerism
- Initiative taken by healthcare providers
- Effect of price transparency regulations on RCM
- Rise of digital operations
- Adoption of RPA, AI, ML, analytics, and workflow solutions across RCM value chain
- Development of partnership ecosystem
- Consolidation among RCM service providers
- Influence of interoperability regulations on RCM operations
RadarView overview (pages 23-25):
- Assessment dimensions
- Research methodology and coverage
- RCM Business Process Transformation 2021 RadarView (pages 26-28):
- Reading the RadarView
- RadarView assessment
Service provider profiles (pages 29-67):
- Detailed profiles for Access Healthcare, AGS Health, Atos, Ciox, Cognizant, Conifer, Corrohealth, Ensemble Health, Exela Technologies, GeBBS, Genpact, HGS, IKS Health, nThrive, Omega Healthcare, Optum, R1 RCM, Sutherland, and Wipro.
Read the Research Byte based on this report.
Related Reports

Digitization to Improve Patient Convenience and Drive Profitability

RCM Business Process Transformation 2023 Market Insights™

RCM Business Process Transformation 2023 RadarView™

RCM Service Providers Help Healthcare Providers Overcome Challenges in Revenue Cycle Management
Disclaimer:.
Avasant's research and other publications are based on information from the best available sources and Avasant's independent assessment and analysis at the time of publication. Avasant takes no responsibility and assumes no liability for any error/omission or the accuracy of information contained in its research publications. Avasant does not endorse any provider, product or service described in its RadarView™ publications or any other research publications that it makes available to its users, and does not advise users to select only those providers recognized in these publications. Avasant disclaims all warranties, expressed or implied, including any warranties of merchantability or fitness for a particular purpose. None of the graphics, descriptions, research, excerpts, samples or any other content provided in the report(s) or any of its research publications may be reprinted, reproduced, redistributed or used for any external commercial purpose without prior permission from Avasant, LLC. All rights are reserved by Avasant, LLC.
Login to get free content each month and build your personal library at Avasant.com
New To Avasant ?
- Report Store
- AMR in News
- Press Releases
- Request for Consulting
- Our Clients

Revenue Cycle Management Market Size, Share, Competitive Landscape and Trend Analysis Report, by Type, by Component, by Deployment Mode, by End-User : Global Opportunity Analysis and Industry Forecast, 2022-2031
IC : Software and Services
Report Code: A01852
Tables: 148
Get Sample to Email
Thank You For Your Response !
Our Executive will get back to you soon
Revenue Cycle Management Market Statistics: 2031
The global revenue cycle management market was valued at $109.5 billion in 2021, and is projected to reach $367.7 billion by 2031, growing at a CAGR of 13.2% from 2022 to 2031.
The supportive growth through regulatory compliance has increased the need for revenue cycle management. In addition, the growing demand for workflow optimization in healthcare organizations coupled with innovative synchronized management software systems is benefiting the growth of the revenue cycle management market. Furthermore, the rise in demand for cloud-based solutions factor notably promotes the growth of revenue cycle management market. However, high costs associated with RCM deployment, and the scarcity of trained professionals are the issues that are limiting the industry expansion. On the contrary, the increasing outsourcing services in developing countries are expected to create lucrative opportunities for the market in the upcoming years. Moreover, a rise in developments & initiatives toward revenue cycle management is anticipated to provide a potential growth opportunity for the market.
Revenue cycle management (RCM) is the process used to track the revenue from patients, from their initial appointment or encounter with the healthcare system to their final payment of the balance. This process helps streamline the business operations of healthcare organizations and private practices. RCM solutions help providers manage and enhance revenue cycle functions such as medical coding & billing, patient insurance eligibility verification, electronic health records, clinical documentation, and claims & denials management.
The revenue cycle management market is segmented into End-User, Deployment Mode, Type and Component.
Segment Review
The revenue cycle management market is segmented into type, component, deployment mode, end user, and region. By type, the market is differentiated into standalone and integrated. By component, the market is segmented into software and services. Depending on deployment mode, it is fragmented into cloud and on-premise. Depending on end user, it is segmented into hospitals, physicians, diagnostic laboratories, and others. Region-wise, the market is analyzed across North America, Europe, Asia-Pacific, and LAMEA.
The services segment is anticipated to grow at a significant rate due to rise in professional and managed services for smooth operations of RCM Software .
By Component, the software segment acquired a major share in the revenue cycle management industry in 2021. This is attributed to the wide adoption of the RCM software to avoid healthcare fraud and decrease administrative costs. However, the services segment is anticipated to register the highest growth rate during the forecast period due to the rise in cloud based RCM and increased demand for professional services.
The revenue cycle management market was dominated by North America in 2021, owing to presence of key players in the region.
Region wise, North America dominated the market in revenue cycle management market size in 2021 due to the presence of key players and surge in demand for IT solutions in the healthcare sector. However, Asia-Pacific is anticipated to register the highest growth rate in the revenue cycle management market forecast due to the rise in healthcare spending and technological advancements in the healthcare sector.
Country Specific Statistics & Information
The growing number of multiple data siloes and unorganized workflows in healthcare settings is paving a path for market development and growth. RCM is a combination of third-party payers, payment models, guidelines, and codes. A practice’s existence depends upon obtaining the right assets. As precise payment for medical services becomes increasingly complex, it increases the value of obtaining an efficient RCM solution. These are some of the trends flourishing the market growth. For instance, in May 2022, Cerner, a leading supplier of healthcare information technology solutions and tech-enabled services aimed to help members achieve revenue cycle automation by providing access to an artificial intelligence (AI)-driven platform through a collaboration with AKASA. The partnership allows Cerner customers to use AKASA’s AI-based Unified Automation platform to automate revenue cycle tasks. In addition, the platform automates authorization tasks, including identifying authorization requirements, initiating requests, checking statuses, and notifying payers of inpatient admissions. The system also assists in claims processing. Providers can use the platform to receive status information for outstanding claims and make any corrections needed before submitting claims to clearinghouses and payers.
Furthermore, the introduction of new and innovative products in the market by key players is expected to boost the growth of the revenue cycle management market during the forecast period. For instance, Veradigm, a leading provider of healthcare data and technology solutions and a business unit of Allscripts Healthcare Solutions, has launched its Veradigm Payerpath. Veradigm Payerpath is an end-to-end revenue cycle management suite of solutions built to assist medical practices of all sizes and specialties improve revenue, streamline communications with payers and patients, and boost practice profitability. The system’s integrated solutions are practice management (PM) agnostic, interfacing seamlessly with all major PM systems. An innovative claims management platform, Veradigm Payerpath delivers a more than 98% first-pass clean claims rate and reaches a network of over 3,100 payers.
COVID-19 pandemic had an unprecedented impact on the majority of the healthcare sectors and brought significant transformations to the normal functioning of healthcare systems. Healthcare providers and healthcare payers struggled through several challenges impacting their revenue earnings and inpatient volume. Furthermore, medical billing complexity and rising healthcare costs created a drastic rise in demand for outsourcing revenue cycle management solutions across the globe. The surge in demand for advanced and innovative RCM solutions drove key participants to develop value-added features such as payer connect, remote coding services, reporting, analytics, and audit and compliance to improve revenue generation and productivity. This, in turn, has become one of the major factors for the revenue cycle management market growth during the global health crisis.
Top Impacting Factors
Favorable government regulations.
The healthcare industry has undergone multiple changes regarding regulatory framework in order to protect patient data and ensure there is a smooth flow of claims management. Health Insurance Portability and Accountability Act of 1996 (HIPAA) is one such regulation that protects electronic protected health information (e-PHI) in order to shield health information privacy rights. Through this act, confidentiality, integrity, and availability of e-PHI are maintained. In addition, there are coding and compliance models such as Current Procedural Terminology codes (CPT), International Classification of Diseases diagnosis codes (ICD), and the Healthcare Common Procedure Coding System (HCPCS). These codes are deployed to integrate the whole healthcare and the insurance industry on one platform.
Furthermore, there are other government mandates such as Affordable Care Act (ACA) 2010 which is also called the ObamaCare and Health Information Technology for Economic and Clinical Health (HITECH) Act. These acts were implemented to improve the quality of healthcare and insurance services at affordable costs and promote the growth of the healthcare IT sector. All these factors collectively drive the growth of the revenue cycle management industry.
Increase in Healthcare Spending
The healthcare sector has witnessed an upsurge in healthcare-related expenditure in the recent past, and this trend is expected to prevail during the forecast period. The healthcare spending growth rate is attributed to the rise in medical prices, growth associated with the insured population, and an increase in demand for advanced healthcare services. In addition, the major factor that contributes to the growth of revenue cycle management in Europe includes, a rise in healthcare expenditure among countries, such as Germany, France, Sweden, UK, and others in this region. Furthermore, high spending patterns of hospitals and physicians among the developing nations of Asia-Pacific and LAMEA are expected to fuel the demand for revenue cycle management.
Rise in the Market for Outsourced RCM Solutions
Healthcare providers have been experiencing problems related to increasing overhead costs, slow growth associated with operating revenues, maintaining profits, denial management, and delay in claims processing. These challenges go hand in hand with the outsourcing of the RCM model from third-party organizations. Additionally, the maintenance of regulatory compliance, reduction in billing errors, improved accuracy over co-pay data, integration with respect to ICD-10 coding requirements, improved service quality, and cost-effectiveness are some of the factors that are expected to create lucrative opportunities for outsourced RCM market growth.
For instance, in October 2019, QuickCred, the credentialing division of MedTrainer, Inc., announced its partnership with athenahealth, the leading provider of network-enabled services for electronic health records (EHR), medical billing, and care coordination. The collaboration enables medical practices to take advantage of QuickCred’s state-of-the-art compliance and credentialing system while optimizing revenue cycle management through athenahealth.
Key Benefits for Stakeholders:
- This report provides a quantitative analysis of the market segments, current trends, estimations, and dynamics of the revenue cycle management market analysis from 2021 to 2031 to identify the prevailing revenue cycle management market share.
- The market research is offered along with information related to key drivers, restraints, and opportunities.
- Porter's five forces analysis highlights the potency of buyers and suppliers to enable stakeholders make profit-oriented business decisions and strengthen their supplier-buyer network.
- In-depth analysis of the revenue cycle management market size segmentation assists to determine the prevailing revenue cycle management market opportunity.
- Major countries in each region are mapped according to their revenue contribution to the global market.
- Market player positioning facilitates benchmarking and provides a clear understanding of the present position of the market players.
- The report includes the analysis of the regional as well as global revenue cycle management market trends, key players, market segments, application areas, and market growth strategies.
Revenue Cycle Management Market Report Highlights
| USD 367.7 billion | |
| CAGR of 13.2% | |
| 2021 - 2031 | |
| 271 | |
| (U.S., Canada) (UK, Germany, France, Italy, Spain, Rest of Europe) (China, Japan, India, Australia, South Korea, Rest of Asia-Pacific) (Latin America, Middle East, Africa) | |
| Quest Diagnostics Incorporated, Epic Systems Corporation, GeBBS Healthcare Solutions, Experian Information Solutions, Inc., eClinicalWorks, Veradigm LLC, Oracle Cerner, McKesson Corporation, GE HealthCare, Athenahealth, Inc. |
Analyst Review
In accordance with insights from leading CXOs, the utilization of RCM among healthcare facilities has increased due to reduced product cycle time. Moreover, supportive growth through regulatory compliance, increasing healthcare spending, growing demand for cloud-based solutions, and increasing market for outsourced RCM solutions drive the growth of the market. In addition, recent innovations and increase in the adoption of advanced healthcare systems have further fueled the market growth. For instance, in May 2021, Bassett Healthcare Network collaborated with Optum, Inc. for revenue cycle management to improve patient care in Central New York.
The market for revenue cycle management is witnessing a rise, owing to rise in the market for outsourced RCM solutions. Healthcare facilities are outsourcing revenue cycle management software solutions owing to the multiple advantages associated such as easy availability of trained and skilled professionals, compliance and adherence to required regulations, enhanced efficiency, and cost-effectiveness.
Due to the numerous benefits, available healthcare facilities are readily outsourcing RCM solutions and services. According to a Med USA article published in 2020, approximately two-thirds of the healthcare organizations outsource their revenue cycle management solutions and services. The growing adoption rates are anticipated to propel market growth over the forthcoming years.
The COVID-19 pandemic enforced governments to impose lockdowns and travel restrictions which caused inconsistency in patient volume and uncertainties in claim volumes. The rising complexities in RCM positively impacted the outsourcing of RCM solutions. Furthermore, the rising claim denials, constantly changing COVID-19 policies, and the development of new codes led to increased pressure on RCM professionals and staff, which positively impacted the growth of the market during the pandemic.
In addition, the transition of healthcare systems toward value-based care and the adoption of virtual engagement technologies such as telehealth is anticipated to pave the way for lucrative opportunities for the revenue management cycle, thereby accelerating revenue growth.
- Business Intelligence Solutions
- Resource Management Software
- Digital Payment Software And Services
- Process Automation Software And Services
The global revenue cycle management market was valued at $109.53 billion in 2021, and is projected to reach $367.71 billion by 2031, registering a CAGR of 13.2% from 2022 to 2031.
North America is the largest region for revenue cycle management market.
Revenue cycle management market is driven by the supportive growth through regulatory compliance, and increase in healthcare spending. In addition, rise in demand for cloud-based solutions fosters the growth of the revenue cycle management market.
The key players operating in the global revenue cycle management market include Athenahealth, Inc., eClinicalWorks, Epic Systems Corporation, Experian Information Solutions, Inc., GeBBS Healthcare Solutions, GE HealthCare, McKesson Corporation, Oracle Cerner, Quest Diagnostics Incorporated, and Veradigm LLC.
The key growth strategies include product portfolio expansion, acquisition, partnership, merger, and collaboration.
Loading Table Of Content...
Loading Research Methodology...
- Related Report
- Global Report
- Regional Report
- Country Report
Enter Valid Email ID
Verification code has been sent to your email ID
By continuing, you agree to Allied Market Research Terms of Use and Privacy Policy
Advantages Of Our Secure Login

Easily Track Orders, Hassel free Access, Downloads

Get Relevent Alerts and Recommendation

Wishlist, Coupons & Manage your Subscription

Have a Referral Code?
Enter Valid Referral Code
An Email Verification Code has been sent to your email address!
Please check your inbox and, if you don't find it there, also look in your junk folder.
Revenue Cycle Management Market
Global Opportunity Analysis and Industry Forecast, 2022-2031
- Contact Us

- Channels ►
- Executive Moves
- Transaction & Valuation
- Health Equity
- Patient Experience
- Care Coordination
- Legal & Regulatory
- Compensation
- Specialties ►
- Orthopedics
- Surgery Centers
- Dental / DSO
- Becker's Healthcare Websites ►
- Dental + DSO
- Behavioral Health
- Physician Leadership
- Newsletters ►
- Sign Up For Our Free E-Newsletters
- Hospital Review
- Hospital CEO Report
- Hospital CFO Report
- Health IT & CIO Report
- Clinical Leadership
- Revenue Cycle Management
- Digital Innovation Report
- Supply Chain
- Payer Issues
- Pharmacy Report
- Women's Leadership
- Laboratory Review
- Cardiology Report
- Oncology Report
- HR + Talent Review
- Post Acute Report
- Life Sciences Report
- Behavioral Health Report
- Marketing Report
- Events ►
- Upcoming Conferences and Events
- 9th Annual Health IT + Digital Health + RCM Annual Meeting: The Future of Business and Clinical Technologies
- Becker's ASC 30th Annual Meeting: The Business and Operations of ASCs
- Fall Future of Dentistry Roundtable
- Fall Payer Issues Roundtable
- 12th Annual CEO + CFO Roundtable
- Chief Pharmacy Officer Summit
- 15th Annual Meeting
- Spring Payer Issues Roundtable
- Bold Ideas + Big Takeaways from Becker's 14th Annual Meeting
- Exhibiting & Sponsoring
- Call for Speakers
- Virtual Events ►
- Upcoming Virtual Events
- Transform Hospital Operations Virtual Summit
- Infusion Center Operations Virtual Summit
- Oncology Virtual Forum
- AI + Digital Health Virtual Event
- Digital Innovation + Patient Experience and Marketing Virtual Event
- Dental + DSO Virtual Event
- Human Resources + Talent Virtual Event
- 9th Annual Health IT + Digital Health + RCM Virtual Event
- 12th Annual CEO + CFO Roundtable Virtual Event
- Oncology Virtual Summit
- Past Virtual Events
- Webinars ►
- Upcoming Webinars
- OnDemand Webinars
- Partner Content ►
- Current Partner Content
- Podcasts ►
- Our Podcasts
- Becker's Healthcare Podcast Episodes
- Becker’s Digital Health + Health IT Podcast
- Becker’s Payer Issues Podcast
- Podcast Summaries
- Becker's Behavioral Health Podcast
- Becker's Ambulatory Surgery Centers Podcast
- Becker's Spine and Orthopedics Podcast
- Becker's Dental + DSO Review Podcast
- Becker’s Clinical Leadership Podcast
- Becker’s Pediatric Leadership Podcast
- Becker's Cardiology + Heart Surgery Podcast
- Becker's Women's Leadership Podcast
- Lists ►
- 100 great community hospitals | 2024
- Great leaders in healthcare | 2024
- Nominations
- Sign up for list nomination updates
- Print ►
- Current Issue
- Past Issues
- Current Issue - Becker's Clinical Leadership
- Past Issues - Becker's Clinical Leadership
- Multimedia ►
- Intuitive + Becker's Content Hub
- NRC Health Content Hub
- Now is the Time
- LeanTaaS AI Solutions
- Healthcare Upside/Down Podcast Series
- Featured Content
- Career Center
- Mass General Brigham
- AMN Healthcare
- 2024 Trends: Key Challenges for Healthcare CFO’s
- Insights ►
- Spine Surgeon
- About Us ►
- About Becker's Hospital Review
- Careers at Becker's
- Request Media Kit
- Content Specifications
- Most Read ►
- Boom times for HCA
- CMS drops 4 final payment rules for 2025: 16 things to know
- 'This is dire': Texas systems face losing their health plans
- CMS sets 2.9% inpatient pay bump for hospitals in 2025: 6 things to know
- HCA slashes contract labor costs by 25.7%
- HCA executives sell nearly $4M in stock
- Judge OKs Steward to close 2 Massachusetts hospitals
- Massachusetts to give Steward $30M to keep hospitals running
- Pressure builds for HCA to relinquish ownership Mission Health
- How HCA, Tenet, CHS and UHS performed in Q2
- Top 40 Articles ►
- 100 great hospitals in America | 2019
- 61 health systems with strong finances
- Ascension reorganizes hospital portfolio: 10 transactions to know
- 16 hospital closures in 2024
- UPMC to lay off around 1,000 employees
- From -6.8% to 12.2%: 43 health systems ranked by operating margins
- As Steward's finances stumble, spotlight turns to CEO's yachts
- Emory Georgia hospital to close by end of year
- 418 rural hospitals at risk of closure, breakdown by state
- Steward plans sale of all hospitals, reports $9B in debt
- 17 health systems dropping Medicare Advantage plans | 2024
- 15 health systems with strong finances
- Steward files for bankruptcy
- 43 health systems ranked by net income
- Rush lays off admin, leadership staff
- Walmart Health to close all 51 health clinics, virtual care
- Texas hospital to close, lay off 94
- Biden's $7.3 trillion budget: 16 healthcare takeaways
- Louisiana hospital closes after licenses revoked
- Tennessee hospital to close March 9
- University Hospitals to cut 300+ jobs, including some VP, C-suite roles
- 20 hospitals, systems where charity care exceeds tax breaks
- Tufts Medicine to lay off 174 employees, including leaders
- California hospital to lose Medicare contract
- 'A crisis of your creating': UnitedHealth CEO grilled by Congress on cyberattack
- 2 Nebraska hospitals abruptly close, 72 laid off
- Nearly half of health systems are considering dropping Medicare Advantage plans
- A leading money loser for hospitals: Kaufman Hall
- Jackson Health lays off hospital CEO, staff amid financial woes
- CHS' highest-earning executives in 2023
- Hospital expenses per inpatient day across 50 states
- Optum laying off 129, closing Ohio facility
- Steward looks to transfer all 9 Massachusetts hospitals amid lawmaker backlash
- Closed New York hospital up for auction
- Hospitals' Medicare Advantage problem hits an inflection point
- Steward to sell 'highly desired' physician group to Optum
- Kaiser laying off 76 in California
- CommonSpirit takes 'firm stance' with payers
- 12 hospitals closing departments or ending services
- Texas hospital struggling to make payroll at risk of closure

Financial Management
6 key rcm company business moves in 2021.
From mergers to acquisitions to new leaders, here are six key moves healthcare revenue cycle management companies made in 2021:
- Gulf Capital acquired two RCM firms for $60 million. The Abu Dhabi-based asset management firm bought Eclat Health Solutions in Herndon, Va., and Hansei Solutions in Los Angeles.
- Two healthcare RCM companies merged : Charlotte, N.C.-based Meduit and Moline, Ill.-based Avadyne Health.
- Chicago-based healthcare RCM company R1 RCM acquired patient financial engagement company VisitPay for $300 million.
- Zotec Partners, a Carmel, Ind.-based RCM company for healthcare providers, added three new leadership positions: chief operating officer, chief product officer and client success officer.
- Baptist Health South Florida ended its RCM agreement with Health System Solutions and will move about 600 employees in-house. The Coral Gables-based health system formed Health System Solutions in 2018 as a joint venture designed to offer RCM services to healthcare providers.
- Renton, Wash.-based Providence's health tech investment portfolio Tegria acquired Colburn Hill Group, a company that uses robotic process automation for healthcare RCM.
Copyright © 2024 Becker's Healthcare. All Rights Reserved. Privacy Policy . Cookie Policy . Linking and Reprinting Policy .
Featured Learning Opportunities
- Whitepapers
- Finance Whitepapers
- Process Improvement Whitepapers
- Health IT Whitepapers
- Clinical Whitepapers
- Payer Whitepapers
- Other Learning Opportunities
- Finance Webinars
- Process Improvement Webinars
- Health IT Webinars
- Clinical Webinars
- Payer Webinars
- Virtual Events
- ASC/Spine Whitepapers
- Dental Whitepapers
- ASC/Spine Webinars
- Dental Webinars
- Hospital Review Virtual Events
- ASC/Spine Virtual Events
- Dental Virtual Events
Featured Whitepapers
Featured webinars.
Becker's Websites
Virtual Learning
Conferences
- 9th Annual Health IT + Digital Health + RCM Meeting: The Future of Business and Clinical Technologies
- 1.800.417.2035
- [email protected]
Get A Free Revenue Cycle Management Assessment
Register Now

Plutus Health Logo
AI in Revenue Cycle Management: How It Improves RCM, Efficiency and Revenue
Thomas John has 30+ years of experience in healthcare RCM and IT. He is the founder and CEO of Plutus Health Inc., one of the biggest healthcare RCM companies in the US. Thomas has comprehensive knowledge of AI-driven practice management and billing software. He believes in providing an end-to-end solution for revenue cycle and practice management.

Artificial Intelligence has the potential to significantly impact the field of Revenue Cycle Management in the US healthcare industry. This article explores how to implement AI in RCM, overcome obstacles, and build a business case for it.
In this blog:
- The benefits of AI in RCM
- How to apply AI to RCM tasks
- Overcoming barriers to implementing AI
- How to build the business case for AI in RCM

How Artificial Intelligence is Optimizing Healthcare Revenue Cycle Management
AI optimizes healthcare RCM in many ways: accuracy and efficiency. Artificial intelligence can perform tasks at lightning speed and with minimal or no errors. This leaves the staff more time for tasks requiring critical thinking and personal attention.
Why is AI Important in Healthcare Revenue Cycle Management?
AI has the potential to revolutionize RCM in the U.S. healthcare industry by streamlining processes, reducing costs, increasing accuracy, and improving both profitability and patient satisfaction. Overall, healthcare companies can compete better in the market.
Benefits of AI in Revenue Cycle Management
The benefits of AI in RCM include improved efficiency, accuracy, patient experience and team satisfaction. In addition, employees can rely on artificial intelligence to simplify time-consuming tasks and focus more on critical thinking and troubleshooting.
Here’s a detailed list of the benefits of RCM AI:
- Improved accuracy: AI software can improve accuracy throughout the revenue cycle management process. AI greatly increases the accuracy of all patient and claims information . It also increases the accuracy of bills. This decreases the need for staff time to deal with follow-up questions and delays from the payer.

One good example comes from Celeste Daye, Vice President of revenue management for New York-based Concerto Care, which offers in-home care programs for seniors. She points out how simple AI processes helped medical organizations during COVID-19 when the federal government required them to input information to allow federal reimbursement for COVID testing.
"There was a pretty arduous process of registering patients into that system. And it was just entering their demographic information," Daye says. "Most hospitals wanted to get that information in as quickly as possible – to get the revenue."
"You can deploy those (staff) resources to touching more of the accounts that require critical thinking – that require a conversation with a payer or a formal appeal that would yield the organization money," says Daye. "Otherwise, (that account) may not be touched, or you may be paying a higher dollar amount on that same payment. Because you’ve had to use someone else because you just don’t have the internal resources to touch everything."
- Better claims management: AI improves and streamlines all aspects of claim management and submission. It helps an organization review many more upcoming claims to check for accuracy and significantly improves how it reviews them. That means organizations can submit accurate claims more quickly.
- Fewer denied claims: AI allows organizations to assess and identify possible problem claims before they happen. Becker’s Hospital CFO Report estimated in 2019 that hospitals lose more than $260 billion each year in insurance denials. AI “machine learning” — a type of AI — can significantly decrease the number of denials by analyzing data from past rejected claims. In addition, it can help organizations fix issues with certain claim types to ensure approval.
Jereen Mathew, an RCM consultant with years of experience in the industry, says the increased revenue can be put into two categories: "faster revenue" and "better revenue."
- Improved patient experience and satisfaction: As AI improves many RCM processes, it can also improve the patient experience. It can automatically and immediately identify patients eligible for financial assistance. In addition, it can help the organization more easily provide price transparency for services.
- Improved scalability: AI allows medical organizations to expand the number of accounts their RCM workflow processes can manage. Organizations wanting to increase the accounts they manage by tens of thousands or hundreds of thousands would otherwise need to hire significant staff. With AI assistance, it can require only more computer processing power.
- Improved predictive analytics: AI algorithms can analyze large volumes of historical claims data and identify patterns that lead to claim denials. By using predictive analytics, AI can help healthcare organizations proactively address potential issues, optimize claim submissions, and improve reimbursement rates.
- Revenue forecasting and financial analytics: AI systems can analyze historical revenue data and other relevant factors to forecast future revenue trends accurately. This can help healthcare organizations make informed financial decisions and optimize their revenue streams.
- Better assessment of RCM performance: AI can analyze huge amounts of data — including on claims, payments and denials — to give organizations insights into their RCM process. Those insights can help organizational staff and revenue cycle analysts improve their processes and RCM strategies to increase revenue.
"There are many people that would prefer to do work that they feel is more thought-provoking," Daye says. "And being able to ask your teams to help identify places where we can automate … and then we use that information, it’s a success that you can share with them."
- Eligibility and benefits verification: The most common use of AI in healthcare RCM is in eligibility and benefits verification. It can help organizations automatically verify a patient’s eligibility long before any claims are submitted. Companies working with the most advanced AI are exploring whether they can use chatbots and similar technologies to communicate with insurance companies directly. For example, chatbots might provide updated patient information that insurance companies may need to determine eligibility. By utilizing machine learning algorithms, AI systems can learn from historical data to improve accuracy and efficiency, reducing the need for manual intervention.
- Patient scheduling: AI allows an organization to schedule patients optimally – using the right providers credentialed for the appropriate insurance companies. It helps organizations ensure their providers are serving the most allowable patients per day.
- Pre-billing audits: Healthcare organizations use pre-billing audits to sample claims and determine whether the RCM process is producing fully accurate claims that payers can immediately approve. AI can replace humans doing these audits. It can automatically check the accuracy of all needed information. Those audits help organizations improve any RCM processes to increase the percentage of approved claims.
- Prior authorization: The most advanced AI and machine learning are helping healthcare organizations get required prior authorization from insurance companies to approve a needed healthcare service for a patient. The AI is aiding the RCM process in determining what added information insurance companies need, and then transferring that information to them.
- Patient payment/timing estimation: AI helps healthcare organizations estimate service costs and due dates for patients. That process requires, among other things, getting information from insurance companies. AI enables that process to be automatic and quick.
- Denials management: AI can help organizations decrease payer denials through more accurate claims. It can also help organizations respond more quickly with information to appeal the denials. And it can help organizations look at historical data on denied claims to determine common reasons and make appropriate fixes before filing the claim.
- Compliance monitoring: AI can ensure that all claims comply with Medicare, Medicaid, and other governmental rules and regulations.
- Charge capture: AI can help medical organizations ensure that all appropriate charges are reflected in a patient’s bill for services. AI can “learn” the common charges for a specific type of service, and ensure those charges are included before the organization submits the claim to the payer.
- Medical coding: AI-powered coding systems can analyze clinical documentation and suggest appropriate codes based on the patient's diagnosis and treatment. This can help reduce coding errors and ensure accurate claims submission.
- Payment posting: Organizations can use AI and RPA to record payments on an account as soon as they happen.
- Claims lifecycle and analytics-driven workflows: AI can assess RCM data and help organizations understand where their RCM processes are inefficient or ineffective. That can pinpoint ways for organizations to improve their entire RCM system and process. “No human can go through millions of records and figure out a pattern,” Mathew says. But AI can analyze that data and related RCM metrics to determine patterns that can improve RCM process, decrease costs, and increase revenue, he says.
- Accounts receivable analysis: AI can help organizations analyze their accounts receivable data to figure out ways to get more bills paid more quickly. It can help identify data patterns and filter by clinic location, provider and other variables.
- Patient access: Many people in the U.S. and throughout the world have limited access to physicians, other medical experts and specialized tests. AI can improve people’s access to needed healthcare in many ways. For example, it can analyze X-rays and other imaging tests to screen for cancer and other diseases. That means people who live in rural areas without access to radiologists can still immediately get their X-rays reviewed.
- Fraud detection: AI can help organizations assess data to look for patterns that mean fraud, leading to further investigation.
Barriers to Adopting AI in Revenue Cycle Management
You may face a few obstacles to implementing RCM AI. Typical ones include data integration, security, expertise and cost. However, you can overcome these obstacles with the right software, training and setup.
Here’s a detailed look at the possible obstacles to RCM AI and expert tips to overcome them:
Resistance to change: Healthcare organizations have performed revenue cycle management in the same way for years. Healthcare organizations also tend to be careful with new and unproven processes. All of that makes people within the organization resistant to significant changes in RCM processes.
How to Build the Business Case for AI in RCM
Your team can build a business case for AI in RCM by demonstrating to organizational leaders how it can improve RCM, decrease costs and increase revenue. Your team can also show the likely return on investment of AI in RCM.
Here are important steps to build the business case:

Also, you can download all of the templates that can help your team make the business case for AI in RCM.
Business Case for AI in RCM Template Set

Potential Risks and Challenges Implementing AI in RCM
- Data Quality and Accuracy: AI models heavily rely on data for training and decision-making. If the data used is incomplete, biased, or inaccurate, it can lead to faulty predictions, incorrect billing, and potential financial losses. It's crucial to ensure data integrity, proper data preprocessing, and ongoing monitoring to maintain accuracy.
- Privacy and Security: RCM involves handling sensitive patient data, including medical records, insurance information, and financial details. Implementing AI systems introduces additional points of vulnerability and increases the risk of data breaches or unauthorized access. It's essential to implement robust security measures, including encryption, access controls, and regular audits, to protect patient privacy and comply with data protection regulations.
- Regulatory Compliance: The healthcare industry is heavily regulated, with various laws and regulations governing billing practices, patient data privacy (such as HIPAA in the U.S.), and insurance reimbursement. AI systems must adhere to these regulations, which can be complex and subject to changes. Ensuring that AI models and processes comply with all applicable laws and regulations is crucial to avoid legal and financial consequences.
- Lack of Explainability: AI models, such as deep learning neural networks, are often considered "black boxes" because their decision-making process is not easily explainable. This lack of transparency can raise concerns about how AI algorithms arrive at specific decisions or predictions. In the context of RCM, it's important to strike a balance between accuracy and the ability to provide clear explanations for decisions made by AI systems.
- Resistance to Adoption: Implementing AI in RCM may encounter resistance from staff members who fear that AI technologies could replace their roles or disrupt established workflows. Overcoming resistance and ensuring proper training and change management efforts are essential to gain acceptance and maximize the benefits of AI in RCM.
- Ethical Considerations: AI systems need to be designed and deployed ethically to ensure fairness, avoid bias, and prevent discrimination. The algorithms used should be regularly monitored and audited to detect and mitigate any potential biases or unintended consequences that may arise during AI decision-making processes.
To mitigate these risks, organizations should establish proper governance frameworks for AI implementation. This includes:
- Robust data management practices
- Ongoing monitoring and auditing of AI systems
- Transparent communication with stakeholders, and involving domain experts in the development and validation of AI models
Additionally, engaging legal and compliance teams to ensure adherence to regulations and ethical guidelines is crucial in mitigating risks associated with AI in RCM.
The Future of AI in Revenue Cycle Management
In coming years, AI will have an increasingly large role in healthcare RCM. Experts believe that healthcare organizations will increasingly use AI in all parts of RCM – from the beginning to the end.
Experts also foresee these other developments:
- AI as a service: More organizations will gain expertise and provide AI as a specific service to healthcare organizations. That will mean healthcare organizations will not have to make huge upfront investments – in hiring new experts and in overall costs – to improve their RCM with AI.
"Our EMR vendors will be spending more time in how they can help improve workflows and potentially be using that AI as part of the AI solution,” Daye says.
How AI is Transforming RCM
AI is already transforming how healthcare organizations perform effective RCM. For example, it is helping organizations collect on medical bills much more quickly. It is reducing insurance claim denials. And it is improving medical coding.
Here are some examples:
- With help from Plutus Health, an obstetrics and gynecology provider, used AI to better understand reasons for a range of denials. The provider then generated more than $245,000 from overdue accounts and claim denials in three months.
- A medical lab was experiencing coding errors and was not processing payor denials and rejections. Plutus Health helped the lab to implement coding standards and use AI to perform eligibility checks . As a result, the lab’s collections per claim rose from $808 to $1,282.
- A small urgent care clinic couldn’t keep up with all tasks needed to perform their RCM processes. Plutus Health created a plan that included a range of help, including AI automation for the fast and accurate posting of charges . The clinic’s collections percentage increased from 80% to 95% in six months.
Get a Free AI RCM Readiness Assessment
Plutus Health can conduct an assessment of your organization's current state of readiness for implementing AI in RCM. Our evaluation will identify any potential gaps or areas of improvement to address before proceeding with the implementation.
We can then help you develop a strategic plan for implanting AI in your RCM system. We can help define the scope of the work and identify key stakeholders. We can also develop a road map for implementation and provide project costs and benefits.

Liked the blog? Share it
Loved our blogs.
Subscribe and stay updated with the latest announcements, information and more.

Thomas John, CEO of Plutus Health

Get in touch
Follow us on:.

Subscribe to Newsletter
Discover, learn, grow with our rcm blogs.
Maximizing Your Revenue: An In-Depth Look at Healthcare Revenue Cycle Management Phases and Steps
Importance of Revenue Cycle Management in Healthcare: Business, Facility and Patient Benefits

Check our latest blogs
Copyright © 2023 Plutus Health. All Rights Reserved
Fill in the form to download the checklist
- Revenue Cycle Management Market
- Top Market Reports
Revenue Cycle Management Market Size, Share & Trends by Product & Services (Eligibility Verification, Clinical Coding, CDI Solutions, Claims Processing, Denial Management, Outsourcing Services), Delivery (Cloud), End Users (Payers, Hospitals) & Region - Global Forecast to 2028

- Description
- TABLE OF Contents
- METHODOLOGY
- DOWNLOAD PDF

Revenue Cycle Management Market Size, Share & Trends
The size of global revenue cycle management market in terms of revenue was estimated to be worth $49.6 billion in 2023 and is poised to reach $84.1 billion by 2028, growing at a CAGR of 11.1% from 2023 to 2028. The comprehensive research encompasses an exhaustive examination of industry trends, meticulous pricing analysis, patent scrutiny, insights derived from conferences and webinars, identification of key stakeholders, and a nuanced understanding of market purchasing dynamics.
Adoption of RCM solutions has increased post the pandemic to reduce the burden on healthcare resources. Newly developed RCM solutions help streamline workflows, enhance data accuracy, improve compliance, and provide a better overall experience for healthcare providers and patients. Furthermore, these RCM solutions offer real-time insights, enable seamless data exchange, support interoperability, and reduce costs for managing multiple standalone systems. Therefore, the rising availability of highly efficient RCM solutions has positively influenced market growth. Moreover, improving data integration standards such as HL7 for efficient data transfer has further enhanced the RCM market growth.
Revenue Cycle Management Market Trends
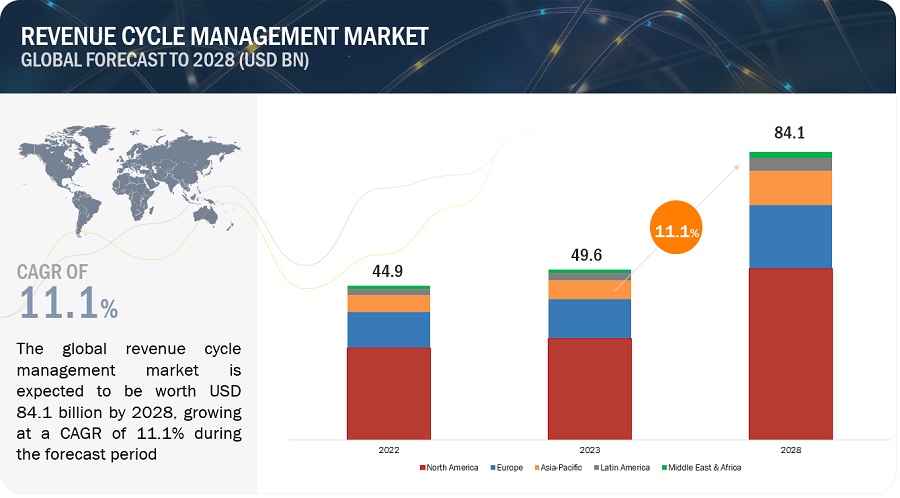
To know about the assumptions considered for the study, Request for Free Sample Report
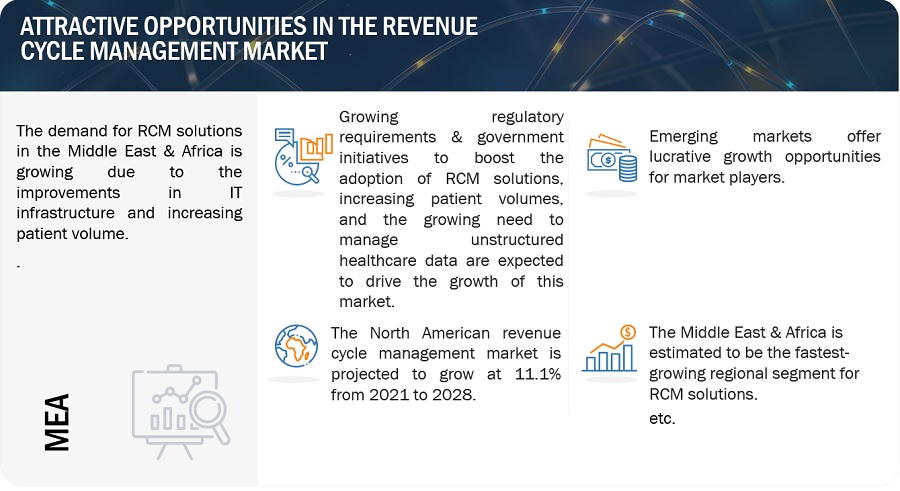
Revenue cycle management Market Dynamics
Driver: growing need to manage unstructured healthcare data.
In the last few years, the volume of electronic data produced in the healthcare industry, primarily due to rising patient volumes and the digitization of administrative, clinical, and financial information, has expanded to terabytes and petabytes. This generates an imperative need to use revenue cycle management solutions. According to industry experts, by using natural language processing (NLP) and optical character recognition (OCR) technology, organizations can transform unstructured data from files, such as medical records, scanned documents, and audio recordings, into structured and normalized data. Other significant factors contributing to this trend are the sheer diversity of data in healthcare and the rising prominence and usage of HCIT tools.
Restraint: Deployment costs include licensing and subscription costs, hardware infrastructure, customization costs, and implementation services cost.
Cost of licensing and implementation is substantially high. Moreover, the price associated with maintaining revenue cycle management software has also significantly increased. Furthermore, IT support and maintenance services, including modifying and upgrading software per changing user requirements and maintaining an efficient IT infrastructure, represent a recurring expenditure. This accounts for a large share of the total cost of ownership. Also, post-sale custom interface development for device integration requires additional verification and validation to ensure solution accuracy and completeness. In 2021, many healthcare providers and their revenue cycle management (RCM) departments faced challenges. Operational costs outpaced revenue growth leading to months and quarters in the red. At the end of 2022, the American Hospital Association anticipated that between 53% and 68% of hospitals would be in deficit, compared to 34% in 2019. This further increases the total cost of ownership for healthcare providers. As a result of the high costs involved, small healthcare facilities, especially in emerging countries, are reluctant to replace their legacy systems with RCM solutions.
Opportunity: Growing demand for AI & cloud-based deployment
The combination of data and artificial intelligence (AI) has the potential to improve outcomes and reduce costs by applying machine learning algorithms and predictive analytics to reduce drug discovery times, provide virtual assistance to patients, and reduce the diagnosing time for ailments by processing medical images. The adoption of AI in healthcare is rising due to its ability to optimize clinical as well as non-clinical processes, thereby solving a variety of problems for patients, providers, and the overall healthcare industry. According to MarketsandMarkets estimates, AI in Healthcare market is predicted to grow at a double-digit rate. AI has experienced high demand for RCM solutions to overcome the load on human resources. Manual and redundant tasks that occur during patient access, coding, billing, collections, and denials can be automated with the help of AI. AI integrated with RCM can perform these functions more accurately by imitating intelligent human behavior through algorithms that find patterns and plan future actions to produce a positive outcome.
Challenge: Issues related to data security and confidentiality
The increased use of automated technologies such as EHRs, healthcare integration, and health information exchanges have helped expand the healthcare privacy and security landscape. Electronic patient data exchange offers greater reach and efficiency in healthcare delivery but has high-security risks due to the broader access. The Anthem Inc. Data breach, Ransomware attack, and Accellion FTA Hack have been the most significant cyberattacks in recent years, jeopardizing USD 47.76 million patient records altogether, causing USD 81.5 million loss. Concerns over the security of proprietary data and applications form a significant challenge to the growth of the market.
Revenue Cycle Management Market Ecosystem
The aspects present in this market are included in the ecosystem market map of the overall revenue cycle management market, and each element is defined with a list of the organizations involved. Products and services are included. The manufacturers of various products include the organizations involved in the entire process of research, product development, optimization, and launch. Vendors provide the services to end users either directly or through a collaboration with a third party.
In-house research facilities, contract research organizations, and contract development and manufacturing companies are all part of research and product development and are essential for outsourcing product development services.
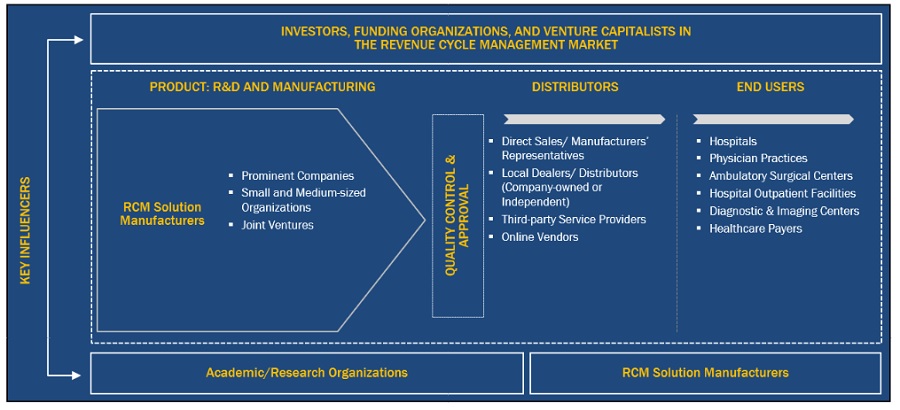
Source: Secondary Literature, Interviews with Experts, and MarketsandMarkets Analysis
By product & services segment, the outsourcing services segment of revenue cycle management industry is expected to grow at the highest growth rate during the forecast period
The outsourcing services segment of revenue cycle management market is expected to grow at the highest CAGR during the forecast period among the product & services. RCM services are outsourced to improve financial performance, navigate complex regulatory landscapes, access specialized expertise, leverage advanced technology, and focus on core healthcare operations. Outsourcing RCM allows organizations to optimize revenue cycles, enhance financial outcomes, and streamline processes in a rapidly changing healthcare environment. Therefore, due to the above-mentioned benefits, the segment is predicted to have a significant growth rate.
The on-premise segment is expected to account for the largest revenue cycle management industry share by delivery mode.
The on-premise segment accounted for the largest share of the revenue cycle management market in 2022. On-premise RCM software provides organizations with greater customization and flexibility. Since the software is deployed locally, it can be tailored to specific workflows, processes, and reporting requirements. This allows organizations to align the RCM software more closely with their unique needs, providing a more personalized and efficient solution thereby, elevating the segment share.
By end user, the healthcare providers segment is expected to account for the largest revenue cycle management industry share.
Healthcare payers and providers are the two segments of the global revenue cycle management market based on end users. The healthcare providers segment accounted for the largest market share 2022. The significant market share of this sector can be ascribed to the effective RCM processes and technologies that provide healthcare providers with improved financial performance, streamlined workflows, enhanced compliance, and a better overall patient experience. By leveraging RCM solutions, healthcare organizations can optimize revenue cycles, increase efficiency, and allocate resources more effectively to deliver high-quality patient care. The aforementioned factors have positively impacted segmental growth.

To know about the assumptions considered for the study, download the pdf brochure
During the forecast period, the Asia Pacific region had a substantial growth rate in the revenue cycle management market. The regional growth can be attributed to the rising penetration of digital healthcare technologies along with improving infrastructure. Moreover, medical tourism is increasing especially in the South East Countries that has further elevated the regional market growth to a certain extent.
The major players in the global revenue cycle management market are R1 RCM (US), Oracle (US), Optum (US). Other prominent players in the market include AdvantEdge Healthcare (US), McKesson Corporation (US), Change Healthcare (US), 3M (US), Experian plc (Ireland), Conifer Health Solutions (US), Veradigm (US), GE Healthcare (US), Cognizant (US), athenahealth (US), SSI Group LLC (US), McKesson Corporation (US), and Huron Consulting Group (US).
Scope of the Revenue Cycle Management Industry
|
|
|
| Market Revenue Size in 2023 | $49.6 billion |
| Projected Revenue Size by 2028 | $84.1 billion |
| Industry Growth Rate | Poised to Grow at a CAGR of 11.1% |
| Market Driver | Technological advancements and increasing R&D investments |
| Market Opportunity | Improvisation of healthcare infrastructure across emerging countries |
The research report categorizes the revenue cycle management market to forecast revenue and analyze trends in each of the following submarkets:
By Product & Services
- Eligibility Verification Solutions
- Pre-certification & Authorization Solutions
- Other Patient Access Solutions
- Clinical Coding Solutions
- Clinical Documentation Improvement Solutions
- Other Mid-revenue cycle Solutions
- Claims Processing Solutions
- Denial Management Solutions
- Other Back-end Revenue cycle Solutions
- Patient Access Outsourcing Services
- Mid-revenue cycle Outsourcing Services
- Back-end Revenue cycle Outsourcing Services
By Delivery Mode
- On-premise Solutions
- Cloud-based Solutions
By End User
- Physicians Practices
- Ambulatory Surgical Centers (ASCs)
- Hospital Outpatient Facilities
- Diagnostic & Imaging Centers
- Other Outpatient Facilities
- Healthcare Payers
- Rest of Europe
- Rest of Asia Pacific
- Latin America
- Middle East and Africa
Recent Developments of Revenue Cycle Management Industry
- In 2023, Optum partnered with Owensboro Health to manage revenue cycle and information technology and improve patient outcomes and safety.
- In 2022, the R1 RCM announced 10-year end-to-end RCM partnerships with Scion Health, Sutter Health, and St. Clair Health to streamline workflow standardization and improve patient access platforms.
- In 2022, McKesson signed a definitive agreement to acquire Rx Savings Solutions to offer medication therapy more affordable and increase medication adherence to improve outcomes.
Frequently Asked Questions (FAQ):
What is the projected market revenue value of the global revenue cycle management market?
The global revenue cycle management market boasts a total revenue value of $84.1 billion by 2028.
What is the estimated growth rate (CAGR) of the global revenue cycle management market?
The global revenue cycle management market has an estimated compound annual growth rate (CAGR) of 11.1% and a revenue size in the region of $49.6 billion in 2023.
To speak to our analyst for a discussion on the above findings, click Speak to Analyst
This study involved the extensive use of both primary and secondary sources. It involved the study of various factors affecting the industry to identify the segmentation types, industry trends, key players, the competitive landscape of market players, and key market dynamics such as drivers, opportunities, challenges, restraints, and key player strategies.
Secondary Research
This research study involved the wide use of secondary sources, directories, databases (such as Bloomberg Businessweek, Factiva, and D&B Hoovers), white papers, annual reports, company house documents, investor presentations, and SEC filings of companies. Secondary research was undertaken to identify and collect information for this extensive, technical, market-oriented, and commercial revenue cycle management market study. It was also used to obtain important information about the key players, market classification and segmentation according to industry trends to the bottom-most level, and key developments related to market and technology perspectives. A database of the key industry leaders was also prepared using secondary research.
Primary Research
In the primary research process, various sources from supply and demand sides were interviewed to obtain qualitative and quantitative information for this report. Primary sources from the supply side include industry experts such as CEOs, vice presidents, marketing and sales directors, technology & innovation directors, and related key executives from various key companies and organizations operating in the revenue cycle management market. The primary sources from the demand side include clinicians, cardiologists, hospital managers, professors, and and stakeholders in corporate & government bodies. Primary research was conducted to validate the market segmentation, identify key players in the market, and gather insights on key industry trends and key market dynamics.
A breakdown of the primary respondents is provided below:
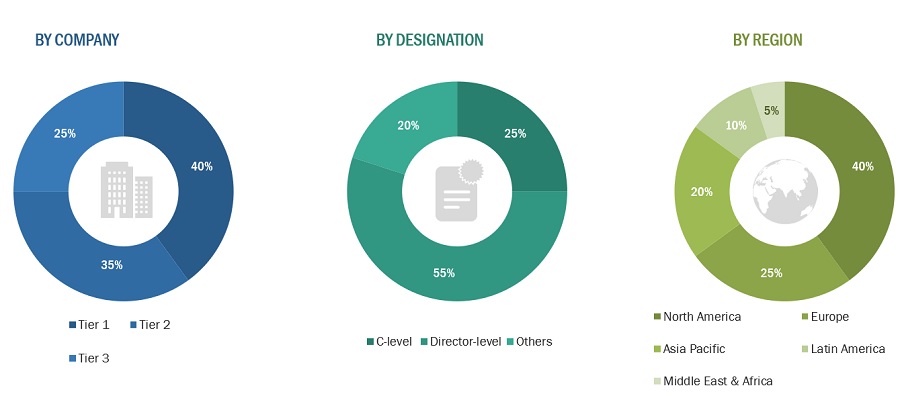
Tiers are defined based on a company’s total revenue. As of 2022: Tier 1= >USD 1 billion, Tier 2 = USD 500 million to USD 1 billion, and Tier 3= <USD 500 million.
Market Size Estimation
The total size of the revenue cycle management market was arrived at after data triangulation from four different approaches. After each course, the weighted average of the three approaches was taken based on the level of assumptions used in each approach.
Method for calculating the revenue of different players in revenue cycle management. Annual reports, SEC filings, online publications, and in-depth primary interviews were used to determine the size of the worldwide revenue cycle management market. The market segment sizes were determined using a percentage split. In order to determine the size for each sub-segment, additional splits were used. Primary participants verified these percentage splits. The country-level market numbers from yearly reports, SEC filings, online publications, and in-depth primary interviews were summed up to determine the total market size for regions. The global revenue cycle management market was calculated by adding the market sizes for each region.
Approach to derive the market size and estimate market growth
The market size and market growth were estimated through primary interviews on a regional and global level. All responses were collated, and a weighted average was taken to derive a probabilistic estimate of the market size and growth rate.
Global revenue cycle management market size: Top-Down Approach
Data Triangulation
The market was divided into a number of segments and sub-segments after the overall market size was estimated through the above-described market size estimation processes. To complete the overall market engineering process and arrive at the exact statistics of each market segment and sub-segment, the data triangulation and market breakdown procedures were employed, wherever applicable. The data was triangulated by studying various factors and trends from both the demand and supply sides.
Market Definition
Revenue cycle management (RCM) is the process used to track the revenue from patients, from their initial appointment or encounter with the healthcare system to their final payment of the balance. This process helps streamline the business operations of healthcare organizations and private practices. RCM solutions help providers manage and enhance revenue cycle functions such as medical coding & billing, patient insurance eligibility verification, electronic health records, clinical documentation, and claims & denials management.
Key Stakeholders
- Healthcare Providers
- Healthcare Vendors
- Technology Developers
- Regulators and Policy makers
- Insurance companies and payers
- Government Institutions
- Market Research and Consulting Firms
- Venture Capitalists and Investors
Objectives of the Study
- To define, describe, and forecast the global revenue cycle management market by product & services, delivery mode, end-user, and region
- To provide detailed information about the significant factors influencing the market growth (such as drivers, restraints, opportunities, and challenges)
- To analyze micromarkets with respect to individual growth trends, prospects, and contributions to the overall revenue cycle management market
- To analyze market opportunities for stakeholders and provide details of the competitive landscape for key players
- To forecast the size of the revenue cycle management market in five major regions along with their respective key countries (North America, Europe, Asia-Pacific, Latin America, and Middle East & Africa)
- To profile the key players in the global revenue cycle management market and comprehensively analyze their core competencies and market shares
- To track and analyze competitive developments such as mergers, acquisitions, developments, expansions, partnerships, alliances, and R&D activities of leading players in the market
Available Customizations
With the given market data, MarketsandMarkets offers customizations as per the company’s specific needs. The following customization options are available for the report:
Geographic Analysis
- Further breakdown of the Rest of the Asia Pacific market into South Korea, Australia, New Zealand, and others
- Further breakdown of the Rest of Europe market into Belgium, Russia, Switzerland, and others
- Further breakdown of the Rest of the Latin America market into Brazil, Argentina, Colombia, Chile, and others
We will customize the research for you, in case the report listed above does not meet with your exact requirements. Our custom research will comprehensively cover the business information you require to help you arrive at strategic and profitable business decisions.

Instant Answers with GPT - Ask Now!
Request more details.
By clicking the "Submit" button, you are agreeing to the Terms of Use and Privacy Policy.
Growth opportunities and latent adjacency in Revenue Cycle Management Market
Which are the major growth driving factors for the End User segment of the Global Revenue Cycle Management Market?
How the healthcare providers segment holds the largest share of the Revenue Cycle Management Market?
Which are the fastest growing economies in the global Revenue Cycle Management Market?
Get recent trends delivered to your inbox
Overtake your competition with ease.
- Back-end Revenue Cycle Management Market
- Mid-Revenue Cycle Management/Clinical Documentation Improvement Market
- Insights-as-a-Service Market
- Healthcare Mobility Solutions Market
- Accountable Care Solutions Market
- Triangulate with your Own Data
- Get Data as per your Format and Definition
- Gain a Deeper Dive on a Specific Application, Geography, Customer or Competitor
- Any level of Personalization
- What are the Known and Unknown Adjacencies Impacting the Revenue Cycle Management Market
- What will your New Revenue Sources be?
- Who will be your Top Customer; what will make them switch?
- Defend your Market Share or Win Competitors
- Get a Scorecard for Target Partners

- Leadership Team
- Research Experts
- REQUEST FREE SAMPLE REPORT
- +1-888-600-6441 (Corporate office hours)
- +1-888-600-6441 (US/Can toll free)
- +44-800-368-9399 (UK office hours)

- Conferences
- Press Releases
- New Reports
- Research Insight
- Privacy Policy
- Terms and Conditions
- ©2024 MarketsandMarkets Research Private Ltd. All rights reserved

Markets and Markets research pvt ltd. (Jun, 2023 ). Revenue Cycle Management Market Size, Share & Trends by Product & Services (Eligibility Verification, Clinical Coding, CDI Solutions, Claims Processing, Denial Management, Outsourcing Services), Delivery (Cloud), End Users (Payers, Hospitals) & Region - Global Forecast to 2028 MarketsandMarkets. Retrieved Aug 4, 2024 , from https://www.marketsandmarkets.com/Market-Reports/revenue-cycle-management-market-153900104.html
Get Embed Code

Please enter your contact details it will help our analyst to reach out to you.

[email protected] | USA 1-888-600-6441
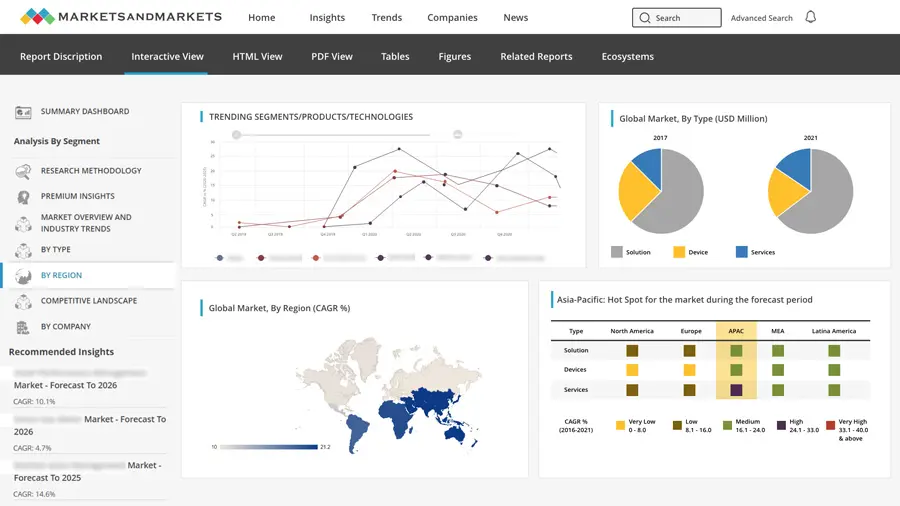
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My Portfolio
- Latest News
- Stock Market
- Biden Economy
- Stocks: Most Actives
- Stocks: Gainers
- Stocks: Losers
- Trending Tickers
- World Indices
- US Treasury Bonds
- Top Mutual Funds
- Highest Open Interest
- Highest Implied Volatility
- Stock Comparison
- Advanced Charts
- Currency Converter
- Basic Materials
- Communication Services
- Consumer Cyclical
- Consumer Defensive
- Financial Services
- Industrials
- Real Estate
- Mutual Funds
- Credit Cards
- Balance Transfer Cards
- Cash-back Cards
- Rewards Cards
- Travel Cards
- Credit Card Offers
- Best Free Checking
- Student Loans
- Personal Loans
- Car Insurance
- Mortgage Refinancing
- Mortgage Calculator
- Morning Brief
- Market Domination
- Market Domination Overtime
- Asking for a Trend
- Opening Bid
- Stocks in Translation
- Lead This Way
- Good Buy or Goodbye?
- Financial Freestyle
- Capitol Gains
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Yahoo Finance
Revenue cycle management (rcm) market size in us to grow by usd 11.98 billion from 2022 to 2027, growing adoption of a value-based reimbursement model to be a major trend, technavio.
NEW YORK , March 6, 2024 /PRNewswire/ -- The revenue cycle management (RCM) market in the US is set to grow by USD 11,985.2 million from 2022 to 2027 progressing at a CAGR of 9.94% during the forecast period. The report offers an up-to-date analysis regarding the current global market scenario, the latest trends and drivers, and the overall market environment. The growing need to reduce revenue leakages in healthcare systems drives market growth. There is an increased focus on reducing the growing revenue leakages to remain competitive in the market in focus from the market vendors in the healthcare service industry. Due to the additional time and resources needed in manual systems, revenue leaks cost more than using electronic systems. Furthermore, in the patient leak process, sometimes a healthcare service provider allows a patient to leave the care setting and sends statements to the patient later. This results in patient-level revenue leakage. Hence, owing to factors such as revenue leaks, the RCM market is estimated to grow during the forecast period.
Here is an Exclusive report talking about Market scenarios with a historical period (2017-2021) and the forecast period (2023-2027).
Download Sample Report in minutes!
|
|
Page number | 127 |
Base year | 2022 |
Historic period | 2017-2021 |
Forecast period | 2023-2027 |
Growth momentum & CAGR | Accelerate at a CAGR of 9.94% |
Market growth 2023-2027 | USD 11,985.2 million |
Market structure | Fragmented |
YoY growth 2022-2023(%) | 9.45 |
The growing adoption of a value-based reimbursement model
There is a shift from fee-for-service to value-based care reimbursements in the healthcare service industry. Value-based RCM is a reimbursement payment methodology, focusing more on quality healthcare at a reasonable cost. Owing to the adoption of programs and legislation by various governments, the involvement of healthcare service providers across the world in value-based RCM models is rising. Hence, such initiatives are expected to have a positive impact on the adoption of value-based RCM, which will boost the growth of the RCM market in the US during the forecast period.
Interoperability issues associated with RCM solutions challenge the growth of the RCM market in US.
Market Segmentation
This US revenue cycle management (RCM) market report extensively covers market segmentation by product (software and services) and end-user (hospitals, physicians, and medical labs).
The software segment will be significant during the forecast period. The growth of the segment can be attributed to factors such as the various software solutions that are specifically designed to streamline and automate the entire revenue cycle management (RCM) process. Furthermore, there are several vendors operating in the market that offer RCM as software solutions. For instance, Epic Systems Corporation offers an integrated suite of healthcare software solutions, including Epic Resolute, which is the company's revenue cycle management software and they provide comprehensive RCM functionalities. Hence, owing to such factors, the software segment of the RCM market is estimated to grow during the forecast period.
This report presents a detailed picture of the market by way of study, synthesis, and summation of data from multiple sources through an analysis of key parameters
View Sample Report
Companies Mentioned
Acclara Solutions LLC
athenahealth Inc.
CareCloud Inc.
Change Healthcare Inc.
Cognizant Technology Solutions Corp.
Computer Programs and Systems Inc.
eClinicalWorks LLC
Epic Systems Corp.
Experian Plc
International Business Machines Corp.
Koch Industries Inc.
McKesson Corp.
Medical Information Technology Inc.
Oncospark Inc.
Oracle Corp.
R1 RCM Inc.
Sage Group Plc
The SSI Group LLC
Veradigm LLC
Vendor Oferings
Acclara Solutions LLC - The company offers revenue cycle management solutions such as Patient Access, Revenue Integrity and Coding, Business Office, and Community Provider Solution.
athenahealth Inc. - The company offers revenue cycle management solutions such as athenaIDX for large practices, health systems, billing services, and hospitals.
Change Healthcare Inc. - The company offers revenue cycle management solutions and services for healthcare providers including hospitals, health systems, physicians, and non-hospital emergency medical service providers to support cash flow, increase speed to payment, and contain costs at a faster rate.
Gain instant access to 17,000+ market research reports.
Technavio's SUBSCRIPTION platform
Analyst Review
The US Revenue Cycle Management (RCM) market stands at the intersection of healthcare organizations' financial health and patient care quality. It encompasses a suite of processes vital to the financial viability of healthcare providers, starting from patient registration and extending through claims processing and payment collection. In an era of burgeoning healthcare costs and evolving reimbursement models like value-based care, efficient RCM practices are paramount for sustainability.
In this landscape, artificial intelligence (AI) and machine learning (ML) are emerging as game-changers. Companies like FutureWise Research delve into the AI in Healthcare market, offering innovative solutions for workflow optimization and data security. However, as the digitalization of healthcare accelerates, concerns over data security and confidentiality loom large, especially with the proliferation of EHRs and health information exchanges.
These challenges are exacerbated by the threat of ransomware attacks, underscoring the need for robust data security measures. Amidst this backdrop, R1 RCM Inc. and other players offer RCM software solutions that integrate medical billing and coding with advanced AI algorithms to streamline processes and mitigate risks.
The market's services segment is witnessing a surge, with providers increasingly outsourcing RCM solutions to specialized firms. These firms leverage machine learning algorithms for claims processing and insurance verification, enhancing efficiency and accuracy while reducing administrative burden.
However, the industry grapples with data siloes and fragmented systems, hindering seamless process digitalization. Companies are thus investing in patient management solutions that break down these barriers, enabling comprehensive patient registration and care coordination.
The transition to ICD-10 further underscores the need for agile RCM solutions capable of adapting to evolving coding standards. Future growth prospects lie in emerging markets, where demand for RCM services is burgeoning, fueled by increasing healthcare expenditure and regulatory reforms.
In essence, the US RCM market is undergoing a transformative shift driven by technological innovation and evolving healthcare dynamics. Companies that navigate this landscape adeptly, harnessing the power of AI and data analytics while prioritizing data security and compliance, are poised to thrive in this dynamic ecosystem.
Related Reports: The telecom billing revenue management market size is estimated to grow at a CAGR of 8.73% between 2022 and 2027. The telecom billing revenue management market size is forecast to increase by USD 6.99 billion. This telecom billing revenue management market report extensively covers market segmentation by solution (software and services), deployment (on-premise and cloud), and geography ( North America , Europe , APAC, South America , and Middle East and Africa ). The expanding telecom services are notably driving the market growth.
The innovation management market size is estimated to grow at a CAGR of 10.3% between 2022 and 2027. The market size is forecast to increase by USD 774.63 million.This innovation management market report extensively covers market segmentation by component (services and solutions), deployment (cloud-based and on-premises), and geography ( North America , Europe , APAC, South America , and the Middle East and Africa ). Growth in infrastructure development is the key driver notably driving the growth of the global innovation management market.
Key Topics Covered:
1 Executive Summary 2 Landscape 3 Sizing 4 Historic Size 5 Five Forces Analysis 6 Segmentations 7 Customer Landscape 8 Geographic Landscape 9 Drivers, Challenges, and Trends 10 Vendor Landscape 11 Vendor Analysis 12 Appendix
About US Technavio is a leading global technology research and advisory company. Their research and analysis focuses on emerging market trends and provides actionable insights to help businesses identify market opportunities and develop effective strategies to optimize their market positions. With over 500 specialized analysts, Technavio's report library consists of more than 17,000 reports and counting, covering 800 technologies, spanning across 50 countries. Their client base consists of enterprises of all sizes, including more than 100 Fortune 500 companies. This growing client base relies on Technavio's comprehensive coverage, extensive research, and actionable market insights to identify opportunities in existing and potential markets and assess their competitive positions within changing market scenarios. Contact Technavio Research Jesse Maida Media & Marketing Executive US: +1 844 364 1100 UK: +44 203 893 3200 Email: [email protected] Website: www.technavio.com
View original content to download multimedia: https://www.prnewswire.com/news-releases/revenue-cycle-management-rcm-market-size-in-us-to-grow-by-usd-11-98-billion-from-2022-to-2027--growing-adoption-of-a-value-based-reimbursement-model-to-be-a-major-trend-technavio-302080926.html
SOURCE Technavio

- Aug 25, 2021
RCM business plan

Today we are going to discuss about the Rcm Business Plan in this article. We will discuss in detail what is Rcm business plan, how to join Rcm business plan, what are the benefits of Rcm marketing plan. We will also tell you what is Rcm Business.
How you can make money with little efforts under Rcm marketing plan 2021. Rcm is a direct selling MLM (Multi Level Marketing) Indian company. Rcm is a product based MLM company of India.
Before we start our article about the Rcm business plan, first we should know about the Rcm company history and profile and who owns Rcm company. So, let’s know about these questions.
Guys, as said above, Rcm is a direct selling MLM company of India . It was set up by a clothing trading company “Fashion Suitings Pvt Ltd.” at Bhilwara in Rajasthan since 1977 by the Chhabra Group. In 1986 Rcm business started its own production. It was founded by Trilok Chand Chhabra (Owner of Rcm Business).

Sh. Trilok Chand wants to remove all the intermediators between the manufacturer and the final customers, so that product may be available to customer at a low price. His idea was to start a direct selling company.As a result, the Fashion Suiting Pvt Ltd. Company transformed to an Rcm Business, a direct selling MLM company.
Table of Content
Rcm Marketing Plan
List of Profit Under Rcm Marketing Plan 2021
Performance Bonus
Royalty bonus, technical bonus.
Important facts of Rcm plan 2021
What is Rcm Business?
Why rcm business is important.
Why We Do Rcm Business?
How to Do Rcm Business Income?
Types of Income in Rcm Business
What to do in Rcm Business After Joining?
Today Rcm is manufacturing around 730 products, having 8 million distributors and 1000 Pickup Centre all over the India. Rcm Business currently manufacturing almost all types of products like health supplements and herbal medicines, food and grocery, clothing for children, women and men as well as a wide array of other stuff such as bags, stationery, tools and many more. Now let’s begin today’s article and learn about the Rcm business plan 2021.
Rcm Business Plan
Guys today we will learn about the Rcm business plan 2021 in detail and know that how you can earn money under Rcm business and marketing plan. Guys as discusses earlier Rcm business comes under Right Concept Marketing, which is a kind of multi-level networking business which is owned by Chhabra Group.
Guys as told; Rcm company is a product based direct selling multi-level marketing company. Now you may be thinking that why its important to join Rcm business plan and what are its benefits to us. So, let’s understand it with an example that what is the benefits to buy a product from Rcm business.

A XYZ company manufacture a product, whose manufacturing cost amounts up to Rs. 100. After that, when a company launch that product in the market, they need to do product promotion which amounts up to Rs. 50.
After that product goes to the selling agency which add their profit. Let’s assume they add Rs. 20 as their profit in the product cost. Now the product goes to wholesaler and then he will add his profit up to Rs. 20 and after that product goes to the retailer and he will also add his profit up to Rs. 10.
After add all these cost the product reaches to the final customer. Now product price which will customer need to pay for that product amounts Rs. 200 (Rs. 100 for manufacturing cost and company profit + Rs. 50 for product promotion + Rs. 20 as selling agency profit + Rs. 20 as wholesaler profit + Rs. 10 as retailer profit).
Guys, this is the big disadvantage of regular system which is followed by our Indian market. Rs. 100 amounting product is provided to the final customer in Rs. 200. You can easily see the drawback of this system. Whereas on other hand is direct selling method is here under Rcm business plan.
In direct selling company, all the extra cost like promotion cost, profits of selling agency, wholesalers and retailers. Under direct selling method, final customer gets the product at low price by eliminating the wasteful extra cost. Also, the Rcm group provide you 100% pure products and good quality products.
In this way, Rcm marketing plan is 100% beneficial for us as compare to buy the goods from the market because with direct selling system, Rcm business plan also allow us to earn some money, in the form of retail profit, performance bonus, royalty bonus, and technical bonus.
So, let’s know how to earn under Rcm marketing plan. To get benefits of Rcm marketing plan you first need to join Rcm business. So, below is the process of joining Rcm business. Let’s see it first.
First Step: First you need to visit official website of Rcm business i.e., www Rcmbusiness com or another way is just going to playstore and search for Rcm business official app and download /install it in your android smart phone.
Second Step: Then click on the direct seller option which will be showing on the left side of the website and then many options will be shown in front of you. You have to click on the e KYC application for New Direct Seller.
Third Step: Once you click on the e KYC application for New Direct Seller option then a registration form will open in front of you. Now you need to fill your detail in the form and submit it in the online mode. You need to fill following information.
Applicant Personal Details
As soon as you click, a new interface will appear in front of you, in which you have to enter the applicant personal details. First of all, it is the sponsor number, before filling it, it is necessary to know what it is.
Sponsor Number is the person under whom you are joining. Whose ID is at the bottom, below which you are joining is your sponsor number.
After this you need to enter Proposer Number, this number of the one, who proposes you to join Rcm business. Now you get to see Gender column under it. After this comes the marital status.
Now it is the turn of the name title, in this you will get Mr. or Mrs. Which you have to select. After filling this in Joining in Rcm Business Plan, you have to fill the Applicant Name in it.
After this, you have to upload applicant picture for the joining of the applicant in Rcm Business Plan. After this, the name of your father and after that the date of birth will have to be filled.
Applicant Nominee Details
After this comes Nominee details, in this you have to fill the information related to your Nominee. Like their name, date of birth and relation and address.
Applicant Communication Details
Then in next you need to enter your communication details joining in Rcm Business Plan. In this your address, state, district, tehsil, post office, city and pin code will be entered.
Along with this, you need to enter your mobile number, you have to fill the same number that you have with you while filling the form because you will get One Time Password on it and you will have to fill it.
After this you will also have to give an ID proof of yours. In this you can also give your Aadhar Card. Along with this, you will also have to upload a photo of your ID proof .
You can also give Pan Card and Driving License instead of Aadhaar Card. You can give your Aadhar card as Address Proof for joining in Rcm Business Plan. You need to upload both side of your Aadhar card.
Applicant Bank Details
After this comes Bank Details, in this you have to fill the name of the bank, bank branch name and your account number, after which you have to upload the first page of your bank account passbook on which the account number and IFSC code are given. Now you have to fill PAN card details. It's your wish, you can fill it if you want.
Security Details
After this comes the Security Details. In this you have to make your password as per your wish and fill it. After that you have to confirm it by filling it again. In Joining in Rcm Business Plan, now select Hint Question as soon as you click on it, many options will come in front of you, you can take any one.
After this comes Hint answer, in this you have to write the answer to that question. This hint question will be asked from you when in future you forgot your password and wants to reset it.
Applicant Family Details
After this, in Joining in Rcm Business Plan, you get another option in which if any of your family member is already in Rcm then you have to fill the details related to it like their ID Number, if not then you can leave it.
At the end you will get that you have read all the terms and conditions and you agree to them. You have to select it. After this you have to click on Send OTP in Joining in Rcm Business Plan. Thus, OTP will come on the number that you entered. Your joining will start as soon as you fill form and submit it. After submitting your form, you will get a reference number.
Additional Read : Rcm Songs
In this way you can join under Rcm marketing plan. And now we will discuss what are the benefits you will get after join Rcm under Rcm marketing plan 2021. Following listed are the benefits of Rcm marketing plan 2021. We will also discuss them in detail.
List of Profits Under Rcm marketing plan 2021.
Retail Profit : One of the main benefits of Rcm Business plan 2021. You can buy the product from the Rcm pick up point at a discount rate up to 10-20% and then sell these products at M.R.P to other customers. In this way you earn profit which is known as retail profit. Let’s understand this with an example.
Let’s assume that you are a direct seller under Rcm business plan. Now you purchased a product from Rcm pickup point whose M.R.P is Rs. 100. You will get that product at a 20% discount price rate i.e., Rs. 80. Now if you sell this product at M.R.P then you get Rs. 20 as a retail profit.
Discount up to 10-20%: Under Rcm business plan 2021, you get the Rcm products at a discounted rate from the M.R.P. You get 10 to 20% of discount rate depending upon your BV (business volume). You just need to join Rcm business plan first and then enjoy the Rcm products at a discounted rate.
To know about this, you should first know about the BV because your performance bonus depends upon your BV points and your group BV.
BV stands for Business Volume. Every product that you buy from the Rcm has BV points. Yours and your groups BV points are added together in the end of the month and the commission is given to you as a performance bonus up to 32% depending up on your BV points.
Further you have to distribute this commission with your group . Business volume table is given below. Let’s see this and understand the calculation of Performance bonus with the help of an example given below the table of performance bonus.

Calculation of Performance Bonus
Example: Purchase in A leg (group)= 80,000 B.V.
Purchase in B leg (group)= 16,000 B.V.
Purchase in C leg (group)= 14,000 B.V.
Self-purchase = 5,000 B.V.
Total Business Volume = 1,15,000 B.V.
Calculation of Performance Bonus:
Bonus of total group (1,15,000 x 24%) = 27,600/-
Less Bonus of A leg (80,000 x 21.5%) = 17,200/-
Less Bonus of B leg (16,000 x 14%) = 2,240/-
Less Bonus of C leg (14,000 x 14%) = 1,960/-
Net performance bonus = 6,200/-
Above examples are given for understanding.
Note : Performance Bonus will be released to only those Direct Sellers whose minimum purchase of RCM Products is 100 Rs. on accrual basis in the relevant month. Performance Bonus will be calculated on monthly Business Volume on difference basis system (Deduction of performance bonus of downline from performance bonus of total group)
Royalty Bonus is given up to 8% on the basis of your business volume points. Royalty Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Royalty is given on the basis of difference by deducting downline royalty from the total royalty. Royalty always calculated on monthly basis.
When a group other than the main group able to make their BV up to 3,50,000 BV or more, it is called second leg (group) and if the other group (other than the main and second group) make their BV points of 1 15,000 or more than they will also get royalty at the second group as per the applicable slab.

Royalty will be released to only those Direct Sellers whose minimum purchase of RCM Products is 1500 B.V. on accrual basis in the relevant month.
Royalty will be calculated on difference basis by deducting Royalty of downline from total Royalty.
Royalty will be calculated on monthly basis.
When B.V. of any other leg (group) except main leg (group) is 3,50,000 or more, it is called the second leg (group) and if B.V. of other leg/legs (other than main and second leg) is 1,15,000 or more, then he will get Royalty on the second leg (group) also as per the slab applicable.
Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Also, he or she should be successfully earning the royalty income up to 8% percent for consecutive 3 months. Technical bonus is given on the basis of difference by deducting downline technical bonus from the total technical bonus. Technical bonus is always calculated on monthly basis.
When a group other than the main group able to make their BV up to 5,00,000 BV or more, it is called second group and if the other group (other than the main and second group) make their BV points of 5,00,000 or more than they will also get technical bonus at the second group as per the applicable slab.

Technical Bonus will be released to only those Direct Sellers whose minimum purchase of RCM Products is equivalent to 1500 B.V. on accrual basis in the relevant month.
Technical Bonus will be calculated on difference basis by deducting Technical Bonus of downline from total Technical Bonus of the main leg (group).
Technical Bonus will be calculated on monthly basis.
Direct Seller, who fulfills 8 % Royalty for consecutive 3 months, shall be entitled for Technical Bonus.
When B.V. of any other leg (group) except main leg (group) is 5,00,000 or more, it is called the second leg and if B.V. of other leg/legs (other than main and second leg) is 5,00,000 or more, then he/she will get Technical Bonus on the second leg (group) also as per the slab applicable.
Terms & Conditions:-
Except for abnormal reasons calculation of Sales Incentive shall be completed within 40 days from the last day of the month, for which Sales Incentive is to be calculated.
The amount of Sales Incentive will be remitted within in 90 days from the date of calculation of the Sales Incentive. Sales Incentive below Rs. 500 shall be remitted once within one year from the date of the first accrual of Sales Incentive.
Payment of Sales Incentive shall be made by anyone mode of Banking System (NEFT/RTGS/INTER BANKING TRANSFER). For this, it is mandatory to give correct bank account number and IFSC detail by Direct Seller.
If Direct Seller does not receive payment due to Non-compliance of rules of Direct Selling by Direct Seller or by any other reason created by Direct Seller, then complete responsibility for delay/ Non-payment will be of Direct Seller
If any defect is found in any of the RCM Products purchased, then the same can be returned/ exchanged within 30 days from the date of purchase. The returned product must be supported with Bill of purchase and such product should not be damaged from any angle. The purchaser should ensure that condition of the product should be similar to the condition which was prevailed at the time of purchases.
Important Facts of Rcm business plan 2021
Here we will discuss some important facts about Rcm Business Plan. These are given below :
Rcm (Rcm Business Plan) company includes 750 plus products.
Rcm has more than 15000 thousand stores across India
Rcm business headquarter is located in Bhilwara, Rajasthan.
Rcm company has started opening Rcm Wonder World in big cities all over India, where you will get all the products at one place.
Rcm (Rcm Business Plan) is a product based direct selling company.
Rcm has very strong roots.
Rcm is the only company that makes products based on Indian mindset.
In Rcm you can earn lakhs of rupees in less time with less efforts.
In Rcm (Rcm Business Plan), you can become a distributor of Rcm by buying a product worth one thousand rupees.
Rcm (Rcm Business Plan) is Indian MLM (Multi-level Marketing) company.
Direct Selling Rcm Business Benefiting its customers by providing them pure & genuine products.
Cheap Product along with Bill for every single purchase. Rcm Business Plan provides a fare bill of even one rupee of purchase is made.
Under Rcm marketing plan 2021 you get 10-20 percent discount. 10-32 percent performance bonus in your bank account, 3-8 percent royalty income generation, 1-5 percent technical income.
Rcm business follows all the government rules and regulations and strictly follow the guidelines of govt. for direct selling company. They pay their total liable tax to the Government of India.
Rcm marketing plan 2021 provides you self-employment opportunity.
Auspicious opportunity to fulfill all your dreams, being a participant in the progress of GDP of the country, also giving right direction to health with pure products. Awakening the spirit of helping each other.
Guys, Rcm business works on direct selling MLM method. This method is known as Right Concept Marketing. Friends we already have discuss about the benefit of direct selling method up on the regular method prevailing in Indian market.
Rcm business is one of the major role players in the industry of direct selling multi-level marketing. Let’s see how the Rcm business come into existence.
Rcm business earlier started as a clothing company known as “Fashion Suiting Pvt Ltd.” Which was establish in Rajasthan by the Chhabra Group in 1977. Further after some time Sh. Trilok Chand Chhabra realize that customers are getting exploited by the intermediators like selling agency, promotion cost, wholesalers and retailers.

Due to which product’s price rise and customer get the product at a high price. To solve this problem, Sh. Trilok Chand Ji (Owner and founder of Rcm business) started a direct selling system and reforms his existing clothing company to Rcm business group which is based up on direct selling product multi-level marketing method. He started Rcm business plan in 2000.
Now the Rcm come under top 10 direct selling multi-level marketing companies of India. Today Rcm is manufacturing around 730 products, having 8 million distributors and 1000 Pickup Centre all over the India.
Rcm Business currently manufacturing almost all types of products like health supplements and herbal medicines, food and grocery, clothing for children, women and men as well as a wide array of other stuff such as bags, stationery, tools and many more. This is all about the Rcm business, one should know before he or she join Rcm marketing plan 2021.
Guys earlier in Indian market, normal selling method is followed, where the final customers get exploited by the intermediators like selling agency, wholesaler, retailers. Looking for the welfare of society and for the benefits of the customers Sh. Trilok Chand Ji (owner and founder of Rcm business) transform their existing clothing company into Rcm business group owned by Trilok Chand Chhabra Ji at that time.
The motive of Rcm business was to start direct selling method in Indian Market. So, that the final customers need not to pay for wasteful expense like for product promotion, wholesaler’s and retailer’s profits and profit of selling agencies.
They add their profits to the product cost, as result low-cost products are provided to the final customers in a high cost. Why it is so? Let’s know its answer with the following example:
A XYZ company manufacture a product, whose manufacturing cost amounts up to Rs. 100. After that, when a company launch that product in the market, they need to do product promotion which amounts up to Rs. 50. After that product goes to the selling agency which add their profit.
Let’s assume they add Rs. 20 as their profit in the product cost. Now the product goes to wholesaler and then he will add his profit up to Rs. 20 and after that product goes to the retailer and he will also add his profit up to Rs. 10. After add all these cost the product reaches to the final customer.
Now product price which will customer need to pay for that product amounts Rs. 200 (Rs. 100 for manufacturing cost and company profit + Rs. 50 for product promotion + Rs. 20 as selling agency profit + Rs. 20 as wholesaler profit + Rs. 10 as retailer profit).
Guys, this is the big disadvantage of regular system which is followed by our Indian market. Rs. 100 amounting product is provided to the final customer in Rs. 200. You can easily see the drawback of this system.
Whereas on other hand is direct selling method is here under Rcm business plan. That’s the reason Trilok Chand Ji start a product based direct selling company, which is now manufacturing all kinds of products and providing them at a reasonable cost by eliminating the extra cost like product promotion cost, profits of selling agencies, wholesalers and retailers.
That’s why Rcm business is important for us. Rcm provides us all the product at a reasonable price with 100% purity. Rcm business plan or Rcm marketing plan 2021 also allow you to make some money by purchasing Rcm products, also it provides 3 types of other income like performance bonus, royalty bonus and technical bonus.
Why Do Rcm Business?
Guys, to know the answer of this question, first you should know what is Rcm business and what is the benefits of Rcm business plan. So, as discussed earlier Rcm business is a product based direct selling multi-level marketing company of India, which comes in top 10 list of direct selling MLM companies of India.
So, the answer for the question that why do Rcm business is Rcm provides us number of benefits like it provide us performance bonus, royalty bonus and technical bonus when you buy Rcm products and sell them to other customers and make others as Rcm business plan consultants under your downline. Let’s study about the Rcm business benefits in detail. Following are the benefits of Rcm business plan.
100% Pure Products: Rcm business provide you 100% pure products. Unlike to all other product available in the market which are adulterated and of low quality, Rcm provide you 100% pure and good quality products.
Retail Profit: One of the main benefits of Rcm Business plan 2021. You can buy the product from the Rcm pick up point at a discount rate up to 10-20% and then sell these products at M.R.P to other customers. In this way you earn profit which is known as retail profit.
Discount up to 10-20%: Under Rcm business plan 2021, you get the Rcm products at a discounted rate from the M.R.P. You get 10 to 20% of discount rate depending upon your BV (business volume).
Performance Bonus (up to 32%): Every product that you buy from the Rcm has BV points. BV stands for Business Volume. Yours and your groups BV points are added together in the end of the month and the commission is given to you as a performance bonus up to 32% depending up on your BV points. Further you have to distribute this commission with your group.
Royalty Bonus (up to 8%): Royalty Bonus is given up to 8% on the basis of your business volume points. Royalty Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021. Royalty is given on the basis of difference by deducting downline royalty from the total royalty. Royalty always calculated on monthly basis.
Technical Bonus (up to 5%): Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Also, he or she should be successfully earning the royalty income up to 8% percent for consecutive 3 months. Technical bonus is given on the basis of difference by deducting downline technical bonus from the total technical bonus.
How to do Rcm Business?
Guys, might you be now thinking that how you can take advantage of Rcm marketing plan 2021. So, we are here to tell you that how to do Rcm business to take earn the income under the Rcm marketing plan 2021.
First you need to join the Rcm marketing plan 2021. So, to join Rcm business go to its official website and fill the form to become a direct seller. In the direct seller form you will fill have to enter first sponsor number then proposer number and then some personal details, bank details and security details.
After that submit your form after uploading all the necessary documents. Once you join Rcm marketing plan then you need to buy minimum 2000 rupees Rcm products. Then in next step you need to sell these products to others through which you can also earn retail profit also.
After that you have to make your own group. You have to add other people on your downline. You have to convince other people to join the Rcm marketing plan 2021 under you.
That’s all you need to do to earn under Rcm marketing plan in Rcm business. You need to be patience because to earn under Rcm business plan and earn commission.
How Does Rcm business make Money?
Guys, under Rcm marketing plan 2021 you can earn multiple income. You can make money in Rcm business in the form of Retail profit, because once you join the Rcm business you get Rcm products at a discounted price and then you can sell these products to other people at M.P.R price and earn retail profit.
Another way to make money in Rcm business is earning commission in the form of Performance bonus. You get up to 32% of performance bonus depending upon your BV. BV stands for business volume.
You also get commission in the form of Royalty. You get royalty bonus up to 8% depending upon your BV. Royalty Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Another commission which is given to you is Technical Bonus. Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021.
Types of Income in Rcm Business?
Now guys, in this topic under Rcm business plan article, we will discuss about the income that you can earn under Rcm marketing plan 2021. Below listed are the types of income in Rcm business. Let’s understand these incomes in detail:
- Performance Income
BV stands for Business Volume. Every product that you buy from the Rcm has BV points. Yours and your groups BV points are added together in the end of the month and the commission is given to you as a performance bonus up to 32% depending up on your BV points. Further you have to distribute this commission with your group.
- Royalty Income
The royalty slab table is given below you can see from the table that how much percentage of royalty bonus you will earn on the basis of your BV.
- Technical Income
Technical Bonus is given up to 5% on the basis of your business volume points. Technical Bonus is given only to those Direct Sellers whose minimum purchase of Rcm products is 1500 BV on accrual basis in the respective month under Rcm business plan 2021. Also, he or she should be successfully earning the royalty income up to 8% percent for consecutive 3 months.
Technical bonus is given on the basis of difference by deducting downline technical bonus from the total technical bonus. Technical bonus is always calculated on monthly basis.
The technical slab table is given below you can see from the table that how much percentage of technical bonus you will earn on the basis of your BV.
Guys, once you join Rcm marketing plan then you need to buy minimum 2000 rupees Rcm products. Then in next step you need to sell these products to others through which you can also earn retail profit also.
After that you have to make your own group. You have to add other people on your downline. You have to convince other people to join the Rcm marketing plan under you.
Credit: https://www.jayrcm.com/RCM-business-plan & https://www.rcmbusiness.com/Home/MarketingPlan
Recent Posts
RCM- Frequently Asked Questions
RCM is a new concept, therefore so many questions arise in the minds of distributors. Some of these Frequently Asked Questions and their answers have been listed here. Visit : https://bndydvrcmbusines
RCM Pran Geet-प्राण गीत
RCM PRODUCT PRICE LIST 2021
RCM Business Plan
Nov 07, 2021
270 likes | 1.43k Views
RCM is one of the topmost MLM company in India. In this article, we have provided the latest RCM Business and Marketing Plan.
Share Presentation

Presentation Transcript
RCM Business Plan RCM has an undeniable Right Concept of Marketing, which goes under Fashion Suitings Private Limited and it is enlisted under RoCA-Jaipur, Rajasthan in April 1988 under MCA. RCM began its MLM plan in the year 2000, which is as yet running today. Karun Jain Cachar and Tilok Chand Chhabra are the current heads of this organization and have an office in Bhilwara, Rajasthan. RCM Company is the establishing individual from FDSA set up in 2011. FDSA Member Slant as of now has around 25 direct retailing organizations, with large designations like My Recharge, Mi Lifestyle, Ok Life Care, and AWPL. RCM is an item-based direct selling organization. Like some other MLM organizations, anybody can join RCM as an immediate dealer. RCM Direct Seller needs to complete 2 assignments, Product purchase It is actual important to purchase the product after joining RCM. It is simply after purchasing a product of Rs 1,000 that the sponsor gets the title and can work on the MLM plan further. Apart from this, direct sellers get the product at a lower price DP than MRP. According to this, you can earn retail profit by selling the direct seller product at MRP. Retail profit = MRP – DP Recruitment Another important assignment that an RCM direct seller has to do is recruitment. Below this, the direct seller will need to add others like him as direct cell RCM to his downline. RCM Income Plan Presently we will give you data about the RCM organization’s pay plan for example RCM Compensation Plan. In which you will discover how RCM gives cash to its immediate vendor and how much kind of pay is given by RCM. Kinds of Income in RCM RCM turns out three kinds of revenue to its immediate vendor, which are as per the following, Execution Bonus. Eminence Income. Specialized reward
- More by User
Business Plan
Business Plan. For the Alaska Inn Hotel & Restaurant . Presented by: Roberta. Alaska Inn. Alaskan beauty with the comfort of home. Alaska Inn P.O. Box 1185 Tel.1-800-555-4307 Fax. 907-555-1132 [email protected]. Alaska Inn. A hotel in Petersburg Alaska, with attached restaurant.
983 views • 18 slides
RCM Tools. Histogram Pareto Chart Cause and Effect Diagram FMEA. Histogram. A histogram is a of a bar chart representing the frequency of an entire data grouped into evenly spaced category. It can be viewed as a graph of class versus frequency. It used for the following:
823 views • 45 slides
Introduction. Solar energy.Executive SummaryCompany.Our Goals and vision. Project Objectives.Opportunities. Product
761 views • 33 slides
RCM Update. Fall, 2012. Guiding Principles.
365 views • 25 slides
Business Plan. Deel 4: Business Model. Business Model: definitie. De methode waarmee het bedrijf zijn middelen inzet om haar klanten een betere klantenwaarde te geven dan haar concurrenten … en daar ook nog een winst aan over te houden .
538 views • 28 slides
Business Plan. By: Revinda Aryandika U (7211413157) Ayu Fitriyani (7211413158) Dhesi Setiyarini (7211413171) I’ma Yayang D (7211413183). Aime Project. Vision . Excellent of the product. Mision . Our product. Target market. Marketing strategy . About Aime Project.
563 views • 14 slides
Business Plan . Business Plan . Les étapes Analyse stratégique & financière SWOT Analyse concurrentielle Orientation stratégique Analyse par activité du CAHT et marges Feuille de route Les étapes de la formalisation Budgets prévisionnels Par DAS (CA HT et marge)
864 views • 32 slides
The City. Restaurant. Business Plan. Life is a Journey…This is Your Destination. The City. Restaurant. Agenda. Introduction SWOT Analysis Operations Plan Marketing Plan Financial Plan Key Success Factors Summary. The City. Restaurant. Company Fact Sheet.
626 views • 20 slides
Business Plan. Ayu Ds (03) Hananto Adi (09). Meko Cupcakes. Tujuan kami mendirikan usaha.
379 views • 11 slides
Business Plan. Establishing our own business in Finland. Content. Idea of Business Personal aspects Questions to ourselves SWOT Analysis Location analysis Public acts Financing Conclusion. The Idea of our Business. Main idea:
286 views • 17 slides
BUSINESS PLAN
BUSINESS PLAN. Presented by Joshi 11pba207 Fr.Anto 11pba210 Michaline 11pba221 Arul jothi 11pba233 Edward 11pba240 Valarmathi 11pba242. “ P rint the flex in your heart ”. Tag Line:. VISION AND MISSION. The best and reliable flex printing unit in Tamil nadu.
353 views • 20 slides
Responsibility Center Management. RCM 401. David Proulx, Assistant Vice President for Financial Planning and Budgeting EMail: [email protected] Budget Office Website: http://www.unh.edu/budget RCM Website: http://www.unh.edu/rcm. RCM 401. Presentation Outline. 1. Overview
468 views • 26 slides
RCM - 2005. Seismic Resistance of RC -framed M asonry Wall System. Osamu JOH Professor, Dr of Eng. Graduate School of Engineering Hokkaido University. Turkey. Objective and Method. Objective:
221 views • 12 slides
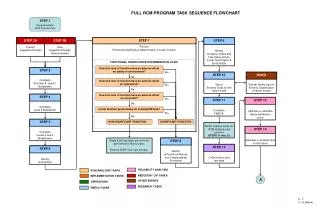
STEP 1 Develop/update RCM Program Plan
STEP 2 New Equipment Design Recommended. STEP 2B. STEP 3. Complete End Item & Level 1 Breakdown. SSWG. System Safety input to Severity Classification of failure modes. Select Severity Class for the failure mode. STEP 10. STEP 4. Complete Level 2 Breakdown.
212 views • 4 slides
NAVAIR RCM logistics.navair.navy.mil/rcm
R ELIABILITY C ENTERED M AINTENANCE. Management Overview. NAVAIR RCM http://logistics.navair.navy.mil/rcm. Objective.
1.34k views • 52 slides
Responsibility Center Management. RCM 401. David Proulx, Assistant Vice President for Financial Planning and Budgeting EMail: [email protected] Budget Office Website: http://www.unh.edu/budget RCM Website: http://www.unh.edu/rcm. RCM 401. Presentation Outline. 1. UNH Overview
391 views • 26 slides
Dynamic RCM
Dynamic RCM. OmegaPS R15.3.
974 views • 87 slides

Enterslice is a leader in business plan consultant in India. Get a professional business plan through Enterslice at just Rs. 69,999. https://enterslice.com/business-plan
530 views • 7 slides
286 views • 26 slides
158 views • 12 slides
275 views • 26 slides
Responsibility Center Management. RCM 401. David Proulx, Associate VP for Finance EMail : [email protected] Budget Office Website: http :// www.unh.edu/vpfa/budget RCM Website: http:// www.unh.edu/vpfa/rcm. RCM 401. Presentation Outline. 1. Overview 2. Allocation Methodologies
400 views • 30 slides
888.461.9998

- Medical Billing Services
- Medical Scheduling Software
- Medical Credentialing
- Medical Billing Audit
- Medical Coding Service
- Medical Coding Audit
- Denial Management
- Document Indexing
- Client Server Based EHR
- Customizable Specialty Solutions
- Mobile Solutions
- MACRA / MIPS
- Real Time Prescription Benefit
- Online Payments
- Medical Speech Recognition
- Patient Portal
- Telemedicine
- Appointment Reminders
- Practice Managers
- New Practices
- Your Specialty
- Interoperability
- EHR Optimization
- EHR Replacement
- Patient Engagement
- Revenue Cycle Management
- Blog Articles
- Knowledge Resources
- Video Library
Revenue Cycle Management (RCM)
Posted by: Alok Prasad
Updated on: 07.14.2024

Blog -> Revenue Cycle Management (RCM)
Optimizes Patient Service Revenue and minimizes Claim Denials
Recent developments in the operating environment of medical practices have resulted in several changes that have made managing the revenue cycle even more important, including:
Increased regulatory oversight: Implementing new regulations, such as the Affordable Care Act and HIPAA, have added complexity to the billing and collections process, making it more important for practices to stay compliant.
Shift towards value-based care: The move towards value-based care models has increased the importance of accurate and timely billing and collections, as reimbursement is tied to the quality of care.
Growing patient financial responsibility: With the rise of high-deductible health plans, patients are now responsible for a larger portion of their healthcare costs, making it more important for practices to bill and collect accurately.
Technological advancements: Technology advancements have enabled practices to automate many of the manual processes involved in RCM, making it easier to manage the revenue cycle more efficiently.
To summarize, the operating environment has seen several changes that have increased the importance of effectively managing the revenue cycle in modern medical practices. Healthcare organizations and medical practices must learn to optimize their revenue cycle while delivering optimal patient care and succeeding as a business entity.
What is RCM?

Revenue Cycle Management (RCM) is a financial process that enables a healthcare practice to optimize total patient service revenue generated by streamlining billing, accelerating the revenue cycle, and reducing billing errors and revenue leakage. RCM is crucial for improving the patient experience, ensuring accurate and timely service reimbursement, and maintaining a stable financial position.
Unlock the benefits of Revenue Cycle Management (RCM) and experience a positive impact on your practice.
Improved Cash Flow : By reducing the time it takes to receive payment for services, practices experience improved overall cash flow.
Increased Revenue : By ensuring that claims are processed accurately and efficiently, practices reduce claim denials and improve the likelihood of full payment for services rendered.
Enhanced Patient Experience : By reducing billing errors and streamlining the payment process, providers can provide a more positive patient experience.
Enhanced Compliance : By ensuring that medical practices comply with healthcare regulations, they can reduce the risk of financial penalties and legal issues.
Improved Efficiency : By automating many of the manual processes involved in RCM, practices can save time and resources and focus on delivering high-quality patient care.
Better Data Management : By improving data accuracy and organization, practice management teams can provide valuable insights into practice performance and enable better decision-making.

Internal and External Factors
Multiple elements influence a practice’s revenue. Some of these are internal and can be controlled by the practice. However, several are external and outside of the practice’s control.
Internal Drivers
Internal revenue drivers include the fees the practice charges for certain services, procedures, and treatments. They also include the make-up of the patient base served by the practice, such as the number of patients, health status or conditions, frequency of seeking treatment, and the physicians’ capacity to see patients and deliver the necessary care. Front and back-office workflow and staff skills also drive revenue to some extent.
External Drivers
These drivers include patient and insurance payer payments, presenting a more significant challenge. External drivers also include healthcare regulations and reimbursement schemes.
Having a process for collecting payments for services that have already been provided is a simple and intuitive way of doing business. However, practices can only sometimes successfully manage some or all aspects of this process. Real challenges exist in the effective execution of revenue cycle management, some of which are unique to the U.S. healthcare industry.
1. Healthcare regulations and reimbursement models
One of the biggest challenges in revenue cycle management is the ever-changing healthcare regulations and complex reimbursement models introduced every few years. Practices must stay abreast of these changes and ensure that their staff understands them and performs their tasks in compliance with these regulations. Expertise in all aspects of the change may take much work, especially for smaller practices.
2. Collecting payment from patients
With the new regulations and the rise of consumerism, patients are increasingly responsible for more healthcare costs. Practices must master the balancing act of collecting patient payments while not resorting to “high-pressure sales tactics” that may turn off patients and cause them to seek care elsewhere. This situation can be avoided by continuously educating staff and patients regarding payment workflows and expectations and establishing alternative payment methods, including payment plans and online payment.
3. Tracking a claim through its entire cycle
If a process is not established for monitoring claims, errors or delays may not be easily identified and resolved, resulting in lost revenue.
4. Denial management
Having claims denied is frustrating and impacts a practice’s bottom line. Each denial increases the risk of a practice not getting paid for services rendered. The high percentage of denials (14%) and never refiled claims (50%) represent a significant chunk of revenue that practices are leaving on the table. An effective denial management plan involves insurance follow-up services and AR (accounts receivable) management to improve payment chances.
5. Staff training
Each staff member involved in the revenue management cycle must be properly trained in the policies, procedures, and workflow. Adequate, effective staff training might be time-consuming and involve costs, but it pays off when knowledgeable staff members know their roles and functions and perform them correctly and efficiently.
How to Optimize the Healthcare Revenue Cycle?
Given the challenges mentioned above, these key elements boost the success of an organization’s revenue cycle:
High-quality patient outcomes resulting from exceptional care delivery and patient engagement help expand the patient base and lower costs, thus increasing revenue.
Financial policies and procedures addressing issues such as unpaid balances help guide both staff and patients. This policy emphasizes pre-registering patients , posting charges as soon as possible, and other matters.
A well-trained staff provides the backbone for a successful practice. The team includes front and back offices, clinicians, certified medical coders, and others. In addition to proficiency in their specific jobs, the staff needs to understand their role in the revenue cycle process and how they can enhance and improve the process.
An efficient process that moves the claim through its life cycle without errors or delays allows practices to collect the cash they need and deserve.
Technology Products
Appropriately and effectively using technology solutions improves patient care, enhances accuracy, automates and streamlines repetitive or tedious processes, and increases staff productivity.
Here are some ways technology supports and enables an optimized revenue cycle process.
1. Front Office
- Patient scheduling and registration, as well as patient reminders, can be done via a patient portal.
- Insurance eligibility verification can be automated.
- Practices can accept and process credit cards, HSAs, and FSAs for co-pays, co-insurance, and deductibles.
2. Patient visit
- Clinical care delivery, charge capture, and charge entry are documented in the EHR/EMR
3. Back office
- Medical transcription, medical coding, and claim submissions are enabled by technology.
- Reports and analytics provide insights into how well a practice performs in terms of key performance indicators.
- Patient payment can be made online via a payment portal.
- Posting of payments can be automated.
- Best Practices
Ever-changing healthcare regulations and reimbursement models have made it incumbent upon medical practices to be increasingly responsible for optimizing payment collections and all other aspects of healthcare RCM. While there are indeed many significant challenges, implementing best practices maximizes collections. Further, it reduces costs at each phase of the revenue cycle and helps small practices better understand, measure, and control their financial aspects.
1. Optimize front office processes and collections
Train your front staff to gather the patient's demographic and insurance information during appointment scheduling. Use “communication scripts” to help staff explain the co-pay collection and the various payment methods or plans available to patients. A well-trained front office staff contributes to both revenue optimization and patient satisfaction.
2. Automate insurance eligibility verification
Automating insurance eligibility verification helps both the practice and the patients. It has the dual advantage of preventing claim errors and informing patients early on regarding payment responsibilities. The increased transparency helps patients plan for out-of-pocket payments and more readily respond when front-office staff collects these payments.
3. Customized EMR Templates
Use and customize EMR templates to efficiently capture clinical documentation and charge data. Remind clinicians to document completely and accurately and set up a review process to help them identify areas for improvement.
4. Integrated EHR and Practice Management Software
Use an EMR/EHR integrated with your practice management system when possible. Data can be pushed automatically and seamlessly downstream, which helps reduce errors and delays.
5. Back Office-Related Best Practices
- Use technology to automate key aspects of your claim submission process. Use e-remittance to speed up payment turn-around time.
- Provide an online payment portal allowing patients to make payments not collected during an in-person visit conveniently.
- Improve cash flow by effectively managing your insurance follow-up and claims denial processes.
- Use reports and data analytics to monitor revenue goals and visualize areas for improvement.
- Evaluate and implement software solutions for various aspects of revenue cycle management that meet the practice’s needs. The right software solution for the right process enables physicians to focus on patient care instead of worrying about payments.
- Consider outsourcing your RCM processes to a comprehensive and integrated solution vendor. Practices that don’t have the time or staffing resources to internally acquire the necessary knowledge and expertise of all the aspects of revenue cycle management may find this option feasible and advantageous. According to Becker’s Hospital Review , “seventy-two percent of hospital CFOs consider end-to-end RCM outsourcing the best option until value-based payment models are better established.”
6. Electronic Prior authorization
Prior authorization ensures that a patient's insurance plan covers the proposed medical services before they are provided. This helps to avoid denied claims, reduce payment delays, and improve overall financial stability for healthcare providers. Pre-authorization also helps maintain compliance with payer requirements and enhances patient satisfaction by clarifying coverage and costs upfront.
How can Artificial Intelligence Improve RCM?
Artificial intelligence (AI) is revolutionizing Revenue Cycle Management (RCM) by automating and optimizing various processes to enhance efficiency, accuracy, and profitability.
- One critical improvement AI brings to RCM is the automation of claims processing. By utilizing advanced algorithms and machine learning models, AI systems can swiftly and accurately process claims, reducing the chances of human error and significantly decreasing the time required for claim adjudication. This leads to faster reimbursements and improved cash flow for healthcare providers.
- AI is also making a substantial impact in reducing claim denials. AI-powered systems can analyze vast amounts of data to identify patterns and predict potential issues that may lead to denials. By flagging these issues before claims are submitted, healthcare providers can take corrective actions, increasing the likelihood of successful claim approvals. This proactive approach reduces the administrative burden associated with reworking denied claims and ensures a steady revenue stream.
- AI can also enhance the accuracy of coding and billing processes. Natural language processing (NLP) and machine learning techniques can extract relevant information from clinical documentation and ensure the correct codes are assigned. This minimizes coding errors and ensures compliance with regulatory requirements, reducing the risk of audits and penalties.
- AI-driven analytics also play a crucial role in strategic decision-making. By analyzing historical data and identifying trends, AI can provide actionable insights into revenue cycle performance, helping organizations optimize processes, allocate resources more effectively, and make informed financial decisions.
In summary, AI can transform RCM by automating routine tasks, improving accuracy, reducing denials, and providing valuable insights, ultimately enhancing healthcare organizations' financial performance.
Healthcare regulations, reimbursement models, and technology have been changing rapidly. This presents formidable challenges for healthcare organizations to maintain their financial viability. A well-thought-out and robust revenue cycle management strategy can differentiate between practices struggling to survive and those that succeed and prosper.
Practices that automate where appropriate and streamline when necessary gain an advantage over those mired in tedious and time-consuming tasks that do not provide the desired outcome—maximum payment for rendered services as soon as possible.
It is more crucial than ever for practices to assess their need for robust and reliable revenue cycle management solutions . RevenueXL has flexible solutions for a variety of needs. We offer individual or integrated tools that support your overall revenue cycle management strategy. Contact us today to discuss how we can help.
Commonly Used Terminology
When thinking about the Revenue Cycle, it would be helpful to know some commonly-used terms:
- ACO - CMS defines an Accountable Care Organization (ACO) as a group of doctors, hospitals, and other healthcare providers who come together voluntarily to give coordinated, high-quality care to their Medicare patients. Coordinated care aims to ensure that patients get the right care at the right time while avoiding unnecessary duplication of services and preventing medical errors.
- Alternative payment models (APMs) – APM is a model of payment that gives incentives for high-quality care instead of the number of services or treatments provided
- Bundled payments – These payments are either “fixed-rate” or “flat-rate” pricing structures for treating certain conditions based on the expected costs of associated services.
- MACRA - The Medicare Access and CHIP Reauthorization Act of 2015 is a law signed on April 16, 2015, and replaces the Sustainable Growth Formula. It rewards clinicians for value over volume, streamlines multiple programs under MIPS, and gives bonuses for participation in APMs.
- Medicare Shared Savings Program – This program is a voluntary CMS program that offers providers and suppliers such as physicians, hospitals, and others involved in patient care an opportunity to band together as an ACO.
- MIPS – The Merit-Based Incentive Program began in 2019. MIPS streamlines three independent programs to work as one to ease the clinician’s burden. It also adds a fourth component to promote ongoing improvement and innovation in clinical activities. It allows clinicians to choose the activities and measures most meaningful to their practice to demonstrate performance.
- Value-based reimbursement – This refers to payments that Medicare, Medicaid, and other payers tie to the quality of care provided or patient outcomes. They are intended to incentivize care providers to focus on quality, lower costs, and inefficiencies.
Topics: Medical Billing , Consultant , Practice Manager
Are you unhappy with your EHR Software?
Our award-winning software and services streamline your practice and help you make more revenue...faster.
Cloud-based, HIPAA compliant, Meaningful Use Certified EHR, Telemedicine and lot more..

- About RevenueXL
RevenueXL is a provider of healthcare solutions with 15+ years of expertise in process knowledge, cutting edge technology and a team of experts in various facets of practice management.
We help small practices accelerate their growth whether using the features bundled in our award winning software or our tailored services.
- We specialize in providing custom solutions.
- We value customer relationships and become partners.
- We help streamline your practice and patient flow.
- We are flexible, agile and adapt to new changes.

- There are no suggestions because the search field is empty.

Related Posts
Ehr vendor selection criteria | ehr selection process, what is mips, providers: mobile healthcare revolution can change your life. adopt it., finding a replacement ehr software - some do's and don'ts, ehr replacement - 9 signs that it is time to make the switch, streamline your small practice with customized solutions, ehr software, practice management, telemedicine, patient engagement, credentialing, medical billing services, denial management, coding compliance and audit.

EHR Vendor Selection Guide For Small Medical Practices Successful implementation of medical EHR software can only be achieved by following a sound...
Learn More about Merit-Based Incentive Payment System MIPS or Merit-Based Incentive Payment System is a program that falls under the Quality Payment...
There’s no doubt that mobile healthcare—often referred to as mHealth—has the ability to transform healthcare as we know it. Mobile health technology,...
Ready to Transform Your Practice?

- Practice Management
- Medical Billing Software
- EHR Software
- E-Prescribing
Learning Center
- EHR Interoperability
- Industry Blog
- Pediatric Resources
- Orthopedic Resources
- Frequently Asked Questions
Our Company
- Contact RevenueXL
© 2021 RevenueXL Inc. All rights reserved. Unauthorized Reproduction Prohibited - Legal Notice.
Privacy Policy | Site Map
Download Rcm Business - The New Marketing Plan Book

- Date: October 2019
- Size: 66.4MB
- Author: Samir K Mishra
This document was uploaded by user and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this DMCA report form. Report DMCA
This is a non-profit website to share the knowledge. To maintain this website, we need your help. A small donation will help us alot.
Copyright © 2024 IDOCPUB.

IMAGES
VIDEO
COMMENTS
The U.S. revenue cycle management market size was worth USD 64.13 billion in 2022 and is projected to grow at a CAGR of 10.7% during the forecast period. Revenue cycle management (RCM) is a healthcare process implemented to maintain a complete record of patient expenses from admissions to discharge. This process streamlines the business ...
The global revenue cycle management market size was valued at USD 135.92 billion in 2023 and is projected to grow from USD 148.84 billion in 2024 to USD 361.86 billion by 2032, exhibiting a CAGR of 11.7% during the forecast period (2024-2032). Today's healthcare systems face major challenges such as increasing complexity, rising treatment ...
Market Size & Trends. The U.S. revenue cycle management market size was estimated at USD 155.59 billion in 2023 and is projected to grow at a CAGR of 10.18% from 2024 to 2030. The rapidly transforming healthcare system, including digitalization, has paved the path for implementing healthcare IT services such as Revenue Cycle Management (RCM ...
Revenue cycle management (RCM) is the process of converting care delivery into cash. At its most comprehensive, services include: payment capture (payment processing, denials, customer service and collections). Effective RCM is challenging because of: Evolving regulations (e.g., all the Covid emergency measures).
Cheap Product along with Bill for every single purchase. Rcm Business Plan provides a fare bill of even one rupee of purchase is made. Under Rcm marketing plan 2021 you get 10-20 percent discount. 10-32 percent performance bonus in your bank account, 3-8 percent royalty income generation, 1-5 percent technical income.
On January 6, 2021, R1 announced that it has entered into an agreement for the conversion of preferred stock held by Ascension and TowerBrook to common stock. As part of the agreement, the holders will receive: 139.3 million common shares. A one-time cash payment of $105 million, funded with cash from balance sheet.
The RCM Business Process Transformation 2021 RadarView highlights the key outsourcing trends in the RCM space and Avasant's viewpoint on them. It aids companies in identifying top service providers to assist them in transforming their RCM operations. It also offers an analysis of each service providers' capabilities in technology, domain ...
The global revenue cycle management market was valued at $109.5 billion in 2021, and is projected to reach $367.7 billion by 2031, growing at a CAGR of 13.2% from 2022 to 2031. The supportive growth through regulatory compliance has increased the need for revenue cycle management. In addition, the growing demand for workflow optimization in ...
business model to the level of site and individual physician performance (by payor mix, ordering volume, reimbursement, etc.) but also provides you with the metrics you need to evaluate how efficiently RCM is managing your revenue cycle. RCM Enterprise Services. Your choice for Revenue Cycle Management.
Hallmark Health System, a charitable health service provider with over 700 physicians, leveraged Optum360 solutions for RCM. Its revenue increased by USD 1.3M and unbilled A/R reduced by over USD 8M. Additionally, its physician query response rate reached over 90%. KentuckyOne Health Medical Group partnered with Optum to streamline its revenue ...
6 key RCM company business moves in 2021. From mergers to acquisitions to new leaders, here are six key moves healthcare revenue cycle management companies made in 2021: Gulf Capital acquired two ...
Benefits of AI in Revenue Cycle Management. The benefits of AI in RCM include improved efficiency, accuracy, patient experience and team satisfaction. In addition, employees can rely on artificial intelligence to simplify time-consuming tasks and focus more on critical thinking and troubleshooting.
The size of global revenue cycle management market in terms of revenue was estimated to be worth $49.6 billion in 2023 and is poised to reach $84.1 billion by 2028, growing at a CAGR of 11.1% from 2023 to 2028. The comprehensive research encompasses an exhaustive examination of industry trends, meticulous pricing analysis, patent scrutiny ...
rcm business new marketing plan July 2021 lunch and first time in YouTubePlease Like subscribe and share forward to allDirect download link https://rcmbusine...
Chapter 7 Revenue Cycle Management (RCM) Market: End-use Estimates & Trend Analysis 7.1 Market: End-use Movement Analysis, USD Million, 2021 & 2030 7.2 Physician Offices
Today I will share New RCM Business Plan 2021.This video teaching you, How to success in life. RCM NABA DIGANTA.Facebook page linkhttps://www.facebook.com/Na...
Global Revenue Cycle Management (RCM) Market Opportunity Analysis and Industry Forecasts, 2020-2021 & 2022-2030 - ResearchAndMarkets.com May 25, 2022 07:24 AM Eastern Daylight Time
#vishalkhatwani #rcmbusiness*****Subscribe our channelचैनल को सब्सक्राइब कीजिए :https://youtube.com/channel/UC3 ...
RCM Business Plan. MyListingMart · Follow. 2 min read · Oct 26, 2021 ...
NEW YORK, Aug. 1, 2023 /PRNewswire/ -- The revenue cycle management (RCM) market in the US is set to grow by USD 11,985.2 million from 2022 to 2027 progressing at a CAGR of 9.94% during the ...
RCM Business plan also provides fare bill for purchase of Re. If you buy RCM Marketing Plan 2021 then you will get 10-20% discount. You will have 10-32 percent off performance bonus, 3-8 percent in royalty income and 1-5 percent in technical income in your bank account.
The revenue cycle management (RCM) market in the US is set to grow by USD 11,985.2 million from 2022 to 2027 progressing at a CAGR of 9.94% during the forecast period. The report offers an up-to ...
Discount up to 10-20%: Under Rcm business plan 2021, you get the Rcm products at a discounted rate from the M.R.P. You get 10 to 20% of discount rate depending upon your BV (business volume). Performance Bonus (up to 32%): Every product that you buy from the Rcm has BV points. BV stands for Business Volume.
RCM Business Plan RCM has an undeniable Right Concept of Marketing, which goes under Fashion Suitings Private Limited and it is enlisted under RoCA-Jaipur, Rajasthan in April 1988 under MCA. RCM began its MLM plan in the year 2000, which is as yet running today. Karun Jain Cachar and Tilok Chand Chhabra are the current heads of this organization and have an office in Bhilwara, Rajasthan.
Revenue Cycle Management (RCM) is a financial process that enables a healthcare practice to optimize total patient service revenue generated by streamlining billing, accelerating the revenue cycle, and reducing billing errors and revenue leakage. RCM is crucial for improving the patient experience, ensuring accurate and timely service ...
Download Rcm Business - The New Marketing Plan Book. Type: PDF. Date: October 2019. Size: 66.4MB. Author: Samir K Mishra. This document was uploaded by user and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this DMCA report form.