- Research article
- Open access
- Published: 29 February 2024

The effectiveness, implementation, and experiences of peer support approaches for mental health: a systematic umbrella review
- Ruth E. Cooper 1 na1 ,
- Katherine R. K. Saunders 1 na1 ,
- Anna Greenburgh 2 ,
- Prisha Shah 6 ,
- Rebecca Appleton 2 ,
- Karen Machin 6 ,
- Tamar Jeynes 6 ,
- Phoebe Barnett 2 , 3 , 4 ,
- Sophie M. Allan 2 , 5 ,
- Jessica Griffiths 1 ,
- Ruth Stuart 1 ,
- Lizzie Mitchell 6 ,
- Beverley Chipp 6 ,
- Stephen Jeffreys 6 ,
- Brynmor Lloyd-Evans 2 ,
- Alan Simpson 1 , 7 &
- Sonia Johnson 2 , 8
BMC Medicine volume 22 , Article number: 72 ( 2024 ) Cite this article
8458 Accesses
2 Citations
26 Altmetric
Metrics details
Peer support for mental health is recommended across international policy guidance and provision. Our systematic umbrella review summarises evidence on the effectiveness, implementation, and experiences of paid peer support approaches for mental health.
We searched MEDLINE, EMBASE, PsycINFO, The Campbell Collaboration, and The Cochrane Database of Systematic Reviews (2012–2022) for reviews of paid peer support interventions for mental health. The AMSTAR2 assessed quality. Results were synthesised narratively, with implementation reported using the CFIR (Consolidated Framework for Implementation Research). The protocol was registered with PROSPERO (registration number: CRD42022362099).
We included 35 reviews (426 primary studies, n = 95–40,927 participants): systematic reviews with ( n = 13) or without ( n = 13) meta-analysis, or with qualitative synthesis ( n = 3), scoping reviews ( n = 6). Most reviews were low or critically low (97%) quality, one review was high quality. Effectiveness was investigated in 23 reviews. Results were mixed; there was some evidence from meta-analyses that peer support may improve depression symptoms (particularly perinatal depression), self-efficacy, and recovery. Factors promoting successful implementation, investigated in 9 reviews, included adequate training and supervision, a recovery-oriented workplace, strong leadership, and a supportive and trusting workplace culture with effective collaboration. Barriers included lack of time, resources and funding, and lack of recognised peer support worker (PSW) certification. Experiences of peer support were explored in 11 reviews, with 3 overarching themes: (i) what the PSW role can bring, including recovery and improved wellbeing for service users and PSWs; (ii) confusion over the PSW role, including role ambiguity and unclear boundaries; and (iii) organisational challenges and impact, including low pay, negative non-peer staff attitudes, and lack of support and training.
Conclusions
Peer support may be effective at improving some clinical outcomes, self-efficacy, and recovery. Certain populations, e.g. perinatal populations, may especially benefit from peer support. Potential strategies to successfully implement PSWs include co-production, clearly defined PSW roles, a receptive hierarchical structure and staff, appropriate PSW and staff training with clinical and/or peer supervision alongside safeguarding. Services could benefit from clear, coproduced, setting specific implementation guidelines for PSW. PSW roles tend to be poorly defined and associations between PSW intervention content and impacts need further investigation. Future research should reflect the priorities of providers/service users involved in peer support.
Peer Review reports
Peer support in mental health care is a recovery-orientated approach delivered by individuals who have lived experience of mental health difficulties (as service users, carers, parents or supporters). Peer support workers (PSWs) are employed to draw on these experiences to support mental health service users or carers of people with mental health conditions [ 1 , 2 ]. As such, PSWs are uniquely positioned to facilitate recovery through empathic engagement with service users and their support networks. The success of peer support is thought to be based in the sharing of lived experiences and mental health knowledge and through interpersonal connection [ 3 , 4 ]. Across diagnoses, peer support may promote recovery through the modelling of coping strategies, and by providing hope and an example of recovery to those dealing with mental health difficulties [ 5 ].
Peer support has been utilised across various populations and types of service, for example in services for early intervention in psychosis [ 6 ], for people with co-occurring substance abuse and mental health difficulties [ 7 ], and in community interventions to reduce mental health inpatient admissions [ 8 ]. The format of peer support varies across services, for example it may involve one-to-one or group sessions, online or face-to-face delivery, unstructured open-ended conversations or more structured manualised support, or activities such as walking groups [ 9 , 10 ]. Peer support may be delivered by trained peer support staff or on a more ad hoc basis among peers [ 11 ]. Peer support for mental health takes place within mental health services in both statutory and voluntary sector settings [ 11 ]. Although PSWs may be paid or unpaid [ 6 , 12 ], paid roles have become increasingly available in mental health care settings [ 13 ]. Professionalising PSW roles as paid demonstrates the value of the role and appropriately rewards work done, should ensure formal training, supervision and management, and may help to clarify the boundaries of the role [ 14 ].
Service user networks and researchers in relevant fields have strongly advocated for provision of peer support [ 14 , 15 ], and peer support is now recognised and recommended across international mental health policy guidance, reflecting an increased understanding of the value of embedding lived experience support in formal mental health services [ 16 , 17 , 18 , 19 , 20 ]. In the UK, peer support is currently being expanded in the NHS [ 16 ].
There have been many reviews of the peer support literature separately evaluating the efficacy, implementation, and experiences of peer support from a variety of different perspectives (e.g. [ 21 , 22 , 23 , 24 ]). Given the numerous and sometimes inconclusive results from existing reviews on this topic, our research group, the NIHR Mental Health Policy Research Unit, agreed with policy makers in England to conduct an umbrella review of peer support to provide clinicians, policy makers and researchers with an overall assessment on the evidence available, comparing results between reviews, while taking the quality of these reviews into account [ 25 , 26 ]. The aim of this systematic umbrella review is to collate, synthesise and summarise the available evidence from published reviews to address the following research questions:
What is the effectiveness (e.g. clinical, social, functional) and cost-effectiveness of paid peer support approaches for mental health?
What influences the implementation of peer support approaches for mental health?
What are the experiences of peer support approaches for mental health (e.g. of acceptability) from the perspective of PSWs, healthcare practitioners, service users, carers?
This umbrella review was conducted by the NIHR Mental Health Policy Research Unit (MHPRU), based at King’s College London and University College London, which delivers evidence to inform government and NHS policy in England, agreeing a programme of rapid research with policymakers.
Study design and protocol
We conducted a systematic umbrella review following guidance from Fusar-Poli et al. [ 27 ] and Cochrane [ 28 ]. The review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (see Additional file 1 : Appendix 1 for the PRISMA checklist) [ 29 ]. The protocol was registered with PROSPERO (registration number: CRD42022362099) [ 30 ]. One amendment was made to the protocol after registration. We amended the ‘intervention’ section to state that reviews were excluded if the majority of interventions did not meet eligibility criteria, e.g. because we found that reviews often included paid and unpaid peer support interventions and did not report results separately.
Lived experience researcher involvement
Members of the MHPRU Lived Experience Working Group (LEWG), who collectively have substantial experience of delivering or receiving peer support, contributed extensively to this review, including protocol development, study selection, data extraction, quality appraisal, data synthesis, drafting the manuscript and lived experience commentary, and attending working group meetings.
Eligibility criteria
The eligibility criteria are detailed in full in the protocol [ 30 ]. In summary, we included:
Study designs : Published, peer-reviewed systematic, scoping or realist reviews which synthesised quantitative or qualitative data (narratively or formally using, e.g. a meta-analysis or meta-synthesis) that examined outcomes or experiences relevant to our research questions.
Intervention : We defined peer support as ‘involving a person who has lived experience of mental health condition(s), or caring for those with mental health conditions, being employed to use and draw on their experiences and empathy to support service users who have mental health conditions or carers or parents of people with mental health conditions.’ Eligible peer support approaches were paid, meaning that the PSW was paid for their work, and delivered face-to-face or remotely, for people with mental health conditions or for carers of people with mental health conditions, across any mental healthcare settings. Peer support approaches were ineligible if the PSWs were not in a dedicated peer support role, if they were primarily for physical health, or automated (i.e. peer support ‘bots’ or avatars). We excluded reviews where over 50% of primary studies in the review did not meet eligibility criteria, e.g. if the majority of people delivering the interventions were unpaid.
Population : Children, young people and adults with a mental health condition (including substance use disorders), carers, paid PSWs and mental healthcare practitioners working alongside PSWs. We excluded service users with a primary diagnosis of an organic mental disorder (e.g. dementia), neurodevelopmental disorders, acquired cognitive impairment and adjustment disorders.
Outcome measures : Included reviews reported outcomes or data on at least one of the following peer support related outcomes that addressed our research questions: (i) clinical outcomes, (ii) economic or cost-effectiveness, (iii) recovery outcomes, e.g. hope, empowerment, goal-attainment, quality of life, (iv) social outcomes, (v) implementation outcomes and barriers and facilitators to implementation, (vi) experiences of delivering, receiving or working alongside peer support and (vii) theories of what works for whom in peer support.
Information sources and search strategy
We combined terms for peer support, reviews and mental health conditions using Boolean operators (AND, OR). We searched the following databases: MEDLINE, EMBASE, PsycINFO, The Campbell Collaboration and The Cochrane Database of Systematic Reviews (see Additional file 1 : Appendix 2 for full search strategy). Searches were run from January 2012 to November 2022 as these reviews will include primary research published before 2012 [ 31 ]. There was no time limit for the primary papers in the included reviews. We had no language restrictions.
Selection process
Reviewers (KS, RC, JG, RS, RA, KM, PS, SA) screened titles and abstracts, and subsequently full texts. To ensure consistent application of eligibility criteria all reviewers initially independently screened the same ten titles and abstracts and discussed inclusion/exclusion. The remaining titles and abstracts were then screened. Records were double screened blind by two reviewers at both the title and abstract (94% agreement) and full text (86% agreement) stages. All disagreements were resolved through discussion with the study team.
Data extraction
Data extraction was completed in Microsoft Excel by the review team (RC, KS, KM, PS, JG, RS, PB, RA). The data used in the paper were checked by another member of the review team. The extracted data included basic information about reviews (e.g. number of included studies, number of participants, review type, aim/objectives), basic information about primary studies (e.g. references, designs), search strategy (e.g. databases searched, eligibility criteria), population (e.g. gender, age), peer support approach (e.g. peer support type and description), type of comparator, additional information (e.g. quality appraisal methods, review author conclusions), primary and secondary outcomes of systematic review or qualitative results.
Quality appraisal of included reviews
The quality of included reviews was independently assessed by reviewers (RC, KS, KM, PS, JG, RS, PB, RA) using the AMSTAR 2 (A MeaSurement Tool to Assess systematic Reviews), a 16-point tool for assessment of the methodological quality of systematic reviews [ 32 ]. We adapted the AMSTAR 2 to apply for scoping reviews and systematic reviews of qualitative data (described in full in Additional file 1 : Appendix 3). The following questions were adapted: (1) PICO criteria, (2) Protocol requirements, (8) Detail of included studies, (9) Risk of Bias requirement. Two reviewers (KS, AG) 100% double-scored reviews blind with any outstanding disagreements resolved through discussion between AG, KS, and RC. Overall ratings for each study were calculated according to guidance [ 32 ], based on 7 critical domains and 6 non-critical domains within the AMSTAR 2 tool. Studies with no or one non-critical weakness and no critical flaws were rated as high quality. Studies with more than one non-critical weakness and no critical weaknesses were rated as moderate quality. Studies with one critical flaw irrespective of non-critical weaknesses were rated as low quality, and those with more than one critical flaw irrespective of non-critical weaknesses were rated as critically low quality. The AMSTAR 2 guidance [ 32 ] states that reviews of critically low quality should not be relied on for comprehensive and accurate summaries of the literature.
Synthesis methods
Rq 1: what is the effectiveness (e.g. clinical, social, functional) and cost-effectiveness of paid peer support approaches for mental health.
Data were tabulated and summarised narratively by two researchers (KS, AG); effectiveness meta-analysis data calculated from two or more studies were tabulated separately from non-meta-analysis effectiveness outcomes. Review outcomes were similar, but not similar enough to combine meaningfully in a meta-analysis. Effect sizes (with 95% CIs and p -values) were reported along with I 2 statistic (with 95% CIs, p -values, χ 2 , and degrees of freedom) where available. We did not tabulate data for subgroup analyses.
RQ 2: What influences the implementation of peer support approaches for mental health?
Outcomes were tabulated according to the main domains in the Consolidated Framework for Implementation Research (CFIR) [ 33 ]. The CFIR provides a comprehensive framework, composed of 5 domains, associated with the effective implementation of interventions [ 33 ]. The 5 domains are as follows: Innovation (the ‘thing’ being implemented); Outer setting (the setting in which the inner setting exists, e.g. hospital system); Inner setting (the setting in which the innovation is implemented, e.g. hospital); Individuals (the roles and characteristics of individuals); Implementation process (the activities and strategies used to implement the innovation) [ 33 ]. Synthesis was conducted using a collaborative process involving one member of the study team (RA) and one lived experience researcher (PS).
RQ 3: What are the experiences of peer support approaches for mental health (e.g. of acceptability) from the perspective of PSWs, healthcare practitioners, service users and carers?
Experiences were synthesised narratively, by three researchers, including two lived experience researchers (TJ, KM, RC) [ 34 ]. Themes from reviews which were identified as addressing research question 3 were extracted and similar themes across the reviews were grouped together. Each group was accounted for using an existing theme from one or more of the reviews or if this was not possible a new theme was developed. Three overarching themes were identified through iterative scrutiny of the data and discussion between TJ, KM, and RC. A summary of the common themes across the reviews, grouped under the three overarching themes, was then developed, including highlighting contrasting findings.
Study selection
The search strategy identified 777 references to be screened (a further 2 papers were identified through other methods); 93 full text articles were assessed for eligibility with 57 excluded (see Additional file 1 : Appendix 4 for reasons for exclusion). Thirty-five reviews (reported in 36 papers) were included (see Fig. 1 ).
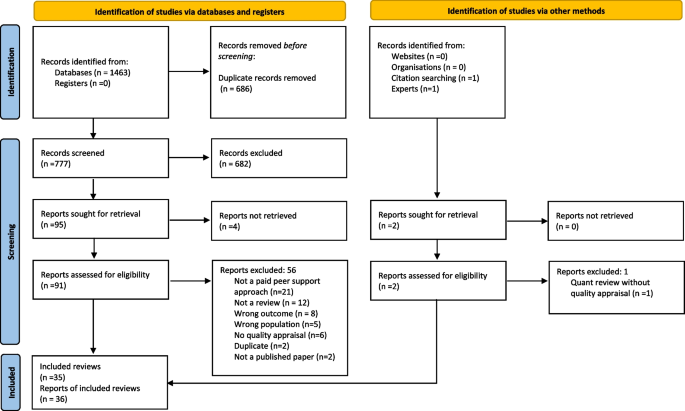
PRISMA flow diagram [ 29 ]
Characteristics of included reviews
Review characteristics are detailed in Table 1 . Of the 35 included reviews, 13 were systematic reviews with meta-analyses, 13 were systematic reviews without meta-analyses, 3 were systematic reviews with a qualitative synthesis and 6 were scoping reviews. The individual reviews included between 95 and 40,927 participants; 6 reviews did not report the number of participants. For reviews where the population were service users, almost all were categorised as adults with mental health problems. Thirteen reviews specified that participants had severe mental illness (SMI) diagnoses [ 1 , 21 , 22 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ], six reviews explicitly included studies with participants accessing mental health services [ 22 , 37 , 38 , 43 , 45 ] [ 46 ], three reviews were conducted in perinatal populations [ 47 , 48 , 49 ], three reviews included participants with any/common mental health conditions [ 50 , 51 , 52 ], four reviews included participants with substance use disorders [ 1 , 38 , 53 , 54 ], two reviews included participants with eating disorders [ 55 , 56 ], one included people experiencing suicidality [ 57 ] and one included articles on peer support for crisis management [ 58 ]. The samples in the remaining reviews were PSWs and various stakeholders (e.g. non-peer staff, service users) [ 23 , 24 , 34 , 59 , 60 , 61 , 62 , 63 , 64 ]. Most reviews included interventions involving any form of peer support, individual, group or combined, although three reviews looked at group peer support alone [ 35 , 43 , 49 ], and three reviews looked at individual peer support alone [ 1 , 40 , 45 ]. Reviews looked at peer support delivered in-person, online or over the phone, and surveyed a range of approaches including both structured and unstructured peer support (see Table 1 ). The reviews included 426 primary studies. We assessed study overlap; most primary studies ( n = 300) were only included in one review; however, many primary studies were included twice ( n = 72), three times ( n = 18) to a maximum of nine times ( n = 1) (see Additional file 1 : Appendix 5 for overlapping studies). Only 1 review reported that people with lived experience were involved in the review [ 57 ]. Only 2 reviews assessed certainty of evidence (using GRADE) [ 21 , 22 ].
Most reviews were appraised as low or critically low (97%) quality and one review was appraised as high quality. The most common weaknesses were in critical domains concerning registering protocols before commencement of the review (21 studies), justification of excluding individual studies (28 studies) and considering risk of bias when interpreting results (13 studies). Reviews without meta-analyses were not scored in the critical domains assessing meta-analytical method or publication bias. There were 13 studies with meta-analyses assessed in these two domains: two of these exhibited one critical weakness and two exhibited two critical weaknesses. As scoping reviews are intended to provide overviews of existing literature regardless of risk of bias [ 65 ], scoping reviews were not scored in the critical domain concerning risk of bias assessment techniques (see Additional file 1 : Appendix 3 for adjustments to quality appraisal for scoping and qualitative reviews). Of the 29 reviews that were eligible to be scored in this domain, 10 exhibited a critical weakness. The review eliciting high confidence was a Cochrane review [ 21 ]. No reviews were rated as moderate. AMSTAR 2 ratings are detailed in Table 1 and in full in Additional file 1 : Appendix 3.
Results of synthesis
Rq1: what is the effectiveness (e.g. clinical, social, functional) and cost-effectiveness of paid peer support approaches for mental health.
Effectiveness outcomes were reported in 23 reviews (66% of total). A wide variety of clinical, recovery and psychosocial effectiveness outcomes were reported across both meta-analysis [ 21 , 22 , 37 , 40 , 41 , 42 , 43 , 44 , 45 , 47 , 48 , 51 , 52 ] and narrative results [ 1 , 21 , 22 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 48 , 50 , 51 , 53 , 54 , 56 , 57 , 58 , 60 ]. Comparator groups also varied across the primary studies included in the reviews, including Treatment as Usual (TaU), active controls (e.g. a comparable standard treatment) and waitlist control groups.
All outcomes except for one (family or carer use of formal community support services; [ 44 ]) were service user outcomes, rather than carer, staff or PSW outcomes. Outcomes from systematic reviews with meta-analysis are reported in Tables 2 , 3 and 4 . Effectiveness results from reviews not including meta-analysis are summarised at the end of this section and reported in full in Additional file 1 : Appendix 6. Evidence was heterogenous across all outcomes and reviews, with many analyses reporting no effect. In the meta-analysis results, there was often notable heterogeneity. There was limited data on cost and cost-effectiveness, but the evidence available from three systematic reviews without meta-analyses (See Additional file 1 : Appendix 6) suggested that peer support interventions were low cost and cost-saving [ 38 , 48 , 50 ].
Results from meta-analyses
Clinical outcomes.
For depression outcomes, evidence from two reviews with meta-analyses suggested that peer support is effective in improving perinatal depression [ 47 , 48 ]. Three reviews of peer support for adults and adolescents with mental health problems including those with SMI diagnoses reported no effect on depression post-intervention [ 22 , 35 , 43 ], where two of these reviews looked at group-based peer support alone [ 35 , 43 ]. Two of these reviews reported follow-up results; one review of group peer support for adults with any mental health condition continued to find no effect at 3–6 months follow-up [ 35 ], while the other involving adults with SMI reported improvements in depression and anxiety at 6 months follow-up, despite reporting no effect at post-intervention [ 22 ]. One review [ 52 ] measured clinical recovery in adults with any mental health diagnosis, reporting improvements post-intervention and at 6–9-month follow-up, but no improvement at 12–18-month follow-up.
Most evidence regarding mental health symptom severity among adults and adolescents with mental health diagnoses or who were using mental health services suggested no effect [ 22 , 35 , 41 , 42 , 43 , 44 ], other than for perinatal depression as previously summarised. One review [ 40 ] of individual peer support for adults with primarily SMI diagnoses reported improvements in symptom severity, while another involving adults with SMI [ 44 ] reported symptom improvements following family-led peer support, but no improvement following individual-led peer support. Results for service use varied depending on the measure, for example, peer support was associated with reduced risk of hospitalisation [ 44 ], including after a follow-up period [ 45 ], but no effect was found regarding length of stay [ 41 , 42 ].
All reviews providing meta-analytic evidence relevant to this question were rated low or critically low quality, except from one high-quality review [ 21 ] which found no effect of peer support on patient activation between 1 and 6 months follow-up (a person’s perceived ability to manage their illness and their approach to healthcare) in adults with schizophrenia diagnoses or similar SMI.
Recovery outcomes
Of the seven reviews with meta-analyses reporting data on overall self-reported recovery, five reported improvements in recovery in adults with mental health diagnoses including SMI [ 22 , 35 , 40 , 44 , 45 ]. Two studies found effects for individual peer support interventions alone [ 40 , 45 ], and one reported an effect for group-based peer support alone [ 35 ]. Only two reviews reported no effect [ 21 , 43 ], where one included studies of adults with SMI in both individual and group-based peer support [ 21 ], and the other involved studies with adults and adolescents with any mental health problem in group-based peer support alone [ 43 ].
Three reviews reported follow-up data showing continued improvements for adults with mental health diagnoses including SMI at follow-ups of 6 months [ 22 ], 3–6 months [ 35 ] and 12–18 months [ 45 ], the former and the latter reviewing individual and group peer support, and the second focussing on group peer support alone. One further review reported no improvements at medium-term follow-up (1–6 months) [ 21 ]. One review of adults with any mental health diagnosis identified improvements in personal recovery post-intervention, but not at 6–9 or 12–18 months follow-up, and found no improvements in functional recovery post-intervention or at 12–18 months follow-up, but did report improvements at 6–9 months follow-up [ 52 ].
All reviews providing meta-analytic evidence for these outcomes were rated as critically low or low quality, except for one [ 21 ] which was rated high quality. Based on evidence from three studies, this latter review [ 21 ] found no effect of peer support on recovery in the medium term for adults with schizophrenia diagnoses or similar SMI.
Psychosocial outcomes
Evidence regarding hope or hopefulness was mixed. Four reviews with meta-analyses suggested that peer support resulted in improvements in adults with SMI [ 22 , 37 , 40 , 44 ], where one of these studies looked at individual peer support alone [ 40 ] and the rest included both individual and group peer support. However, three reviews of studies including SMI and mixed mental health diagnoses samples reported no effect [ 21 , 35 , 43 ], where two of these reviews focussed on group-based peer support alone [ 35 , 43 ]. One study [ 22 ] followed up adults with SMI and those using secondary MH services at 3–6 months and found continued improvements in hope. However, another review investigating longer-term outcomes (over 6 months) in adults with SMI found no effect [ 21 ].
Improvements in empowerment were evidenced by two reviews with meta-analyses [ 40 , 51 ] of studies involving adults with any mental health diagnosis including SMI. No effects were reported in four reviews [ 22 , 35 , 43 , 44 ]. One of the meta-analyses finding positive effects of peer support on empowerment looked at individual peer support alone [ 40 ], whereas two of the meta-analyses with no effect solely involved group-based peer support [ 35 , 43 ]. Three studies reported follow-up data. Two showed improvements at 6 months in adults with SMI [ 22 ] and at 6–12 months follow-up among adults using mental health services with any diagnoses [ 45 ]. The other showed no improvements from group-based peer support only in adults with mental health diagnoses including SMI between 3 weeks and 6 months follow-up [ 35 ].
Quality of life reportedly improved in two reviews with meta-analyses [ 37 , 44 ] of studies involving adults with SMI, while there was no evidence of improvement in one other with an SMI sample [ 22 ]. The two studies which reported follow-up data continued to find no effect [ 22 , 45 ].
There were improvements in self-efficacy in adults with any mental health problem in all three reviews with meta-analyses reporting this outcome [ 43 , 44 , 51 ]. Decreases in self-stigma and stigma-related stress in adults and adolescents with any mental health problem were found by one review with meta-analysis of group-based peer support [ 43 ]. There was no evidence for peer support improving satisfaction with care [ 22 , 41 , 42 , 44 , 45 ] or relational outcomes (including social support and network) and building relationships (both personally and with staff) [ 41 , 42 , 44 , 45 ].
All reviews providing meta-analytic evidence for these outcomes were rated as critically low or low quality, except one high-quality review [ 21 ] which found no effect of peer support on hope in adults with schizophrenia diagnoses or similar SMI in the medium or long term.
Summary of results from systematic reviews without meta-analysis
Effectiveness results from systematic reviews without meta-analyses are tabulated in full in Additional file 1 : Appendix 6. These reviews presented mixed results pertaining to clinical outcomes including depression, anxiety, eating disorder pathology, and psychosis. However, two scoping reviews reported evidence of peer support in improving suicidal ideation [ 57 , 58 ]. Evidence was deemed inconclusive regarding the impact of peer support on indicators of service use, where three reviews failed to find evidence for peer support [ 21 , 22 , 41 , 42 ], three reported mixed results [ 1 , 38 , 54 ], and one found evidence for improvements associated with peer support [ 36 ]. More consistent evidence was found indicating peer support improves recovery outcomes [ 1 , 36 , 38 , 40 , 44 , 53 ]. For most psychosocial outcomes, systematic reviews presented mixed evidence, for example different effects were found by one high-quality review for empowerment, hope and self-efficacy, depending on what measures were used [ 21 ]. Despite mixed effects being reported overall for the impact of peer support on satisfaction with care, one review cited some possible associated moderating factors such as the number of conversations had between peer supporter and recipient [ 48 ]. Evidence was marginally less mixed for relational outcomes, such as strength of interpersonal relationships and sense of community, as the majority (three) of relevant reviews found evidence in support of peer support [ 21 , 38 , 58 ], although one review found this did not persist long term [ 21 ].
Implementation was investigated in nine reviews [ 23 , 24 , 36 , 39 , 46 , 50 , 55 , 59 , 62 ]. Table 5 shows an overview of implementation outcomes by CFIR domain [ 33 ]. All reviews relevant to this research question were rated as critically low quality based on the adapted AMSTAR 2 rating scale (see Additional file 1 : Appendix 3).
Studies reported generally high acceptability and feasibility of PSW-led interventions [ 36 , 39 , 46 , 50 ]. When planning a peer-led service, co-producing the design of peer support provision with the community and stakeholders was found to be key [ 59 ].
Outer setting
The existence of national policy and funding provisions for employing and retaining PSWs facilitated PSW-led care [ 39 , 46 , 59 ], as did integration of interventions within existing healthcare systems [ 50 ]. However, barriers included power hierarchies [ 39 ], difficulties incorporating PSWs in medical mental health care models [ 24 , 39 , 46 ], interference of work with welfare benefits [ 62 ] and a lack of recognised PSW certification [ 62 ].
Inner setting
A workplace culture emphasising recovery-orientated practice [ 24 , 59 ], and organisational openness and readiness to employ PSWs [ 39 ], was important. Facilitators included strong leadership and support at the highest level [ 46 ], and flexible and understanding employers, especially in times of crisis [ 59 ]. A key facilitator was a supportive, accepting and trusting workplace culture where PSWs occupy a central position and fit in well with other staff members [ 24 ]. A trusting culture allowed the management of risk in a psychologically safe space [ 59 ]; effective communication and collaboration between PSWs and other workers facilitated this [ 24 ], while stigmatising staff attitudes were a barrier [ 62 ]. It was easier to implement PSWs in a more collaborative and less hierarchical service [ 59 ]. There were practical facilitators and barriers for PSWs also, such as access to desk space or administrative data [ 24 , 46 ], time restraints, high caseloads [ 23 , 24 ] and insufficient funding for PSW role [ 24 , 50 ].
Individuals
The professionalisation and legitimisation of the PSW role was seen as important, with associated performance standards and/or a code of ethics [ 24 ] which was linked to rigorous recruitment practices, ensuring parity in the recruitment of PSWs and other staff [ 46 ]. A further facilitator was high levels of competency among peer-counsellors when delivering interventions and having relevant skills and knowledge, e.g. mental health conditions [ 50 ]. PSWs were often required to have recovered from their mental health difficulties [ 55 ] and be able to use their coping skills and resilience to avoid potential negative impacts on their wellbeing [ 24 ]. PSWs reported a conflicted sense of identity between being a ‘peer’ with experience of mental health problems and a ‘professional’ as a barrier to their work [ 62 ]. The use of champions and implementation leaders to drive the set up and maintenance of PSW interventions was reported as a facilitator [ 46 ], as was staff willingness and ability to work with PSWs and accept them as part of the service [ 24 ].
Implementation process
Studies emphasised the importance of comprehensive training for PSWs delivered both prior to starting work and on an ongoing basis, alongside regular clinical supervision [ 24 , 46 , 50 , 55 ] supporting the management of any problems encountered [ 59 ]. PSW roles should be clearly defined [ 24 , 62 ] and training should also be delivered to other members of staff to help them work effectively with PSWs [ 46 ]. Establishing sustainable models of cost and supervision from the outset was key for the longevity of PSW [ 50 ].
Experiences of both the benefits and challenges of peer support were reported in 11 reviews [ 23 , 34 , 39 , 42 , 46 , 49 , 55 , 60 , 61 , 63 , 64 ] from a range of perspectives: PSWs [ 23 , 34 , 39 , 55 , 61 ], service users [ 39 , 55 , 61 ], non-peer staff [ 61 ], peer support group members [ 49 ], and mixed samples which consisted of combinations of PSWs, service users, non-peer staff, carers, mental health organisations, policy makers and peer programme developers [ 23 , 39 , 42 , 46 , 55 , 60 , 61 , 63 , 64 ]. In one review, it was unclear whose perspective was being presented [ 46 ], although this review only contributed to one theme. All reviews providing evidence for this research question were rated as critically low quality based on the adapted AMSTAR 2 rating scale (see Additional file 1 : Appendix 3). We identified 3 overarching themes: (i) what the PSW role can bring, (ii) confusion over the PSW role and (iii) organisational challenges and impact. Table 6 gives an overview of the overarching themes and subthemes (with more detail in Additional file 1 : Appendix 7). The following provides an overview of each overarching theme from the perspective of the different samples (i.e. PSWs, service users, mixed samples).
What the PSW role can bring
Perspective of psws.
PSWs experienced improved wellness and recovery from working in the role, reporting increased self-esteem, personal growth, and social networks [ 23 , 34 , 55 , 61 ]. They benefited in a variety of ways, e.g. the role provided a route back into employment, improving functioning and social inclusion, and allowed them to learn more about their own mental health [ 23 , 34 ]. PSWs also reported increased self-acceptance as they no longer had to hide their mental health issues [ 34 ]. The role was therefore often reported to be mutually beneficial for PSWs and service users [ 34 , 55 ]. PSWs felt it was important that they were role models for service users, being ‘the evidence of recovery’ [ 34 ]. However, working as a PSW could also have a negative impact on the PSWs’ wellbeing and recovery [ 23 , 34 ]. Reasons for this included the role reminding them of their mental health condition and the ‘sick’ label staying with them [ 23 ].
Perspective of service users
For service users, PSWs could be role models, giving them hope of recovery [ 39 , 55 , 61 ]. PSW support normalised and de-medicalised service user experiences [ 55 ]. Lack of judgement from PSWs reduced feelings of self-stigma for service users [ 55 ]. Service users felt empowered by and valued gaining experiential knowledge from PSWs, perceiving them to be more insightful than non-peer staff, and trusting their services [ 39 ]. Service users also built rapport more easily with PSWs than non-peer staff, feeling they were more approachable and had greater empathy than non-peer staff [ 39 , 61 ]. However, some service users reported that PSWs are not role models and found it challenging to view them as professionals or fully trust their knowledge, due to their lack of training and concerns about their mental health history [ 39 , 61 ].
Perspective of non-peer staff
From working with PSWs, non-peer staff developed increased empathy towards service users and a belief in recovery [ 61 ].
Perspective of peer support group members
Forming relationships in peer support groups and having their experiences validated by others was valuable for recovery [ 49 ]. However, group members could feel isolated when other members’ experiences contrasted with their own [ 49 ].
Perspective of mixed samples
PSWs were perceived to be role models, providing valuable support to service users and giving them hope of recovery [ 60 , 64 ]. Working as a PSW could enable service users to find a role in the community, beyond the identity of being a ‘patient’ [ 61 ]. PSWs could build trust-based pathways to function as a bridge between service users and non-peer staff [ 64 ]. Within teams, working with PSWs could improve recovery-oriented care and PSWs carried out various roles, such as providing psychosocial support, advocating for service users, providing insights based on their lived experiences [ 64 ]. For mental health organisations, PSW roles decreased stigma towards mental health problems and set a positive example [ 61 ]. However, there were fears that the PSWs’ mental health condition could impact the provided support, such as increased PSW absenteeism which could increase non-peer staff caseloads and concerns that service users’ and PSWs’ could experience distress due to exposure to difficult (‘triggering’) content [ 42 , 55 , 60 ]. PSWs experienced pressure due to the perception that they were pioneers, leading to expectations, e.g. failure could reduce future PSW opportunities [ 64 ]. There was also concern that PSWs lacked mental health knowledge, beyond their own experience [ 64 ].
Confusion over the PSW role
A lack of clarity about the PSW job description led PSWs to feel the role was undervalued and tokenistic and meant they felt confused in their role. This impacted their perception of competence which affected their recovery and led to uncertainty in their responsibilities with service users [ 23 , 34 ]. PSWs also found the transition from service user to PSW and knowing where to draw the line between friend and service provider to be challenging [ 23 , 61 ]. Linked to this, their dual identity as a service user and provider could be a source of stress. For example, it meant they could closely connect with service users who had similar difficulties to their own, but this could also be triggering and lead to a recurrence of the PSWs’ own mental health issues [ 34 ]. PSWs expressed varying views on disclosing their recovery story [ 34 , 39 ]. For some, sharing elements of their story was linked to their own personal recovery [ 34 ]. However, other PSWs felt fearful of disclosure, e.g. they were concerned about being labelled ‘mentally ill’ and service users not trusting them [ 39 ].
A lack of clarity on the PSW role could lead service users to view the role as informal, leading to negative perceptions of the PSW services. Perceptions of tokenism of peer support could lead to the content of the PSW intervention ‘feeling irrelevant’ [ 39 ].
PSWs and non-peer staff found the PSW role to be ambiguous, e.g. the role was not clearly defined [ 63 ] and job descriptions were ‘vague’ [ 64 ]. Although this gave flexibility to define the role [ 64 ], it also led to challenges. Some PSWs felt they were expected to develop the role over time and received insufficient training, which hampered service delivery and could result in perceptions that PSWs were tokenistic [ 42 , 63 , 64 ]. Uncertainty about the role also led to a lack of support from non-peer staff [ 63 ]. Relatedly, there was confusion for PSWs over when/with whom to disclose their lived experience [ 63 , 64 ]. Some PSWs felt vulnerable and were reluctant to disclose, but disclosure could build trust with service users, enabled PSWs to be recovery role models, and could educate non-peer staff on alternative views [ 63 , 64 ]. Disclosure was also felt to require discretion when fitting with professional relationships. However, ‘professionalisation’ of PSWs may not challenge the existing boundaries (e.g. traditional hospital-based boundaries which could make it difficult for the sharing of lived experience to be valuable), when challenging these boundaries could change culture [ 63 , 64 ]. The transition for PSWs from patient to staff was challenging, e.g. non-peer staff were concerned about the PSW becoming unwell, making PSWs feel like they are being treated like patients [ 63 , 64 ]. There were issues around boundaries, including whether PSWs should relate to service users as friends or service users [ 63 ].
Organisational challenges and impact
PSWs experienced a lack of support and training for their role, potentially related to unclear job descriptions, and insufficient supervision [ 23 , 34 ]. This meant that PSWs struggled to develop the skills for their roles, including to work with service users with more complex needs than their own experiences [ 23 ]. Although there were some contrasting views, PSWs were concerned that they received low pay which made them feel that they were not valued, and they perceived themselves to be ‘cheap labour’ [ 23 , 34 , 61 ]. Some PSWs felt accepted in their teams however others experienced negative and rejecting non-peer staff attitudes [ 23 , 34 , 61 ]. For example, PSWs reported not being invited to social events and being treated like patients [ 61 ]. Consequently, some PSWs felt excluded, that their roles were tokenistic and experienced self-stigma [ 23 , 34 ]. PSWs as part of the newer recovery model reported challenges around integrating into traditional treatment models, e.g. where doctors spent the least time with service users but held the majority of power and decision making for service users. PSWs were expected to contest the traditional treatment model in support of a recovery focus, e.g. by their presence or in some cases being openly challenging, and this clash between old and new treatment models could lead to friction [ 23 ].
There was a fear that ‘cheap labour’ provided by PSWs may lead to fewer non-peer staff positions [ 61 ].
PSWs often received low pay, which led to role dissatisfaction for PSWs, suggesting the job was tokenistic or the role was unclear [ 63 , 64 ]. One reason for low pay was due to PSWs not requiring certification (i.e. specific qualifications, which e.g. a social worker would require) [ 63 ]. Some PSWs were positive about certification but others felt it could conflict with the grassroots ethos of peer support. However, there was the view that lived experience was not solely sufficient to work in interprofessional teams [ 64 ]. Despite this, supervision and support were often not offered to PSWs leading to risks [ 60 , 64 ].
There were challenges in PSW relationships with non-peer staff which could lead to a lack of support and hostility from non-peer staff. Non-peer staff felt threatened that they may be replaced by PSWs [ 64 ], were uneasy about working with people they previously treated [ 46 ], were concerned about the effectiveness of peer support [ 39 ], and felt expectations to support PSWs, increasing their workload [ 42 ]. This undermined the role of PSWs, e.g. they were subsequently given fewer responsibilities [ 39 ]. For PSWs, they wanted to challenge stigma by taking on more responsibility but high, varying workloads could jeopardise relationships with non-peer staff and team hierarchies hindered their ability to challenge clinically dominant ways of thinking [ 64 ].
A final theme was the perception that service users should be able to choose among PSWs as service providers [ 60 ].
Summary of key findings
An overview and summary of the key findings for each research question is presented in Table 7 .
Key findings
Our umbrella review of 35 reviews explored the effectiveness, implementation and experiences of peer support for mental health.
Effectiveness was reported in 23 reviews. Many reviews reporting effectiveness data reported no effect of peer support on a range of outcomes, mirroring the findings from other reviews [ 9 , 66 ] including those focusing on other types of peer support (e.g. online peer support for young people) [ 67 ]. However, there was consistent evidence from meta-analyses that peer support may improve the clinical outcomes of perinatal depression and risk of hospitalisation of adults with severe mental illness, as well as recovery outcomes, and self-efficacy and stigma-related outcomes. Mixed meta-analytic results were found for the clinical outcomes of overall psychiatric symptoms in adults with SMI, psychosis symptoms, length of hospital stay and patient activation, and for psychosocial outcomes such as hope, empowerment, and quality of life. There was no meta-analytic evidence for improvements in relational support. Evidence from systematic reviews without meta-analysis similarly gave a mixed picture regarding psychosocial and clinical outcomes, but indicated more consistent evidence that peer support has a positive impact on recovery, suicidal ideation, and, to some degree, satisfaction with care.
Many possible sources of heterogeneity across the included reviews could contribute to the mixed findings in this study, such as low-quality methodologies, differences in the populations included, and poor specification of peer support roles or the content of interventions delivered. One important potential contributor to our mixed results is that the primary studies contributing to the included reviews often varied in the type of control groups they considered, for example studies with treatment as usual, active controls and waitlist controls were often reviewed within the same paper. As such, it was not possible to determine whether peer support is effective in comparison to certain types of care provision but not others. In a similar vein, we could not perform subgroup analysis to determine whether specific forms of peer support are more effective on certain populations as most reviews with meta-analyses involved a combination of different formats and a range of participant groups. Nevertheless, there was some indication that differences in the format of peer support may impact its effectiveness on empowerment, as the two meta-analyses involving individual peer support alone found a positive effect on empowerment, but the two looking at group-based peer support alone did not. However, further research is needed to adequately address such questions.
Although this overview of quantitative evidence does not give unequivocal support for peer support on a variety of outcomes, the mixed results must be understood not only in the context of heterogeneity of the quantitative research conducted thus far, but with regard to the qualitative evidence documenting strong support for this intervention (as discussed in more detail below). Given that the implementation of peer support in mental health services is still relatively rare and highly variable, many of the trials conducted thus far may have tested peer support in environments where it is not fully embedded in the organisation and culture. Indeed, peer support may have positive impacts on the operation of mental health services that have not been measured as quantitative outcomes in existing trials—such as a stronger culture of person-centred care. More consistent quantitative results demonstrating the benefit of peer support may increasingly emerge as it becomes better integrated in the mental health care system.
We identified several factors reported to be important for the successful implementation of peer support, which were summarised and structured using the CFIR. These factors included adequate training and supervision for PSWs, a recovery-oriented workplace structure, strong leadership and a supportive and trusting workplace culture with effective collaboration between PSWs and non-peer staff. Barriers to peer support being implemented effectively included a lack of time, resources, and appropriate funding, and a lack of recognised PSW certification. Policy, research and campaign groups have advocated implementation approaches in line with these findings, for example, ImROC (implementing Recovery through Organisational Change) [ 14 , 68 ], who support peer support implementation globally and international competence frameworks from New Zealand [ 69 , 70 ], outline recovery focus as a core principle of peer support and emphasise the importance of training and ongoing professional development; peer support practice guidelines in the USA outline the importance of and give guidelines for supervision [ 71 ]. Formalised career pathways for PSWs [ 72 ] may help to address some of the identified barriers to effective implementation of peer support work, although these are still early in their development [ 68 ].
Experiences of peer support were from a range of perspectives (e.g. PSWs, service users, non-peer staff) and were organised under three main themes. The benefits of peer support for PSWs, service users and non-peer staff were expressed in many reviews; however, there were also conflicting and challenging experiences of the role. The mental health experience of PSWs was viewed as valuable, but also subject to some stigmatising views. For PSWs, the role could improve their personal wellness and recovery, providing a route back into employment and improving functioning, and provide service users with role models of recovery. The reciprocal benefits of peer support have also been highlighted as an advantage of peer support in resources developed by NHS England [ 19 ]. However, PSWs reported the ‘sick’ label stayed with them in the role, with non-peer staff at times concerned that PSWs mental health would impact their work, and some service users reported that they found it challenging to trust PSWs knowledge due to their lack of training and mental health history. A key experience, which became the core of our second theme, was the ambiguity of the PSW job description, including lack of clarity over boundaries with service users and when to disclose PSWs’ personal experiences. This ambiguity meant that the role was flexible, but also led to the perception that it was tokenistic and left PSWs feeling confused which impacted their own recovery. IMROC recommend the prioritisation of clear roles when implementing peer support [ 68 ]. Professional accreditation can counter the view of peer support as tokenistic, e.g. the UK Peer Support Competence Framework outlined by the Royal College of Psychiatrists [ 73 ] and the Canadian Peer support Accreditation and Certification, a national standard endorsing peer support work as a valuable career, developed in 2017 by PSWs themselves [ 74 ]. The final theme ‘organisational challenges and impact’ included experiences such as PSWs receiving inadequate support, training and supervision, and receiving low pay, leaving them feeling undervalued. Some non-peer staff attitudes were also a reported issue; while some PSWs felt accepted within teams, others experienced negative and rejecting non-peer staff attitudes, such as being treated as patients and not being invited to staff social events. Organisations should prepare, structurally and culturally, for the introduction of PSWs in order to ensure PSW wellbeing and reduce the risk of absences due to sickness [ 68 , 75 ].
Strengths and limitations
We conducted a comprehensive search of several relevant databases and identified a large number of reviews for inclusion, providing the first detailed summary of review findings relating to effectiveness, implementation and experiences of peer support. We also had consistent involvement of researchers with lived experience of mental health and peer support delivery and receipt throughout the design, data screening and extraction, analysis and synthesis, and manuscript drafting for this paper, which allowed lived experience priorities and experiences to guide our approaches to data and our decision making throughout.
We aimed to focus our review on paid peer support; however, this information was underreported in the reviews, and even when reported, interventions were often grouped with peer support interventions that did not fully meet our eligibility criteria (e.g. were unpaid). We also synthesised data from studies where payment status of PSWs was ambiguous, i.e. not reported. This limits our ability to draw firm conclusions around paid peer support specifically, as a significant portion of the data synthesised was from studies investigating unpaid or voluntary peer support. Another limitation was the lack of involvement of people with lived experience in the included reviews, with involvement reported in only one review [ 57 ]. Given the service user-led origins of peer support, future reviews should ensure involvement of people with lived experience. This is addressed in more detail later in this paper. Most included reviews were appraised by the AMSTAR 2 as low or critically low (97%) quality with only one review appraised as high quality. Although the low quality of reviews is a limitation, we aimed to report an overview of all current evidence for peer support to inform policy makers and healthcare practitioners, therefore to maximise the evidence base, we synthesised the reviews scored as ‘critically low quality’. Our ratings are also in line with a prior umbrella review of peer support which rated 87% of reviews as critically low quality and the remainder as low quality, but reported outcomes from all reviews [ 66 ].
Beyond the aforementioned limitations regarding variation in studies within each review, there is also a loss of granular detail through the umbrella review process of summarising data across reviews, which themselves contain many studies which have been summarised. The person-centred nature of peer support may mean that there are meaningful outcomes for the service user which are not easily captured in standard outcome measurement tools or recognised as clinically significant. Variation in peer support roles across studies may have contributed to the contradictions in our findings for RQ3, e.g. the challenges around PSW roles being ambiguous, but also the reported benefits of a flexible role.
A strength of our review was our broad inclusion criteria, for example, for qualitative data on experiences of peer support we reported data from the perspectives of service users, non-peer staff and PSWs. Though some data was reported separately by role, there were studies where experiences were reported together, and these perspectives were difficult to disentangle. Finally, we did not conduct a formal meta-synthesis of the qualitative experiences data; therefore, some detail may have been missed.
Implications for practice
Peer support may be effective at improving some clinical outcomes, self-efficacy and recovery outcomes for some people and could augment the standard service range. Certain groups may benefit from peer support more than others; evidence was strongest for depression outcomes within perinatal populations, but extremely variable for other populations. Peer support may differ in effectiveness depending on population needs and characteristics. PSWs need adequate pay, clear role descriptions and guidelines (e.g. about boundaries and disclosure), ongoing training and supervision, and opportunities for progression. Attitudes about peer support held by non-peer staff may significantly support or impede the implementation and experience of PSWs, and non-peer staff may require training about PSW roles and how to work collaboratively with PSWs. Culture, hierarchical structure and staff acceptability of peer support impact implementation and experience of peer support—structural and cultural change may be required for peer support to succeed, e.g. ensuring a recovery-oriented care model is operating in the service.
Implications for policy
Successful implementation of PSWs in healthcare settings is likely to require a coproduction approach with clearly defined PSW roles, a receptive hierarchical structure and staff, strong leadership and appropriate training (for PSWs and staff) with clinical and/or peer supervision alongside safeguarding. Issues relating to cost, lack of time and lack of resources are key considerations for service providers aiming to implement PSW that is sustained and effective within services. Additionally, Services could benefit from clear, coproduced guidelines, outlining the steps that are most likely to lead to successful PSW implementation.
Implications for research
Future primary and secondary research could usefully explore the differences in efficacy, implementation and experiences in paid PSW over time as it becomes more established; an important distinction as there are likely to be differences in these outcomes as the role of PSW develops. Such studies could consider using more personalised outcome measures such as goal-based outcome measurement [ 76 ]. Current PSW roles are still poorly defined and PSW content, including PSW variations (such as whether PSWs should deliver structured or more loosely structured, informal interventions, or whether interventions should vary according to need and context), need further exploration. Realist investigations around what works for whom, how and in which contexts would uncover more fine-grained detail on the specific contexts and mechanisms that explain these differences. Very few reviews included in this umbrella review reported lived experience researcher leadership or involvement in the undertaking of the study. It is imperative for future research in this area to appropriately reflect the priorities of those who are directly involved in PSW, either as providers or as service users. As the number of PSWs increases and more formalised roles are created, positive impact may not be restricted to outcomes of those supported by PSWs, but also to the functioning of services at an organisational level [ 68 ]. Further research is needed to evaluate how teams function with and without PSWs in order to understand how they may impact experiences through changes at a system level [ 68 ].
Our umbrella review has summarised data from 35 reviews on the effectiveness, implementation, and experiences of peer support for mental health. Although we attempted to focus solely on paid peer support, this detail was often not reported in the reviews. While data on effectiveness was mixed, there was some evidence of improvements on outcomes including depression, particularly perinatal depression, self-efficacy, and recovery, illustrating the potential benefits of wider PSW implementation across mental health services. Good implementation of peer support depends on co-design with people with lived experience, clear job descriptions, a recovery-oriented workplace culture, strong leadership, appropriate training for PSWs and staff , and supervision for PSWs. However due to limited information on cost or cost-effectiveness, we are unable to draw conclusions around resources required to implement PSWs. Experiences of peer support were from a range of perspectives. Peer support was mutually beneficial for PSWs’ and service users’ wellbeing and recovery and PSWs became role models. However, at times PSW roles were ambiguous, this meant that the role was flexible but could also lead to confusion which could impact PSWs own recovery. Potential strategies to successfully implement peer support include that the PSW roles should be clear, PSWs should be appropriately trained and paid, as well as supported and supervised within a trusting and accepting workplace structure and culture that advocates for a recovery-oriented model of care.
Lived experience commentary, written by LM and KM
This study provides a useful summary of the available research on peer support. By providing an overarching review of 35 reviews including 426 available studies, the paper brings together the knowledge on a topic of growing importance and understanding of the experiences, effectiveness, and implementation of peer support. However, this evidence is limited to ‘paid peer support workers’ included in data from academic literature of systematic reviews.
The nature of an umbrella review means that the systematic reviews themselves are synthesised, limiting our ability to look at specific details in the primary studies, for example to look for evidence of lived experience involvement or co-authorship or demographics of participants. The papers within the review are likely to have originated from traditionally funded research enquiries, and an umbrella review potentially magnifies academic or clinical perspectives over user voices and interests. While this is a frustration in any mental-health-related topic, this is particularly concerning in relation to peer support, with its origins in our user-led history.
The roots in user-led peer support are also overlooked when limiting the studies to paid peer support work. Although they might use the same language of mutuality and reciprocity, the two feel different. We are hesitant to suggest that we would prefer the skills and expertise of our supporters to be voluntary and unpaid; we strongly believe their expertise should be valued and funded. But there is something magical about informal peer support which can be lost when it is over-policed in bureaucratic cultures. Additionally, with studies included in the review dating back to 1979, we question how relevant these studies are in informing England’s evolving peer support landscape.
A crucial area of future research is exploring what type of peer support works best for whom and in what circumstances, and how we can deliver this. Furthermore, we need to better understand how NHS cultures can be supported to value the expertise that originates in our lived experience, including the marginalised experiences which have been disproportionately represented in mental health services.
Availability of data and materials
The data used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
A MeaSurement Tool to Assess systematic Reviews
Consolidated Framework for Implementation Research
Implementing Recovery through Organisational Change
Lived Experience Working Group
Population, Intervention, Comparator group, Outcome
Peer support worker
Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, et al. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Serv. 2014;65:429–41.
Article PubMed Google Scholar
NHS Health Education England: Peer support workers. https://www.hee.nhs.uk/our-work/mental-health/new-roles-mental-health/peer-support-workers . Accessed 4 Aug 2023.
Gillard S. Peer support in mental health services: where is the research taking us, and do we want to go there? J Ment Heal. 2019;28:341–4.
Article Google Scholar
Watson E. The mechanisms underpinning peer support: a literature review. J Ment Heal. 2019;28:677–88.
Salzer MS, Shear SL. Identifying consumer-provider benefits in evaluations of consumer-delivered services. Psychiatr Rehabil J. 2002;25:281–8.
Galloway A, Pistrang N. “We’re stronger if we work together”: experiences of naturally occurring peer support in an inpatient setting. J Ment Heal. 2019;28:419–26.
O’Connell MJ, Flanagan EH, Delphin-Rittmon ME, Davidson L. Enhancing outcomes for persons with co-occurring disorders through skills training and peer recovery support. J Ment Heal. 2020;29:6–11.
Lawn S, Smith A, Hunter K. Mental health peer support for hospital avoidance and early discharge: an Australian example of consumer driven and operated service. J Ment Heal. 2008;17:498–508.
Bellamy C, Schmutte T, Davidson L. An update on the growing evidence base for peer support. Ment Heal Soc Incl. 2017;21:161–7.
Mental Health Mates. https://www.mentalhealthmates.co.uk/our-story/ . Accessed 4 Aug 2023.
Peer Support. https://www.england.nhs.uk/personalisedcare/supported-self-management/peer-support/ . Accessed 4 Aug 2023.
National Voices. Peer support. What is it and does it work ? 2015. p. 58.
Watson E, Meddings S. Peer support in mental health. London: Bloomsbury Publishing; 2019.
Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Briefing: Peer support workers: theory and practice. CentreformentalhealthOrgUk. 2013. p. 1–16.
Faulkner A, Basset T. A helping hand: taking peer support into the 21st century. Ment Heal Soc Incl. 2012;16:41–7.
NICE. NHS Long Term Plan » NHS Mental Health Implementation Plan 2019/20 – 2023/24. 2019.
Department of Health. The fifth national mental health and suicide prevention plan. 2017.
Farmer P, Dyer J. The five year forward view for mental health. 2016.
Integrated personal commisioning. Community capacity and peer support: summary guide. NHS Engl. 2017:66. https://pdf4pro.com/view/community-capacity-and-peer-support-nhs-england-78a0d2.html . Accesed 5 June 2023.
Mental Health Commission of Canada: Peer Support. https://mentalhealthcommission.ca/what-we-do/access/peer-support/ . Accessed 4 Aug 2023.
Chien WT, Clifton AV, Zhao S, Lui S. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database Syst Rev. 2019;2019:CD010880.
PubMed Central Google Scholar
Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. 2014;14:1–12.
du Plessis C, Whitaker L, Hurley J. Peer support workers in substance abuse treatment services: a systematic review of the literature. J Subst Use. 2020;25:225–30.
Ibrahim N, Thompson D, Nixdorf R, Kalha J, Mpango R, Moran G, et al. A systematic review of influences on implementation of peer support work for adults with mental health problems. Soc Psychiatry Psychiatr Epidemiol. 2020;55:285–93.
Belbasis L, Bellou V, Ioannidis JPA. Conducting umbrella reviews. BMJ Med. 2022;1:e000071.
Article PubMed PubMed Central Google Scholar
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132–40.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ WV (editors), editor. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Google Scholar
Cooper R, Saunders K. The effectiveness, implementation, and experiences of peer support approaches for mental health: an umbrella review of reviews. PROSPERO 2022 CRD42022362099. 2022. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022362099 .
Aromataris E, Fernandez R, Godfrey C, Holly C, Khalil H, Tungpunkom P. Chapter 10: Umbrella Reviews. In: Aromataris E, Munn Z (editors). JBI manual for evidence synthesis. JBI. 2020. https://doi.org/10.46658/JBIMES-20-11 . Available from: https://synthesismanual.jbi.global .
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:1–9.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:1–15.
Bailie HA, Tickle A. Effects of employment as a peer support worker on personal recovery: a review of qualitative evidence. Ment Heal Rev J. 2015;20:48–64.
Lyons N, Cooper C, Lloyd-Evans B. A systematic review and meta-analysis of group peer support interventions for people experiencing mental health conditions. BMC Psychiatry. 2021;21:1–17.
Fortuna KL, Naslund JA, LaCroix JM, Bianco CL, Brooks JM, Zisman-Ilani Y, et al. Digital peer support mental health interventions for people with a lived experience of a serious mental illness: systematic review. JMIR Ment Heal. 2020;7:e16460.
Fuhr DC, Salisbury TT, De Silva MJ, Atif N, van Ginneken N, Rahman A, et al. Effectiveness of peer-delivered interventions for severe mental illness and depression on clinical and psychosocial outcomes: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1691–702.
Gaiser MG, Buche JL, Wayment CC, Schoebel V, Smith JE, Chapman SA, et al. A systematic review of the roles and contributions of peer providers in the behavioral health workforce. Am J Prev Med. 2021;61:e203–10.
Ong QS, Yang HZ, Kuek JHL, Goh YS. Implementation of peer-support services in Asia: a scoping review. J Psychiatr Ment Health Nurs. 2022;30:309–25.
Peck CKH, Thangavelu DP, Li Z, Goh YS. Effects of peer-delivered self-management, recovery education interventions for individuals with severe and enduring mental health challenges: a meta-analysis. J Psychiatr Ment Health Nurs. 2023;30:54–73.
Pitt VJ, Lowe D, Prictor M, Hetrick S, Ryan R, Berends L, et al. A systematic review of consumer-providers’ effects on client outcomes in statutory mental health services: the evidence and the path beyond. J Soc Social Work Res. 2013;4:333–56.
Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. 2013;2013:CD004807.
PubMed PubMed Central Google Scholar
Sun J, Yin X, Li C, Liu W, Sun H. Stigma and peer-led interventions: a systematic review and meta-analysis. Front Psychiatry. 2022;13:1–12.
Wang Y, Chen Y, Deng H. Effectiveness of family-and individual-led peer support for people with serious mental illness a meta-analysis. J Psychosoc Nurs Ment Health Serv. 2022;60:20–6.
White S, Foster R, Marks J, Morshead R, Goldsmith L, Barlow S, et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry. 2020;20:1–20.
Mutschler C, Bellamy C, Davidson L, Lichtenstein S, Kidd S. Implementation of peer support in mental health services: a systematic review of the literature. Psychol Serv. 2022;19:360–74.
Fang Q, Lin L, Chen Q, Yuan Y, Wang S, Zhang Y, et al. Effect of peer support intervention on perinatal depression: a meta-analysis. Gen Hosp Psychiatry. 2022;74:78–87.
Huang R, Yan C, Tian Y, Lei B, Yang D, Liu D, et al. Effectiveness of peer support intervention on perinatal depression: a systematic review and meta-analysis. J Affect Disord. 2020;276:788–96.
Jones CCG, Jomeen J, Hayter M. The impact of peer support in the context of perinatal mental illness: a meta-ethnography. Midwifery. 2014;30:491–8.
Triece P, Massazza A, Fuhr DC. Effectiveness and implementation outcomes for peer-delivered mental health interventions in low- and middle-income countries: a mixed-methods systematic review. Soc Psychiatry Psychiatr Epidemiol. 2022;57:1731–47.
Burke E, Pyle M, Machin K, Varese F, Morrison AP. The effects of peer support on empowerment, self-efficacy, and internalized stigma: a narrative synthesis and meta-analysis. Stigma Heal. 2019;4:337–56.
Smit D, Miguel C, Vrijsen JN, Groeneweg B, Spijker J, Cuijpers P. The effectiveness of peer support for individuals with mental illness: systematic review and meta-analysis. Psychol Med. 2022;53:5332–41.
Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer-delivered recovery support services for addictions in the united states: a systematic review. J Subst Abuse Treat. 2016;63:1–9.
Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, et al. Peer recovery support for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. 2014;65:853–61.
Lewis HK, Foye U. From prevention to peer support: a systematic review exploring the involvement of lived-experience in eating disorder interventions. Ment Heal Rev J. 2022;27:1–17.
Pellizzer ML, Wade TD. The effectiveness of lived experience involvement in eating disorder treatment: a systematic review. Int J Eat Disord. 2022;56:331–49.
Schlichthorst M, Ozols I, Reifels L, Morgan A. Lived experience peer support programs for suicide prevention: a systematic scoping review. Int J Ment Health Syst. 2020;14:1–13.
Bowersox NW, Jagusch J, Garlick J, Chen JI, Pfeiffer PN. Peer-based interventions targeting suicide prevention: a scoping review. Am J Community Psychol. 2021;68:232–48.
Zeng G, McNamara B. Strategies used to support peer provision in mental health: a scoping review. Adm Policy Ment Heal Ment Heal Serv Res. 2021;48:1034–45.
Åkerblom KB, Ness O. Peer Workers in co-production and co-creation in mental health and substance use services: a scoping review. Adm Policy Ment Heal Ment Heal Serv Res. 2023;50:296–316.
Walker G, Bryant W. Peer support in adult mental health services: a metasynthesis of qualitative findings. Psychiatr Rehabil J. 2013;36:28–34.
Vandewalle J, Debyser B, Beeckman D, Vandecasteele T, Van Hecke A, Verhaeghe S. Peer workers’ perceptions and experiences of barriers to implementation of peer worker roles in mental health services: a literature review. Int J Nurs Stud. 2016;60:234–50.
Miyamoto Y, Sono T. Lessons from peer support among individuals with mental health difficulties: a review of the literature. Clin Pract Epidemiol Ment Heal. 2012;8:22–9.
Viking T, Wenzer J, Hylin U, Nilsson L. Peer support workers’ role and expertise and interprofessional learning in mental health care: a scoping review. J Interprof Care. 2022;36:828–38.
Article CAS PubMed Google Scholar
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Yim CST, Chieng JHL, Tang XR, Tan JX, Kwok VKF, Tan SM. Umbrella review on peer support in mental disorders. Int J Ment Health. 2023;52:379–400.
Ali K, Farrer L, Gulliver A, Griffiths KM. Online peer-to-peer support for young people with mental health problems: a systematic review. JMIR Ment Heal. 2015;2:1–9.
Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Peer support workers: a practical guide to implementation. 2013:1–32.
Te Pou. Competencies for the mental health and addiction service user, consumer and peer workforce. 2014:1–26. https://www.hqsc.govt.nz/assets/Our-work/Mental-health-and-addiction/Resources/DG038-Te-Poucompetencies-for-mental-health.pdf . Accessed 4 Aug 2023.
Te Pou. Competencies for the mental health and addiction consumer, peer support and lived experience workforce. 2021:1–26.
Foglesong D, Knowles K, Cronise R, Wolf J, Edwards JP. National practice guidelines for peer support specialists and supervisors. Psychiatr Serv. 2022;73:215–8.
Ball M, Skinner S. Raising the glass ceiling : considering a career pathway for peer support workers - 2021. 2021.
National Health Service [NHS]. The competence framework for mental health peer support workers. 2020.
Peer C, Mentors S. Peer Support Accreditation and Certification (Canada). National Certification Handbook. 2014.
Poremski D, Kuek JHL, Yuan Q, Li Z, Yow KL, Eu PW, et al. The impact of peer support work on the mental health of peer support specialists. Int J Ment Health Syst. 2022;16:1–8.
Law D. The Goal-based Outcome (GBO) tool guidance notes. 2019.
Download references
Acknowledgements
This work is supported by the NIHR UCLH BRC.
This study is funded by the National Institute for Health and Care Research (NIHR) Policy Research Programme. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Ruth E. Cooper and Katherine R. K. Saunders are joint first-authors.
Authors and Affiliations
NIHR Mental Health Policy Research Unit, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Ruth E. Cooper, Katherine R. K. Saunders, Jessica Griffiths, Ruth Stuart & Alan Simpson
NIHR Mental Health Policy Research Unit, Division of Psychiatry, University College London, London, UK
Anna Greenburgh, Rebecca Appleton, Phoebe Barnett, Sophie M. Allan, Brynmor Lloyd-Evans & Sonia Johnson
Centre for Outcomes Research and Effectiveness, Research Department of Clinical, Educational and Health Psychology, University College London, London, UK
Phoebe Barnett
National Collaborating Centre for Mental Health, Royal College of Psychiatrists, London, UK
University of East Anglia, Norwich, UK
Sophie M. Allan
MHPRU Lived Experience Working Group, London, UK
Prisha Shah, Karen Machin, Tamar Jeynes, Lizzie Mitchell, Beverley Chipp & Stephen Jeffreys
Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, London, UK
Alan Simpson
Camden and Islington NHS Foundation Trust, London, UK
Sonia Johnson
You can also search for this author in PubMed Google Scholar
Contributions
All authors (RC, KS, AG, PS, RA, KM, TJ, PB, SA, JG, RS, LM, BC, SJ, BLE, AS, SJ) substantially contributed to the conception or design of this study. Data acquisition was undertaken by: KS, RC, JG, RS, RA, KM, PS, SA, PB. The data were synthesised and interpreted by: KS, AG, RA, PS, KM, TJ, and RC. KS and RC led on drafting the manuscript with input and/or editing by all other authors (AG, PS, RA, KM, TJ, PB, SA, JG, RS, LM, BC, SJ, BLE, AS, SJ). All authors (RC, KS, AG, PS, RA, KM, TJ, PB, SA, JG, RS, LM, BC, SJ, BLE, AS, SJ) read and approved the final manuscript.
Authors’ Twitter handles
Twitter handles: @soniajohnson (Sonia Johnson); @cityalan (Alan Simpson); @MentalHealthPRU (Mental Health Policy Research Unit).
Corresponding authors
Correspondence to Ruth E. Cooper or Katherine R. K. Saunders .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
KM is a Director of With-you Consultancy Ltd who provide peer support training and consultancy. All other authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Prisma checklist [ 29 ]. Appendix 2. Full search strategy. Appendix 3. AMSTAR2 ratings. Appendix 4. Excluded studies following full text screening, with reasons. Appendix 5. Study overlap. Appendix 6. Effectiveness of peer support outcomes: results for non-meta-analysis results. Appendix 7. Experiences of peer support (detailed themes).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Cooper, R.E., Saunders, K.R.K., Greenburgh, A. et al. The effectiveness, implementation, and experiences of peer support approaches for mental health: a systematic umbrella review. BMC Med 22 , 72 (2024). https://doi.org/10.1186/s12916-024-03260-y
Download citation
Received : 07 November 2023
Accepted : 15 January 2024
Published : 29 February 2024
DOI : https://doi.org/10.1186/s12916-024-03260-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Mental health
- Systematic review
- Umbrella review
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- Issue Brief
Exploring Barriers to Mental Health Care in the U.S.
Access to care and treatment for mental health issues remains out of reach for most of the population in the United States even though more than one-fifth of U.S. adults (21%, 52.9 million) had a mental illness 1 in 2020. 2 Even among individuals with insurance, issues such as a lack of available providers, inadequate insurance coverage, high out-of-pocket costs, and fragmented care persist. This brief defines the barriers to accessing mental health care in the United States and highlights the key focus areas policymakers should prioritize to improve access, coverage, and affordability of care.
This Isn’t New … and It’s Getting Worse
From 2008 to 2019, the number of adults aged 18 or older with any mental illness increased from 39.8 million to 51.5 million, a nearly 30% increase. 3 The pandemic has further exacerbated mental health problems for all ages; among adults aged 18 or older who had serious thoughts of suicide in 2020, more than one-fifth (21%) listed COVID-19 as the reason for those thoughts. 2 While progress has been made to reduce the stigma around mental health issues, the problem persists and prevents many people from accessing care. 4
The United States is also facing a growing youth mental health crisis. From 2009 to 2019, the share of high school students who reported experiencing persistent feelings of sadness or hopelessness increased 41%. 5 From 2010 to 2020, suicide death rates increased by 62% among adolescents aged 12 to 17. 6 In early 2021, emergency department visits for suicide attempts were 51% higher for adolescent girls and 4% higher for adolescent boys than in early 2019. 7 Furthermore, in October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared child and adolescent mental health a national emergency. 8
Mental Health Professional Shortages
The United States needs more mental health professionals. As of Sept. 30, 2021, an estimated 129.6 million people lived in one of the 5,930 federally designated mental health care Health Professional Shortage Areas. Less than one-third of the U.S. population (28%) lives in an area where there are enough psychiatrists and other mental health professionals available to meet the needs of the population — in fact, most states have fewer than 40% of the mental health professionals needed. The percentage of need met ranges from as low as 5% in the District of Columbia to 69% in New Jersey (Figure 1). 9 Additionally, more than half (51%) of counties in the United States have no practicing psychiatrists. 10
The shortage and maldistribution of mental health professionals across the country further impedes access to mental health care. Rural areas, where 14% of the U.S. population (or 46 million people) 11 live, have disproportionately low numbers of practicing mental health professionals compared with urban areas. Among nonmetropolitan counties, 65% had no practicing psychiatrist as compared with 27% of metropolitan counties. 8
While the number of aspiring psychiatrists matched to a medical residency program has grown over the past five years, 12 educating and training physicians takes over a decade. Psychologists, social workers, licensed therapists, and other mental health professionals who can be trained more quickly than psychiatrists play a critical role in expanding access to mental health care.

Navigating a Maze
Even when mental health providers are geographically accessible to patients, insured patients often find it difficult to find a provider who is in their insurance network and end up paying high out-of-pocket costs for out-of-network care; in some cases, they do not seek care at all.
In 2020, among adults aged 18 or older who had any mental illness in the past year and a perceived unmet need for services, 30% reported not receiving care because their health 3 insurance did not cover any mental health services or did not pay enough for mental health services. This number was similar for those with serious mental illnesses. 2
While the Mental Health Parity and Addiction Equity Act of 2008 mandates equal coverage and benefits for mental health and general medical conditions, gaps between insurance coverage for mental health conditions and other medical conditions still exist and are growing. 13 The insurance practices that are most likely to impede access to mental health care — including arbitrary medical necessity standards, network inadequacy, and fail-first approaches — remain pervasive among insurance companies. 14
For the 27.4 million 15 nonelderly individuals without insurance, accessing and affording mental health care is even more difficult, particularly in states that have not expanded their Medicaid programs. In 2019, adults aged 18 or older who had any mental illness in the past year were significantly more likely than those without any mental illness to be uninsured (10.8% versus 9.6%, respectively). 16 Uninsured adults with depression or anxiety were also more likely to not receive any treatment compared with their insured counterparts. 17
Who Is Really in My Insurance Network?
In a survey conducted by the National Alliance on Mental Illness (NAMI) in 2015, 1 in 4 respondents did not have a mental health therapist in their health plan’s network as compared with 1 in 10 who did not have a medical specialist in their health plan’s network. 18 Additionally, patients often find themselves wading through “ghost” or “phantom” networks — a directory of providers who supposedly take the patient’s insurance but who often do not take new patients, do not exist altogether, or are not “in network” with the insurance plan. A recent study found that in Oregon’s Medicaid managed care organizations, 67% of mental health prescribers and 59% of mental health nonprescribers were “phantom” providers who did not see Medicaid patients. 19 Due to these barriers, the patients who can afford to do so are much more likely to go out-of network for mental health services. A report analyzing claims data for commercial PPO plans covering 37 million individuals found that, in 2017, 17% of behavioral health office visits were to out-of-network providers as compared with 3% of office visits to primary care providers and 4% of office visits to medical/surgical specialists (Figure 2). 20 These differences were even greater in states like Alaska, where 64% of behavioral health office visits were out-of-network compared with 22% of primary care visits; New Jersey (41% versus 4%, respectively); and South Carolina (20% versus 4%, respectively). 15
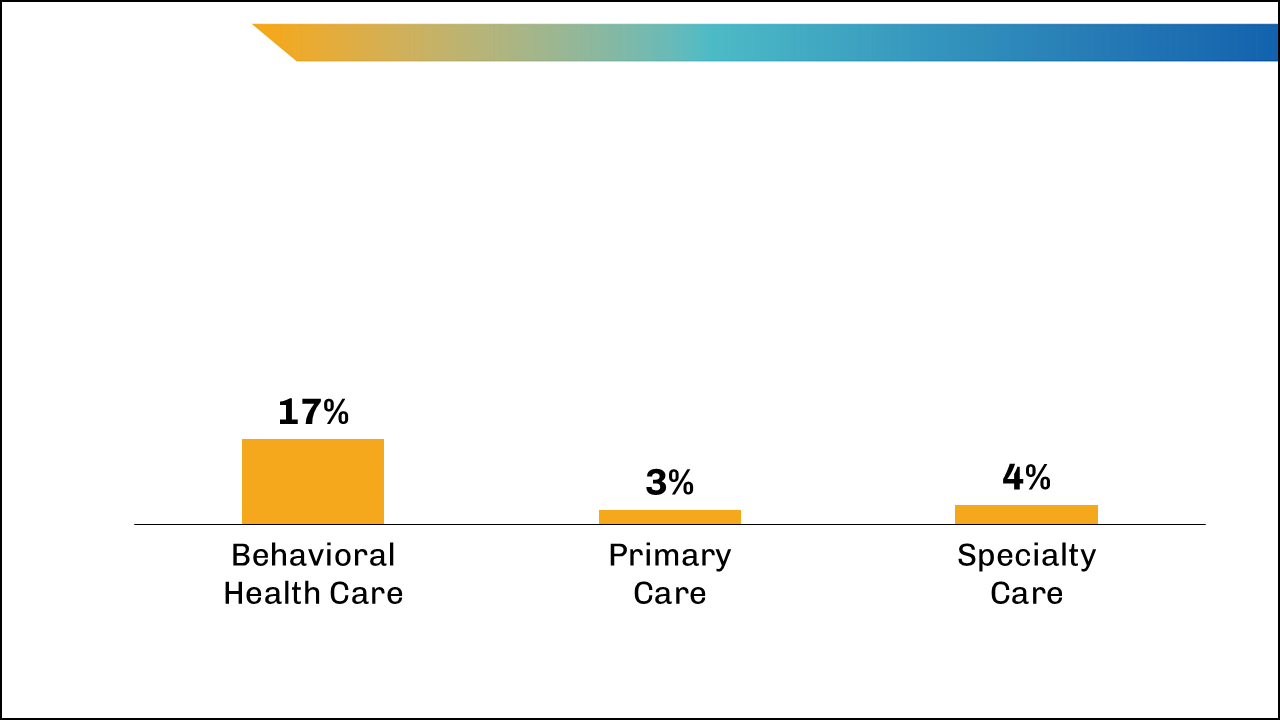
Patients who turn to their primary care providers (PCPs) for mental health services face a different set of barriers. In the 1980s, many insurers began “carving out” mental health benefits, meaning they outsource mental health services to different vendors that have their own unique network of doctors. However, patients and their PCPs are often unaware of this because insurance companies do not make this information widely available. As a result, PCPs do not get paid for rendering mental health services since they are often out-of-network with the vendor, and the cost ultimately gets passed on to the patient. 21 A study by KFF found that as of July 2021, 7 of the 41 states that contract with Medicaid managed care organizations always carved out specialty outpatient mental health services from their contracts. 22 Carve-outs (and the limited information on them), among other barriers, impede true parity of access to mental health care. 23
No Insurance Accepted
In addition to insurance network inadequacy, another pressing issue that is limiting access to mental health care is the large proportion of psychiatrists who do not accept insurance. A 2014 study found that only 55% of psychiatrists accepted private insurance as compared with 89% of physicians in other specialties in 2009-2010. The disparity was similar for Medicare and Medicaid. 24
Low reimbursement rates are the main driver of this disparity. For similar mental health services, nonpsychiatric medical doctors received anywhere from 13% to 20% higher in-network reimbursement than psychiatrists. On the other hand, for services provided out-of-network, the 5 median reimbursement was 6% to 28% higher for psychiatrists than for nonpsychiatric doctors. 25 These low reimbursements disincentivize mental health professionals from joining insurance networks. 26
Among mental health professionals who do accept insurance, reimbursement rates vary based on the insurance type. Providers are less likely to accept Medicaid or Medicare because their reimbursement rates are lower than private insurance. Despite being the largest payer for mental health care, 27 Medicaid generally reimburses providers at lower rates than both private insurance and Medicare, making access particularly difficult for patients with Medicaid coverage. A 2017 study found that only 46% of psychiatrists were willing to accept new patients covered by Medicaid; 75% were willing to accept new patients covered by Medicare and 69% were willing to accept new patients covered by private coverage. 28
First, Let’s … Fail?
The criteria for how insurance companies define the “medical necessity” of mental health services are inconsistent, which results in high rates of claim denials. In a 2015 survey conducted by NAMI, 29% of respondents reported that they or their family member had been denied mental health care because their insurance company had deemed the care medically unnecessary; conversely, only 14% of respondents were denied general medical care for the same reason. 29 In 2020, one-fifth of the approximately 765,000 medically necessary claims for behavioral health services were denied. 30
Insurance companies usually adopt these restrictive practices, which also include paying mental health providers lower rates than other medical providers and excluding mental health providers from insurance networks, in an attempt to lower costs by increasing barriers to care.
Insurance companies may also reduce patient access to mental health services in ways that do not clearly violate parity standards. Insurance companies often employ a “fail-first” strategy for mental health services, meaning that they will cover a more expensive treatment only after a patient shows no improvement through a cheaper treatment. Such strategies impede timely access to care and worsen outcomes. As a result, care is often guaranteed only when patients are in crisis, and even then, care depends on providers and other resources being available to them.
What Can Be Done?
Integrating and coordinating care .
One-third of adults aged 18 or older who reported having a mental illness and an unmet need for services indicated that they did not receive care because they did not know where to go for services. 2
Historically, diagnosis and treatment of mental health illnesses have been separated from physical illnesses. Different health care providers work in their own silos, and collaboration to coordinate a patient’s care is not standard practice. This is driven by a combination of factors including a lack of integrated technology and training, regulations and laws, and misaligned payment incentives.
PCPs often serve as the entry point into the care system for patients. As a result, patients with mental health illnesses are more likely to discuss them with a primary care doctor than with psychiatrists or other health professionals (Figure 3). Additionally, over one-third of the care and one-quarter of the medication prescribing for patients with serious mental illnesses was done by PCPs. 31 Primary care settings play an important role in providing mental health services and treatment, but PCPs often lack time, training, and resources to do so effectively on their own.
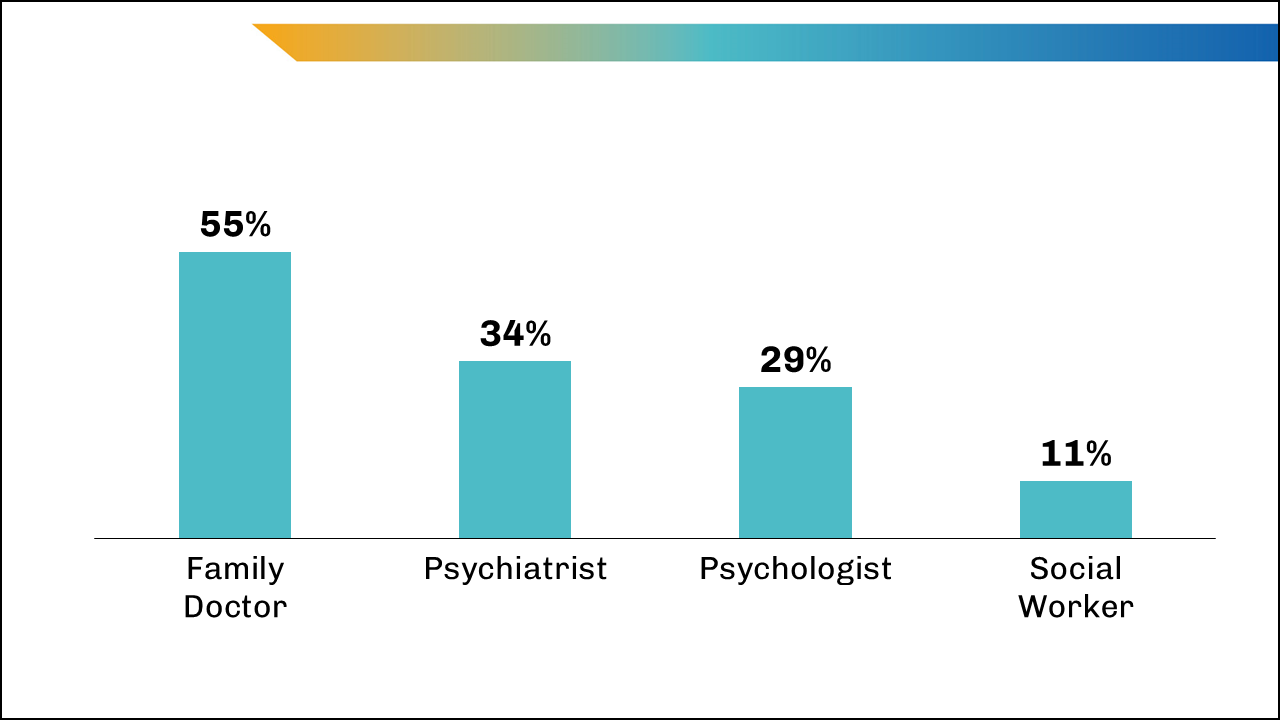
One issue is the lack of electronic health record (EHR) usage among mental health providers in nonprimary care settings. A 2012 report found that only 20% of behavioral health practices had adopted EHRs while 60% of other health care providers had done so. 32 A 2016 study found that for 27% of patients with depression and 28% with bipolar disorder, their primary care records showed no indication of their mental illness. 33 Missing information about previous diagnoses and treatment can harm patients. An incomplete picture of the patient’s health can lead to medication errors, under- or over-diagnosing, and mismanagement of comorbid conditions.
While primary care settings may be the most accessible entry point to mental health care for many patients, PCPs are already stretched thin and many are unable to provide patients with even routine preventive and chronic care. 34 Moreover, fewer and fewer Americans have a primary care provider. 35
Given how frequently individuals bring up mental health concerns in primary care settings, and the fact that PCPs may not have the time or training to treat mental health issues, integrated systems that help PCPs coordinate care and connect patients with the right mental health provider can significantly improve access and outcomes. Many different types of integrated care models have emerged in recent years. Yet, implementation has lagged mainly due to fragmented reimbursement systems, regulatory barriers, and lack of interoperability.
Individuals with mental health issues tend to have a higher rate of physical comorbidities. 36 There is no doubt about the connection between the mind and body, and evidence suggests that for many commonly occurring chronic physical illnesses, treatment of comorbid mental health issues leads to improvement in both mental and physical health. 37 This is where integrated behavioral health, or “collaborative care,” comes into play. 38 Integrating and coordinating care across medical and behavioral health providers is crucial to delivering wholeperson care and is a first step toward taking a preventive approach to mental health care. Building models where trained psychologists or social workers practice within a primary care setting can bridge the divide between mental and physical health.
Investing in Technology
Telehealth has played a significant role in improving access to mental health care during the COVID-19 pandemic. In 2019, less than 1% of mental health and substance use care was accessed through telehealth, compared with 40% from March through August 2020. While telehealth use for other medical services has dropped by more than 50% since the return of inperson care, telehealth use for mental health and substance use services has remained fairly consistent, accounting for 36% of visits from March through August 2021. 39
Telehealth continues to play an important role in the ongoing pandemic and can be a promising near-term solution to expanding access to mental health care, especially in rural areas. Between March and August 2021, the proportion of patients in rural areas who used telehealth for mental health and substance use services was 55%, compared with 35% in urban areas. 39 However, preserving this heightened access to care and expanding these efforts largely relies on extending the policy and payment flexibilities implemented under the COVID-19 public health emergency. 40 In July 2022, the U.S. House of Representatives passed legislation that would help extend some of these telehealth policies for Medicare through 2024. 41 However, it remains to be seen whether it will be passed into law and whether these extensions will prompt lawmakers to consider permanent telehealth reform.
Enforce, Expand, Insure, and Enact
The United States does not currently have the capacity to provide the necessary mental health care to millions of people — nor is accessing such care easy for most patients. There are short- and long-term opportunities to create policies that prioritize growing the workforce, expanding insurance coverage for patients, increasing reimbursement rates for providers, and enforcing state and national parity laws.
In March 2022, the Biden administration proposed a $700 million investment to expand the mental health workforce in rural and other underserved areas. 42 While Biden’s proposal showed that policymakers are increasingly recognizing the problem of workforce shortages in mental and behavioral health, Congress has yet to allocate any such funding as of September 2022. Funding is crucial to solving these workforce shortages, and Congress needs to invest in programs to recruit and train more mental health professionals. 8
Expanding the workforce is necessary but it cannot alone ensure patients can access care in the near term. If existing mental health professionals continue to be excluded from insurance networks, patients will continue facing barriers to accessing care. 43
Furthermore, the low reimbursement rates for mental health professionals further disincentivize them from accepting insurance. Policymakers should consider implementing policies that ensure mental health professionals can join insurance networks and increase reimbursement rates for these professionals. In addition, insurers and policymakers need to make greater efforts to ensure all patients seeking care have reliable insurance, including coverage for mental and behavioral health services.
Medicaid is the largest payer for mental and behavioral health services in the country, 27 but because 12 states have not expanded their Medicaid programs as of Sept. 20, 2022, 44 many individuals (2.2 million as of 2019) fall into the coverage gap 45 — meaning they are uninsured because they do not meet the eligibility requirements for Medicaid but cannot afford private insurance. Closing the coverage gap through Medicaid expansion would increase the number of insured individuals and expand access to health care for millions of people.
The varying definitions of “medical necessity” across states further impedes access, coverage, and affordability of care. While the Mental Health Parity and Addiction Equity Act of 2008 was created to provide equal coverage and benefits for mental health and substance use services and for physical health, insurers have found ways to skirt parity rules, particularly during the pandemic. 46 In 2020, California passed a law that requires insurers to expand medical necessity determinations to “generally accepted standards of mental health and substance use disorder care,” meaning they must evolve their definitions of necessity to reflect current standards of care. 47 Both state and national policies must compel insurers to expand medical necessity determinations to enhance access and coverage. However, policies expanding medical necessity determinations must be enacted together with policies addressing network inadequacy. Focusing solely on medical necessity can only help so much if providers do not accept insurance.
Telehealth has garnered more national attention and has been used more than before the COVID-19 pandemic. Despite the large increases in telehealth use, particularly for mental and behavioral health services, coverage for these services remains limited. While the U.S. House of Representatives has passed legislation to extend telehealth access, these policies need to become long-term changes. Expanding the use of technology that makes health care more convenient for patients, like telehealth, and ensuring that insurance companies cover care delivered through such technology over the long term, will allow many more people to access health care, as shown during the pandemic. However, providers will need to keep up with the increased demand, so policymakers’ efforts to expand the use of technology in health care should align with efforts to increase the number of mental health professionals.
Finally, policymakers should make a greater effort to enact policies that integrate mental and physical health. While many PCPs are stretched thin, these providers are often a patient’s first point of entry into the health care system. Our health care system must both implement models in which PCPs are more appropriately equipped to triage mental health issues and promote greater collaboration and coordination among primary care and mental health providers. The integrated behavioral health model requires training, costs, and changes to current systems, but it serves patients better. Furthermore, physicians favor the model. 48
With a growing share of the population reporting mental health and substance use issues, policymakers need to prioritize expanding access, coverage, and affordability of care. In the near term, expanding Medicaid coverage across all states, enforcing parity laws that have an evolving definition of medical necessity across all insurers, expanding coverage of telehealth services, and integrating mental health care into the primary care setting will all provide immediate benefits to millions of Americans.
Download Brief
Cite this source: Modi H, Orgera K, Grover A. Exploring Barriers to Mental Health Care in the U.S. Washington, DC: AAMC; 2022. https://doi.org/10.15766/rai_a3ewcf9p
- The 2019 National Survey on Drug Use and Health (NSDUH) classified adults with any mental illness as adults who had any mental, behavioral, or emotional disorder in the past year of sufficient duration to meet DSM-IV criteria.
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, SAMHSA. https://www.samhsa.gov/data/ . Accessed Aug. 1, 2022.
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, SAMHSA. https://www.samhsa.gov/data/ . Accessed Aug. 1, 2022.
- Weinberger A, Gbedemah M, Martinez A, Nash D, Galea S, Goodwin, R. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018;48(8):1308-1315. doi:10.1017/S0033291717002781.
- Centers for Disease Control and Prevention. Youth Risk Behavior Survey: Data Summary and Trends Report, 2009-2019. CDC; 2020. https://www.cdc.gov/healthyyouth/mental-health/index.htm. Accessed July 8, 2022 .
- Panchal N, Rudowitz R, Cox C. Recent Trends in Mental Health and Substance Use Concerns Among Adolescents. Washington, DC: KFF; June 28, 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/recent-trends-in-mental-health-and-substance-use-concerns-among-adolescents/ . Accessed July 6, 2022.
- American Academy of Pediatrics. AAP-AACAP-CHA declaration of a national emergency in child and adolescent mental health. https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/ . Published Oct. 19, 2021. Accessed July 6, 2022.
- U.S Department of Health and Human Services. Protecting Youth Mental Health. https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf . Accessed July 20, 2022.
- KFF. State Health Facts. Mental Health Care Health Professional Shortage Areas (HPSAs) as of Sept. 30, 2021. San Francisco, CA: KFF. https://www.kff.org/other/state-indicator/mental-health-care-health-professional-shortage-areas-hpsas/ . Accessed July 6, 2022.
- Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, Larson EH. Geographic variation in the supply of selected behavioral health providers. Am J Prev Med. 2018;54(6):S199-S207. https://doi.org/10.1016/j.amepre.2018.01.004 . Accessed July 6, 2022.
- Dobis EA, Krumel TP, Cromartie J, Conley K, Sanders A, Ortiz R. Rural America at a Glance. U.S. Department of Agriculture, Economic Research Service; November 2021. https://www.ers.usda.gov/webdocs/publications/102576/eib-230.pdf . Accessed July 8, 2022.
- National Resident Matching Program. National Resident Matching Program, Results and Data: 2022 Main Residency Match. NRMP; May 2022. https://www.nrmp.org/wp-content/uploads/2022/05/2022-Main-Match-Results-and-Data_Final.pdf . Accessed July 8, 2022.
- Centers for Medicare and Medicaid Services (CMS). The Mental Health Parity and Addiction Equity Act (MHPAEA). https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/mhpaea_factsheet . Accessed July 8, 2022.
- O’Connor K. Government steps up efforts to enforce parity law. Psychiatr News. 2022;57(3). https://doi.org/10.1176/appi.pn.2022.03.3.32 . Accessed July 11, 2022.
- Tolbert J, Orgera K, Damico A. What Does the CPS Tell Us About Health Insurance Coverage in 2020? San Francisco, CA: KFF; Sept. 23, 2021. https://www.kff.org/uninsured/issue-brief/what-does-the-cps-tell-us-about-health-insurance-coverage-in-2020/ . Accessed April 21, 2022.
- U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health 2019 (NSDUH-2019-DS0001). https://datafiles.samhsa.gov/ . Accessed July 8, 2022.
- Panchal N, Rae M, Saunders H, Cox C, Rudowitz R. How Does Use of Mental Health Care Vary by Demographics and Health Insurance Coverage? Washington, DC: KFF; March 24, 2022. https://www.kff.org/health-reform/issue-brief/how-does-use-of-mental-health-care-vary-by-demographics-and-health-insurance-coverage/ . Accessed Aug. 9, 2022.
- National Alliance on Mental Illness (NAMI). Out-of-Network, Out-of-Pocket, Out-of-Options: The Unfulfilled Promise of Parity. Arlington, VA: NAMI; November 2016. https://www.nami.org/Support-Education/Publications-Reports/Public-Policy-Reports/Out-of-Network-Out-of-Pocket-Out-of-Options-The/Mental_Health_Parity2016.pdf . Accessed July 8, 2022.
- Pifer R. “Phantom” provider lists limit Medicaid mental healthcare access, study finds. Healthcare Dive. https://www.healthcaredive.com/news/phantom-provider-networkst-medicaid-mental-health-care-access-Health-affairs/626617/ . Published July 6, 2022. Accessed July 12, 2022.
- Melek S, Davenport S, Gray TJ. Addiction and Mental Health vs. Physical Health: Widening Disparities in Network Use and Provider Reimbursement. Milliman Research Brief. November 2019. https://assets.milliman.com/ektron/Addiction_and_mental_health_vs_physical_health_Widening_disparities_in_network_use_and_provider_reimbursement.pdf . Accessed July 12, 2022.
- Pattani A. Patients seek mental health care from their doctor but find health plans standing in the way. Kaiser Health News. https://khn.org/news/article/primary-care-mental-health-insurance-barriers/ . Published July 12, 2022. Accessed July 21, 2022.
- Guth M. State Policies Expanding Access to Behavioral Health Care in Medicaid. Washington, DC: KFF; Dec 9, 2021. https://www.kff.org/medicaid/issue-brief/state-policies-expanding-access-to-behavioral-health-care-in-medicaid/ . Accessed Aug. 9, 2022.
- Charlesworth CJ, Zhu JM, Horvitz‐Lennon M, McConnell KJ. Use of behavioral health care in Medicaid managed care carve‐out versus carve‐in arrangements. Health Serv Res. 2021;56(5):805-816. https://doi.org/10.1111/1475-6773.13703 . Accessed Aug. 9, 2022.
- Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181. doi:10.1001/jamapsychiatry.2013.2862. Accessed July 6, 2022.
- Mark TL, Olesiuk W, Ali MM, Sherman LJ, Mutter R, Teich JL. Differential reimbursement of psychiatric services by psychiatrists and other medical providers. Psychiatr Serv. 2017;69(3):281-285. https://doi.org/10.1176/appi.ps.201700271 .
- U.S. Government Accountability Office. Report to the Chairman, Committee on Finance, U.S. Senate: Mental Health Care, Access Challenges for Covered Consumers and Relevant Federal Efforts. Washington, DC: GAO; March 2022. https://www.gao.gov/assets/gao-22-104597.pdf . Accessed July 8, 2022.
- Centers for Medicare and Medicaid Services, Medicaid.gov. Behavioral health services. https://www.medicaid.gov/medicaid/benefits/behavioral-health-services/index.html . Accessed July 8, 2022.
- Medicaid and CHIP Payment and Access Commission (MACPAC). Physician Acceptance of New Medicaid Patients: Findings From the National Electronic Health Records Survey. Washington, DC: MACPAC; June 2021. https://www.macpac.gov/wp-content/uploads/2021/06/Physician-Acceptance-of-New-Medicaid-Patients-Findings-from-the-National-Electronic-Health-Records-Survey.pdf . Accessed July 8, 2022.
- NAMI. A Long Road Ahead: Achieving True Parity in Mental Health and Substance Abuse Care. Arlington, VA: NAMI; April 2015. https://www.nami.org/Support-Education/Publications-Reports/Public-Policy-Reports/A-Long-Road-Ahead/2015-ALongRoadAhead . Accessed July 18, 2022.
- Pollitz K, Rae M, Mengistu S. Claims Denials and Appeals in ACA Marketplace Plans in 2020. Washington, DC: KFF; July 5, 2022. https://www.kff.org/private-insurance/issue-brief/claims-denials-and-appeals-in-aca-marketplace-plans/ . Accessed July 18, 2022.
- Jetty A, Petterson S, Westfall JM, Jabbarpour Y. Assessing primary care contributions to behavioral health: a cross-sectional study using medical expenditure panel survey. J Prim Care Community Health. 2021; 12. https://doi.org/10.1177/21501327211023871 .
- McGregor B, Mack D, Wrenn G, Shim RS, Holden K, Satcher D. Improving service coordination and reducing mental health disparities through adoption of electronic health records. Psychiatr Serv. 2015;66(9):985-987. https://doi.org/10.1176/appi.ps.201400095
- Madden JM, Lakoma MD, Rusinak D, Lu CY, Soumerai SB. (2016, April 14). Missing clinical and behavioral health data in a large electronic health record (EHR) system. J Am Med Inform Assoc. 2016;23(6):1143-1149. https://doi.org/10.1093/jamia/ocw021 .
- Privett N, Guerrier S. Estimation of the time needed to deliver the 2020 USPSTF preventive care recommendations in primary care. Am J Public Health. 2021;111(1):145-149. doi: 10.2105/AJPH.2020.305967. Epub 2020 Nov 19. PMID: 33211585; PMCID: PMC7750618.
- Finnegan J. Number of Americans with a primary care provider declined 2% over a decade, new study shows. Fierce Healthcare. https://www.fiercehealthcare.com/practices/moving-wrong-direction-fewer-americans-have-a-primary-care-provider-new-study-shows . Published Dec. 17, 2019. Accessed July 8, 2022.
- Ramanuj P, Ferenchik E, Docherty M, Spaeth-Rublee B, Pincus HA. Evolving models of integrated behavioral health and primary care. Curr Psychiatry Rep. 2019;21(1). https://doi.org/10.1007/s11920-019-0985-4 .
- Katon WJ, Lin EH, von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611-2620. https://doi.org/10.1056/nejmoa1003955 .
- Weiner S. A growing psychiatrist shortage and an enormous demand for mental health services. AAMCNews. https://www.aamc.org/news-insights/growing-psychiatrist-shortage-enormous-demand-mental-health-services . Published Aug. 9, 2022. Accessed August 25, 2022.
- Lo J, Rae M, Amin K, Cox C, Panchal N, Miller BF. Telehealth Has Played an Outsized Role Meeting Mental Health Needs During the COVID-19 Pandemic. Washington, DC: KFF; March 22, 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/telehealth-has-played-an-outsized-role-meeting-mental-health-needs-during-the-covid-19-pandemic/ . Accessed July 20, 2022.
- Health Resources and Services Administration, telehealth.hhs.gov. Policy changes during COVID-19. https://telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/ . Accessed July 8, 2022.
- Morse S. House passes bill extending telehealth waivers through 2024. Healthcare Finance. https://www.healthcarefinancenews.com/news/house-passes-bill-extending-telehealth-waivers-through-2024/ . Published July 28, 2022. Accessed Aug. 20, 2022.
- The White House. Fact sheet: President Biden to announce strategy to address our national mental health crisis, as part of unity agenda in his first State of Union. https://www.whitehouse.gov/briefing-room/statements-releases/2022/03/01/fact-sheet-president-biden-to-announce-strategy-to-address-our-national-mental-health-crisis-as-part-of-unity-agenda-in-his-first-state-of-the-union . Published March 1, 2022. Accessed July 8, 2022.
- Koons C, Tozzi J. As suicides rise, insurers find ways to deny mental health coverage. Bloomberg. https://www.bloomberg.com/news/features/2019-05-16/insurance-covers-mental-health-but-good-luck-using-it . Published May 16, 2019. Accessed July 8, 2022.
- KFF. State Health Facts: Status of State Action on the Medicaid Expansion Decision, September 20, 2022. Washington, DC: KFF. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ . Accessed Aug. 7, 2022.
- Garfield R, Orgera K, Damico A. The Coverage Gap: Uninsured Poor Adults in States That Do Not Expand Medicaid. Washington, DC: KFF; Jan. 21, 2021. https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/ . Accessed Aug. 12, 2022.
- Huetteman E. Mental health services wane as insurers appear to skirt parity rules during pandemic. Kaiser Health News. https://khn.org/news/article/gao-report-mental-health-services-wane-as-insurers-appear-to-skirt-parity-rules-during-pandemic/ . Published April 30, 2021. Accessed Aug. 9, 2022.
- Lara R. Enactment of Senate Bill 855 – Submission of Health Insurance Policies for Compliance Review [notice to health insurers]. Sacramento, CA: California Department of Insurance. Published Dec.10, 2020. http://www.insurance.ca.gov/0250-insurers/0300-insurers/0200-bulletins/bulletin-notices-commiss-opinion/upload/Notice-to-Health-Insurers-re-Requirements-of-Senate-Bill-855.pdf . Accessed July 8, 2022.
- Miller-Matero LR, Dykuis KE, Albujoq K, et al. Benefits of integrated behavioral health services: the physician perspective. Fam Syst Health. 2016;34(1):51-5. doi: 10.1037/fsh0000182. PMID: 26963777.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- About the Acting NIMH Director
- Advisory Boards and Groups
- Strategic Plan
- Offices and Divisions
- Careers at NIMH
- Staff Directories
- Getting to NIMH

Addressing Disparities: Advancing Mental Health Care for All Americans
By Joshua Gordon
January 29, 2020
As I sit down to write this message, I’m thinking of two former patients. One of them, a Hispanic man, I met in the emergency room at New York-Presbyterian Hospital when I was a resident in the early 2000s. Floridly psychotic, disheveled, and homeless, he was shouting at the emergency room nurse when I first saw him, demanding medications that he said were stolen from a locker in the homeless shelter across the street. The second patient, a White woman, was referred to my private practice in Midtown Manhattan a few years later. Composed and controlled, she asked compelling questions about her illness and its management, bringing with her dozens of pages of medical records. Both patients were young adults. Both had severe bipolar disorder . Both had survived a suicide attempt. Their medication lists were the same. Their lives were not.
Differences in health outcomes like these can reflect a number of underlying factors, including biological factors or environmental exposures; social, economic, and cultural contexts; and access to quality health care. When these differences adversely affect disadvantaged populations, they are known as health disparities .
Disparities in mental health are significant and easily documented. Deaths by suicide, for example, are much more common in American Indians and Alaska Natives compared to the general population. The rate of deaths by suicide is also higher in rural areas . Another example: Black and Hispanic children may be diagnosed with autism at a later age compared to White children. That is an important factor because the earlier the diagnosis, the earlier treatment can start, and the earlier treatment starts, the better these children will do. These and other mental health disparities further disadvantage members of minority groups and increase the burden of mental illnesses on individuals, families, and communities.
Accordingly, the National Institute of Mental Health (NIMH) supports a research agenda aimed at understanding and reducing mental health disparities. One early success comes from research led by Emily Haroz, Ph.D. , a promising early-career investigator at the Johns Hopkins Bloomberg School of Public Health. Using an approach that has worked for the U.S. Army, the U.S. Department of Veterans Affairs, and a group of health management organizations (HMOs), Haroz and colleagues built an algorithm that uses electronic health record data to identify individuals in the White Mountain Apache Tribe in Arizona who are at increased risk of suicide. Such a predictor could be used by health professionals to refer these individuals to appropriate mental health care. Meanwhile, NIMH continues to support three hubs for collaborative research focused on suicide prevention in Native American communities. These hubs are busy establishing common protocols for novel interventions and testing the efficacy of these interventions. This research holds the promise of making a real difference in the near term, helping health professionals and community leaders understand how to reduce deaths by suicide in their communities.
Similar efforts are underway in other communities to help families with children who may have autism. The Autism Spectrum Disorder Pediatric, Early Detection, Engagement and Services Network (ASD PEDS) is an NIMH-funded network of investigators studying a diverse array of strategies and interventions aimed at identifying and treating children with autism as early as possible. This collaborative group is committed to eliminating disparities by reducing the age at which children from underserved populations are diagnosed and has several projects that are nearing completion. For example, Alice Carter, Ph.D. , at the University of Massachusetts Boston, is finishing a study designed to test whether a system-level intervention can reduce these disparities. The intervention involves outreach to primary care pediatricians, a comprehensive multi-stage screening process, and motivational interviewing with parents and other caregivers. Wendy Stone, Ph.D. , at the University of Washington, is testing a complementary intervention that aims to reduce disparities by improving screening and referral procedures in primary care pediatric practices. Stone and colleagues will examine the acceptability and efficacy of the intervention in four diverse communities.
While we at NIMH are justifiably proud of these and other investments in research on mental health disparities, I can’t help but ask whether similar projects would remedy the disparate situations faced by my former patients. Would early intervention have saved my first patient from homelessness? Are there treatment approaches for bipolar disorder that work better for individuals from disadvantaged backgrounds? How can we promote better access to and engagement in community-based mental health care? These are the sorts of questions we need to answer to ensure that improved mental health care meets the needs of all Americans.
Allen. J., Rasmus, S. M., Fok, C. C. T., Charles, B., Henry, D., & Qungasvik Team. (2018). Multi-level cultural intervention for the prevention of suicide and alcohol use risk with Alaska Native youth: A nonrandomized comparison of treatment intensity. Prevention Science, 19 (2), 174-185. doi:10.1007/s11121-017-0798-9
Daniels, A. M., & Mandell, D. S. (2014). Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism, 18 (5), 583-597. doi: 0.1177/136236131348027
Haroz, E. E., Walsh, C. G., Goklish, N., Cwik, M. F., O'Keefe, V., & Barlow, A. (2019). Reaching those at highest risk for suicide: Development of a model using machine learning methods for use with Native American communities. Suicide and Life-Threatening Behavior . doi:10.1111/sltb.12598
Ibañez, L. V., Stoep, A. V., Myers, K., Zhou, C., Dorsey, S., Steinman, K. J., Stone, W. L. (2019). Promoting early autism detection and intervention in underserved communities: Study protocol for a pragmatic trial using a stepped-wedge design. BMC Psychiatry, 19 , 169. doi:10.1186/s12888-019-2150-3
Ivey-Stephenson, A. Z., Crosby, A. E., Jack, S. P., Haileyesus, T., & Kresnow-Sedacca, M. (2017). Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death — United States, 2001–2015. MMWR Surveillance Summary , 66 (No. SS-18), 1–16. doi:10.15585/mmwr.ss6618a1
O'Keefe, V. M., Haroz, E. E., Goklish, N., Ivanich, J., The Celebrating Life Team, Cwik, M. F., & Barlow, A. (2019). Employing a sequential multiple assignment randomized trial (SMART) to evaluate the impact of brief risk and protective factor prevention interventions for American Indian youth suicide. BMC Public Health, 19 , 1675. doi:10.1186/s12889-019-7996-2.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 21 July 2023
Psychedelic therapies reconsidered: compounds, clinical indications, and cautious optimism
- Jennifer M. Mitchell ORCID: orcid.org/0000-0002-7567-8129 1 , 2 , 3 , 4 &
- Brian T. Anderson 2 , 4
Neuropsychopharmacology volume 49 , pages 96–103 ( 2024 ) Cite this article
7313 Accesses
9 Citations
24 Altmetric
Metrics details
- Neuroscience
The clinical investigation of psychedelic medicines has blossomed over the last 5 years. Data from a Phase 3 industry trial and a multicenter Phase 2 industry trial, in addition to multiple early phase investigator-initiated and industry trials, have now been published in peer-reviewed journals. This narrative review summarizes both the recent data and the current clinical trials that are being conducted with various classes of “psyche-manifesting” substances, which may prove beneficial in the treatment of a broad range of conditions. Methodological considerations, unique challenges, and next steps for research are discussed in keeping with the uniquely “experiential” nature of these therapies.
Similar content being viewed by others

Psychedelics: preclinical insights provide directions for future research

Could psychedelic drugs have a role in the treatment of schizophrenia? Rationale and strategy for safe implementation
Treatment resistance in psychiatry: state of the art and new directions
Introduction.
The past few years have ushered in a renewed wave of psychedelic interest and research that has led to the clinical testing of multiple psychedelic agents for various health conditions. Australia and Canada have even recently approved the clinical use of certain psychedelic medicines under restricted circumstances [ 1 , 2 ]. However, along with this renewed wave of interest has come a series of challenges with respect to the taxonomy of psychedelics, the implementation of best practices for the evaluation of psychedelic therapies, and the capacity to stay abreast of developments in this rapidly expanding scientific field. Here we review the contemporary clinical research to provide an overview of the different classes of psychedelics currently under investigation for clinical use, their proposed indications, and—because they are “experiential medicines”—considerations for their judicious use.
Psychedelics have long been implicated in the treatment of mood and anxiety disorders, as well as disorders related to impulsivity, repetitive behaviors, and impaired decision-making, such as alcohol and other substance use disorders [ 3 , 4 , 5 ]. Yet the clinical promise of mid-20th Century psychedelic research was ultimately overshadowed by methodological limitations [ 6 ], regulatory restrictions, and a political landscape that made psychedelic research all but untenable for several decades [ 7 ]. Current biomedical theories speculate that psychedelic therapies improve clinical functioning by regulating affective states (such as anhedonia) and self-referential cognitive processes and may therefore ultimately involve interrelated neural circuits across a broad range of conditions [ 8 , 9 ]. Along these lines, the current clinical research landscape has expanded significantly compared to even a few years ago [ 10 ], and now includes evaluations of the effects of psychedelic therapies in a wide array of diagnostic categories, including mood disorders, substance use disorders, obsessive compulsive and related disorders, trauma-related disorders, and disorders of dysfunctional coping such as pathological grief and end of life distress. Typically, when investigated as therapies for psychiatric conditions, psychedelics are administered as adjuncts to a brief course of behavioral therapy to mitigate the risk of adverse events and to augment efficacy [ 11 , 12 ].
In addition to psychiatric indications, psychedelics are also being studied more generally as neuroplastic agents, potentially capable of inducing change in intractably crystalized neurological pathways. As such, they are being pursued as therapeutics for age-related degenerative conditions—including Alzheimer’s and Parkinson’s—as well as for pain, headache and migraine, autism, and visual impairments. Only time will tell if these compounds can reverse ingrained neurological processes, perhaps by enabling neuroplasticity, to the point where previously inflexible systems can be adjusted and reset.
Defining psychedelic
The original definition of the term psychedelic , as coined by the psychiatrist Humphry Osmond, is “mind-” or “soul-manifesting”, and as such is independent of biological mechanism. With this definition in mind, drugs that activate the serotonin 5-HT2A receptor directly (typically termed classic psychedelics) [ 13 ] as well as those that activate serotonin receptors indirectly or not at all, or that work through binding to a combination of receptors (including glutamatergic, dopaminergic, and opioidergic receptors) would all be considered psychedelic if they demonstrate the capacity for allowing greater access to the psyche in a manner similar to the classic psychedelics. Therefore, this review will include a series of drugs that meet the original definition of psychedelic for which there exists preliminary evidence from modern trials of the potential to affect psychotherapeutic change in humans. Some atypical, or non-classic, psychedelics are also included here; these are drugs with psychoactive effects that are not primarily or uniquely mediated through the activation of the 5-HT2A receptor. The decades-long history of the use of substances like ketamine [ 14 , 15 ] and psychedelic amphetamines like 3,4-methelenedioxyamphetamine (MDA) [ 16 ] in psychedelic therapy suggests that a comprehensive review of psychedelic therapies should include drugs beyond the classic psychedelics.
While the term hallucinogen is often colloquially substituted for the term psychedelic, hallucinogens are a category of drugs that induce perceptions in the absence of external stimuli (as opposed to inducing perceptual distortions of extant stimuli). Therefore, although there is some overlap in the categories of hallucinogen and psychedelic, here we will only use the term psychedelic, as we are summarizing effects that are more broadly relevant to processes of psychotherapeutic change, and not limited to perceptual alterations per se. With these definitions in mind, and considering the available data and currently registered trials, the modern clinical investigation of the following classic and atypical psychedelics (henceforth, collectively referred to as “psychedelics”) will be discussed in this review: ayahuasca, N,N-dimethyltrypatmine (DMT) and 5-methoxy-DMT (5-MeO-DMT), ibogaine, ketamine, lysergic acid diethylamide (LSD), 3,4-methylenedioxymethamphetamine (MDMA), mescaline, salvinorin A, and psilocybin. In addition, as psychedelics are thought to be “experiential medicines” affected by both set and setting [ 17 , 18 , 19 ], attention will also be focused on the environmental and psychological conditions that modulate the therapeutic efficacy of psychedelics.
Many psychedelic molecules have structural similarities that may enable specific signaling mechanisms. However, molecular differences allow them to be divided into indolamines (including the ergolines and simple tryptamines), phenethylamines, diterpines, and cyclohexanones. Each of these will be discussed in turn in an attempt to provide the reader an up-to-date view of the rapidly evolving field of clinical research into psyche -manifesting drugs.
Indolamines
Ibogaine is an indolamine that is derived from the West African Tabernanthe iboga bush that has long been used as part of the Bwiti religious tradition in the jungles of Gabon [ 20 ]. Ibogaine binds dopamine and serotonin (5-HT) receptors, acts as both an NMDA and a3b4-nicotinic receptor antagonist, and acts as a kappa opioid receptor agonist [ 21 ]. Although ibogaine was originally touted as an anti-addiction medication as far back as the 1960s https://www.nytimes.com/2010/02/17/us/17lotsof.html , it took over 30 years for it to make its way into phase 1 clinical studies, which indicated that, although ibogaine has the potential to be an effective an anti-addiction therapeutic for a number of different substance use disorders [ 22 , 23 , 24 ], it also carries cardiac and neurological risks that complicate its use as a therapeutic [ 25 , 26 , 27 ]. A series of sudden and unexpected deaths halted phase 1 testing for drug abuse and dependence [ 25 , 28 ] and clinical trials have yet to resume in the United States, although there is growing political support for these studies [ 29 ].
Although ibogaine is a Schedule 1 substance and is not FDA approved, over the last few decades it has been administered at drug and alcohol treatment centers in Latin America and the Caribbean, and it is currently under investigation outside of the United States as a potential therapeutic for alcohol misuse (NCT03380728), and for drug use, dependence, and withdrawal (NCT04003948; NCT05029401). Recent data suggest that the potential negative impact of ibogaine on cardiac function can be controlled through careful screening and monitoring during drug administration [ 30 ] and that, as both ibogaine and methadone may induce QT prolongation (an alteration in cardiac ventricular repolarization that is associated with the Torsade de Pointes arrhythmia and increased risk of sudden cardiac death), care should be taken to ensure that those seeking ibogaine treatment for opioid use disorder are screened for the use of methadone and other QT prolonging drugs prior to ibogaine administration.
Elucidation of the mechanism(s) by which ibogaine exerts its clinical effects might lend insight into the contribution of various neurotransmitter systems to the clinical effectiveness of psychedelics, as ibogaine is perhaps one of the least pharmacologically specific, and yet most impactful, psychedelics currently under investigation.
Indolamines: Ergolines
Lysergic acid diethylamide (lsd).
LSD was first synthesized by the chemist Albert Hoffman during his employment with Sandoz Pharmaceuticals in the 1930s while he was searching for novel compounds to treat respiratory depression. LSD has since been shown to bind with high affinity to several 5-HT receptors [ 31 ] and also acts as a dopamine (D1, D2, D4) receptor agonist [ 32 , 33 ]. Potential clinical indications include alcohol and other substance use disorders [ 34 , 35 , 36 ], obsessive compulsive disorder [ 37 ], depression (now in phase 2), end of life anxiety [ 38 ], cluster headache [ 39 ], and attention-deficit hyperactivity disorder (ADHD) [ 40 ]. LSD has long been available through Compassionate Use laws in Switzerland as an adjunct to psychotherapy for the treatment of a number of different mental health conditions [ 41 ].
Although a substantial volume of data from the 1960s to 1970s suggest that LSD could be effective in decreasing alcohol consumption in self-ascribed, and self-selected, “alcoholics,” [ 42 ] and although a more recent meta-analysis that incorporated clinical data from 6 smaller studies demonstrated that a single dose of LSD resulted in a long-term decrease in alcohol “misuse,” [ 35 ] previous outcome measures were not collected using current methodological standards and should therefore be replicated to confirm and extend previous findings in a thoroughly characterized subject population with alcohol use disorder (AUD). Fortunately, a double-blind, placebo-controlled, randomized, multisite study is currently being planned (NCT05474989) to evaluate the effects of two doses of LSD (150 µg for first dose followed by either 150 µg or 250 µg for second dose) on prevention of relapse to alcohol in a population with AUD. These data will hopefully provide insight into whether LSD does indeed hold promise as a potential therapeutic for AUD.
LSD has also recently completed early phase clinical testing for anxiety disorders (NCT03153579; NCT00920387) and the results have shown that LSD decreases anxiety while increasing quality of life [ 43 ] and also, importantly, that these effects are long-lasting [ 38 ]. In addition, a randomized, double-blind, placebo-controlled phase 2 trial of LSD for major depression (comparing two moderate to high doses of LSD = 100 µg/100 µg or 100 µg/200 µg, and two low doses of LSD = 25 µg/25 µg) has now been completed (NCT03866252), although these data were not yet available for review at the time of this publication. Lastly, a multisite, randomized, double-blind, placebo-controlled phase 2 trial is also currently being planned to further study the use of LSD for adults with ADHD (NCT05200936).
In addition to the mental health disorders listed above, both case (40. Sewell et al., 2006) and self-reports [ 44 ] indicate that LSD could be effective in combating cluster headache, and a double-blind, randomized, placebo-controlled phase 2 trial of LSD (3 doses of 100 mcg over 3 weeks) has recently been initiated to evaluate the efficacy of LSD for treatment of cluster headache (NCT03781128). Finally, as part of a drug development program for treating Alzheimer’s Disease, a recent double-blind randomized pilot trial of repeated (every 4 days) low doses of LSD (5 mcg vs 10 mcg vs 20 mcg vs placebo) in healthy older adults (age 55–75) found the drug to be well-tolerated in this population [ 45 ].
Indolamines: Simple tryptamines
Psilocybin is an active agent in Psilocybe mushrooms, which have been used ritualistically for thousands of years by Indigenous communities in Central and North America. Psilocybin exerts its psychedelic effects primarily through activation of 5HT2A receptors [ 46 ] and through activation of a 5-HT2AR-mGluR2 receptor complex [ 47 ]. Likely due to its well-established safety profile, minimal abuse potential, and short duration of subjective perceptual effects, psilocybin is currently the most broadly studied psychedelic for mental health conditions. Clinical indications under investigation currently include major depression [ 48 ], treatment-resistant depression [ 49 ], alcohol and other substance use disorders [ 50 ], smoking cessation [ 51 ], and OCD [ 52 ]. Psilocybin has also been studied in conjunction with individual and group psychotherapy for treating distress in patients with serious illness including cancer-related mood and anxiety disorders, and demoralization in long term AIDS survivors [ 53 ].
Not only has psilocybin been successfully administered for smoking cessation [ 51 , 54 ], but, intriguingly, it has also been shown that change in tobacco consumption following psilocybin administration is correlated with the degree of “mystical-type experience” reported by study participants, such that those reporting greater intensity of mystical-type experiences also report a greater decrease in smoking [ 54 ]. While there remains great debate over the nature and assessment of a “mystical-type experience”, high-dose psilocybin has repeatedly been reported by participants to be a spiritual or transcendent event, which seems to be an important contributor to treatment effectiveness [ 55 ] and, as such, merits further attention.
A modest-sized proof of principle phase 2 trial recently demonstrated the significant and long-lasting efficacy of psilocybin when combined with psychotherapy for the treatment of AUD ( 50 . Bogenschutz et al., 2022). Mechanistic (NCT04141501), head-to-head (NCT05421065), larger, multisite (NCT05646303), and other trials (NCT04620759) of psilocybin therapy for AUD are currently recruiting.
The most detailed exploration of psilocybin for a therapeutic indication thus far has been for treatment-resistant depression (TRD), and a recent, double-blind phase 2 study found a dose-dependent reduction in depression scores in the weeks following administration of a single dose of psilocybin (1 mg, 10 mg, or 25 mg) [ 56 ]. Similarly, a trial investigating the use of two psilocybin administration sessions in conjunction with therapy for major depressive disorder (MDD) not only found a significant attenuation in depression scores at both the primary endpoint and at the 4-week follow up [ 57 ] but also noted that these effects were still durable 1 year after psilocybin administration [ 58 ]. This trial also noted a correlation between mystical-type experience at the time of psilocybin administration and increased well-being at the 12-month follow-up. As multiple studies have noted a positive correlation between the lasting impact of psilocybin on mental health measures and mystical-type experiences, it will be interesting to note whether future studies will be able to elucidate the nature of the relationship between psilocybin-induced mystical-type experiences and durable alleviation of mental health conditions.
A myriad of additional phase 2 trials with psilocybin are now underway for a variety of other indications including PTSD (NCT05554094; NCT05243329; NCT05312151), OCD (NCT05370911; NCT04882839; NCT03300947; NCT05546658; NCT03356483), depression in bipolar 2 disorder (NCT0506529; NCT04433845), anorexia nervosa (NCT04656301; NCT04052568; NCT04661514; NCT05481736; NCT04505189), binge eating (NCT05035927), fibromyalgia (NCT05548075; NCT05128162; NCT05068791), phantom limb pain (NCT05224336), migraine (NCT03341689; NCT04218539), cluster headache (NCT02981173), concussion headache (NCT03806985). Multiple trials are assessing psilocybin therapy for distress associated with serious medical illness (NCT04950608; NCT05398484; NCT05506982; NCT04522804; NCT05220046; NCT04593563; NCT05403086). In addition, a series of studies have been evaluating the potential of psilocybin to attenuate methamphetamine use disorder (NCT04982796; NCT05322954) and cocaine use disorder (NCT02037126). With any luck, the next couple of years should further quantify the myriad of potential therapeutic uses of psilocybin.
Ayahuasca is typically an admixture of the Banisteriopsis caapi vine, containing MAO-inhibiting beta-carboline alkaloids, and the DMT-containing leaves of the Psychotria viridis shrub, although other plants, such as Diplopterys cabrerana , are at times used to make decoctions that are also referred to as ayahuasca. The drink has been used ceremonially in the Amazon Basin for at least hundreds of years and is used widely today in shamanic and other religious contexts within and outside of South America [ 59 ]. Potential indications for ayahuasca include alcohol and other substance use disorders, anxiety and depression disorders [ 60 ] and possibly prolonged grief disorder [ 61 ] and eating disorders [ 62 ]. Naturalistic studies have indicated that regular users of ayahuasca consume less alcohol and other drugs compared to other populations [ 63 , 64 , 65 ], and that ritual participants self-report improved affective symptoms after drinking ayahuasca [ 66 ], however individuals with anxiety and mood disorders may also be at higher risk of experiencing adverse effects in rituals settings [ 67 ]. One recent placebo-controlled proof of principle trial has also shown that a single administration of ayahuasca can attenuate symptoms of treatment-resistant depression [ 68 ].
DMT & 5-MeO-DMT
N,N-Dimethyltryptamine (DMT) is a substituted tryptamine that constitutes one of the primary active ingredients in ayahuasca and is structurally similar to the psychedelic compounds 5-MeO-DMT and bufotenin (5-HO-DMT). In addition to high binding affinity at a number of 5-HT receptors, DMT acts as a TAAR agonist [ 69 ], and a sigma receptor agonist [ 70 ] and may mediate effects at metabotropic glutamate receptors [ 71 ]. Although the clinical data are currently limited, DMT is now being studied in a fixed order, open-label, dose-escalation study in participants with major depression (NCT04711915), and a double-blind, randomized, placebo-controlled study of intravenous DMT in subjects with major depressive disorder (MDD) has now been completed (NCT04673383). Because the subjective effects of DMT are short-lasting compared to other psychedelic compounds [ 72 ], DMT might lend itself more readily to use in clinical settings.
Phenethylamines
3,4-Methylenedioxymethamphetamine (MDMA) was originally synthesized by the pharmaceutical company Merck in 1912 as part of a research program on anticoagulating agents. Early case reports suggested that MDMA could be a remarkably effective catalyst in both individual and couples psychotherapy [ 73 , 74 ] for a variety of psychological issues. The psychedelic-like effects of MDMA were eventually immortalized by Alexander and Ann Shulgin in their book, PiHKAL [ 75 ].
MDMA acts on human monoamine transporters [ 76 ], though most of the subjective effects of MDMA are dependent on serotonin release, which MDMA potentiates through a series of different mechanisms. MDMA inhibits the 5-HT vesicular transporter (VMAT2) and activates the intracellular presynaptic terminal receptor (TAAR1), which impacts both the release and reuptake of serotonin [ 69 , 77 , 78 ]. Downstream of serotonin efflux, MDMA promotes the release of oxytocin [ 79 ], a neuromodulator shown to play a critical role in bonding and social interactions [ 80 ], which may therefore facilitate the therapeutic process by enabling participants to remain emotionally open while they explore difficult memories and subject matter.
MDMA most likely exerts its influence through effects within the amygdala, and previous human research indicates that MDMA attenuates left amygdalar responses to angry facial expressions and enhances ventral striatal responses to happy expressions [ 81 ]. More recent research has found that, when administered to subjects with severe PTSD, MDMA induces changes in functional connectivity between the left amygdala and both the left insula and bilateral posterior cingulate cortex during autobiographical memory recall [ 82 ]. Further experiments are needed to address individual differences in responsivity to MDMA and to determine if and how to maximize the effects of MDMA administration on retrieval and reconsolidation of negative memories.
MDMA is typically administered in conjunction with therapy and the combination of MDMA plus therapy is has recently been investigated for use in indications including PTSD [ 83 , 84 ], social anxiety in adults with [ 85 ] and without autism (NCT05138068), AUDs (NCT05709353), illness-related anxiety (NCT02427568), adjustment disorder (NCT05584826), fear extinction (NCT03527316), and eating disorders (NCT04454684). The most thoroughly investigated of these indications is currently PTSD. Indeed, MDMA for PTSD might well be the first psychedelic to be submitted to the FDA as part of a new drug application (NDA) for regulatory approval and is the only psychedelic to date to have completed phase 3 clinical trials. Phase 3 findings demonstrated that MDMA-therapy was both safe and effective in treating PTSD, functional disability, and symptoms of depression in a population with severe PTSD [ 83 ].
In addition to the current manualized inner-directed therapy that has been used in conjunction with MDMA administration in phase 3, several other studies are now underway to investigate the pairing of MDMA with other gold standard, manualized therapies for PTSD. Studies are being conducted to investigate the combination of MDMA plus exposure therapy for PTSD (NCT05746572), MDMA plus group therapy for Veterans with PTSD (NCT05173831), MDMA plus cognitive processing therapy for PTSD (NCT05067244), and MDMA plus cognitive behavioral conjoint therapy for couples with PTSD (NCT02876172). Also, because of its ability to potentiate self-compassion [ 86 ], MDMA could be particularly powerful in those suffering from moral injury in relation to PTSD.
Mescaline is currently found in four species of cacti: Bolivian Flame, Peruvian Flame, San Pedro, and Peyote, the last of which has been used in ritual by Native American communities for thousands of years [ 87 ]. It has long been used as a treatment for alcoholism within Native American communities [ 88 , 89 ].
Recent self-reported data (via an online questionnaire) indicate that mescaline may attenuate symptoms of anxiety, PTSD, depression, and both alcohol and substance use [ 90 , 91 ]. In keeping with studies into the mechanistic actions of psilocybin, many participants rated their experience with mescaline as one of the most spiritually significant and meaningful experiences of their lives [ 91 ]. In addition, improvements in symptoms of anxiety, PTSD, depression, and both alcohol and other substance use were associated with greater “intensity of insight”, again demonstrating that some aspect of the subjective effect of the psychedelic experience is linked to clinical outcome. While clinical research with mescaline is still in its infancy, the data thus far suggest that mescaline may hold similar promise to other phenethylamines for the treatment of multiple mental health disorders.
Salvinorin A
Salvia divinorum is a sage species that is used ritualistically among the Mazatec tribe of Mexico. The active constituent, salvinorin A, is a kappa opioid agonist that has no discernable action at the 5HT 2A receptor, giving pause to the assertion that all psychedelics act primarily through 5HT 2A receptor activation. As a kappa agonist, salvinorin A may also hold clinical potential as a treatment for pain, ischemia, cardiac damage, and addiction [ 92 ], perhaps especially in biological females who do not find kappa agonists particularly aversive [ 93 ]. While there is still a paucity of human research on salvinorin A, recent findings indicate that when smoked, salvinorin A produces intense but short acting hallucinations and out of body experiences but, notably, no significant changes in heart rate or blood pressure [ 94 ]. In keeping with the classic psychedelics, administration of salvinorin A has also been shown to reduced brain wide dynamic functional connectivity (most notably in the default mode network), while increasing between-network static functional connectivity [ 95 ]. Unlike ibogaine, which also activates kappa opioid receptors and demonstrates anti-addictive properties, salvinorin A has not, to date, been shown to induce the notable adverse effects that have curtailed ibogaine’s development as a clinical therapeutic, and emergent events are rare ( https://calpoison.org/news/salvia-divinorum ). Because of its potential safety and novel pharmacological mechanism of action, further effort should be made to evaluate the pharmacological potential of salvinorin A.
Dissociative agents (Cyclohexanones)
Ketamine is a selective NMDA antagonist that has long been used as an anesthetic and animal tranquilizer, and which has recently found new use as a fast-acting—albeit temporary—treatment for depression [ 96 ]. While ketamine is best considered an atypical psychedelic, or perhaps a drug with psychedelic-like effects, the mechanism of action of ketamine (NMDA antagonism) is a contributor to the effects of several classic psychedelics (such as ibogaine and DMT) and may prove relevant to the further development of psychedelics as therapeutics. It is therefore worth briefly mentioning the state of current research with ketamine.
In addition to its use as an antidepressant, ketamine might hold promise for the treatment of anxiety and PTSD. A recent review indicates that, under certain circumstances (e.g., specified dose and route of administration), ketamine is effective in temporarily attenuating some anxiety disorders [ 97 ] and may therefore merit further investigation. With respect to PTSD symptomology, although a randomized, double-blind active-placebo-controlled trial demonstrated that 2 weeks of 3× weekly ketamine infusions are efficacious for up to a month in those with severe PTSD [ 98 ], a larger trial found no significant effect of 4 weeks of 2× weekly ketamine infusions in a population of military Veterans and service members with comorbid depression and PTSD [ 99 ]. Furthermore, recent years have seen the publishing of promising data on the use of ketamine as a rapid-acting therapy for substance use disorders and other neuropsychiatric conditions like obsessive-compulsive disorder [ 100 ]. As with previous depression trials, even if initially efficacious under certain dosing regimens, the limited durability of positive clinical outcomes of ketamine complicates drug administration and adoption as a frontline therapeutic [ 101 ] for a number of conditions. It is possible that, as with MDMA and psilocybin, durability of ketamine’s effects on mental health indications could be potentiated with the addition of psychotherapy and, to this end, a recent study has found that an automated, computerized training protocol might extend the effects of ketamine on depression [ 102 ]. Additional data are needed to determine whether and how the coupling of ketamine administration with psychotherapy [ 103 ] renders the drug more efficacious and durable for different indications.
Set and setting are key variables
Set and setting have long been recognized as fundamental elements driving the clinical outcomes of psychedelic administration [ 104 ], but more research is needed to operationalize and investigate how best to incorporate these factors into treatment protocols. Set is typically defined as the mindset, psychosocial education, and experience that a participant brings with them as they enter treatment, and setting is defined as the environment in which the psychedelic compound is administered. The dependence of the clinical and psychological effects of psychedelics on the mindset and environment of the user suggests that they truly are “experiential medicines”. Increasingly, human studies with psychedelics are attempting to systematically modify set and setting, either to study set and setting as independent variables affecting the outcomes of the study (NCT04410913), or by making them a fixed key part of the study design, such as electing to use group psychotherapy and/or drug administration instead of individual sessions [ 105 , 106 ]. Group treatment processes likely result in qualitatively different therapeutic environments that differ from individual treatments in ways beyond economics and scalability. The long history of the group use of psychedelic substances in Indigenous and other traditional settings across North and South America suggests that, with the proper context and training, it is possible for group psychedelic experiences to be safely managed and to result in positive outcomes for the participants [ 107 , 108 ]. Nevertheless, most of the clinical data to date have been generated using a fairly homogenous clinical approach, and so specific experiments should be conducted with more variation in set and setting to determine how best to potentiate the therapeutic value of these variables, while mitigating possible harm when administering psychedelics as medical therapies.
Optimizing set while maintaining blinding
One concern that is repeatedly raised in the discussion of psychedelic trials is the conundrum around experimental blinding [ 109 ]. The prevailing belief is that psychedelic trials are difficult to blind and therefore one must always worry that expectation is coloring outcome. This is especially true when participants enroll in a trial that not only takes up weeks of their life, but also assesses whether the investigational compound occasions a particularly meaningful, and often spiritual, life experience. While maintaining a double-blind is indeed a common challenge in psychedelic trials, several methods can be utilized to minimize the impact of expectation and ensure that clinical outcome measures reflect the long-term and durable effects of psychedelic therapies. For example, the use of an active control drug and/or a psychedelic naïve subject population may make it more difficult for even a well-informed participant to be confident of their treatment assignment. In addition, the use of a centralized assessment core to evaluate outcome measures ensures that data collection is blinded and homogeneously collected across study sites while also mitigating the risk of participants inflating their improvements to please study staff with whom they have developed a therapeutic alliance. Perhaps most importantly, the collection of long-term follow-up data from study participants can partially address concerns regarding expectation effects and can speak to the potential durability of psychedelic-induced change. While it is reasonable to suggest that a participant in the throes of a clinical trial might inadvertently exaggerate their improvements when surrounded with engaged and supportive staff, it is less reasonable to assume that this effect would last months after the trial has ended and the participant is again immersed in their regular environment.
Limitations and future directions for psychedelic therapies
The recent explosion in interest in psychedelic therapies has been based on multiple preliminary reports suggesting the potential of safety and efficacy in various psychiatric and general medical conditions, especially mood disorders, alcohol use disorder, and PTSD. These data, however, are not without their limitations. As clinically effective as psychedelics can be when administered under the right conditions, it would be negligent to forego mention of the study participants who do not respond discernably to psychedelic agents. For example, while the recent phase 3 trial of MDMA therapy for PTSD showed that 67% of participants gain complete remission from PTSD, and another 21% exhibited a clinically meaningful response, this still left 12% of study participants with no clinically meaningful response. Similarly, a recent phase 2 trial of psilocybin therapy for an episode of treatment-resistant depression showed that, while 37% of participants displayed a clinically meaningful response to psilocybin at the primary endpoint (week 3), most did not [ 56 ]. While some of this can perhaps be chalked up to the impact of set and setting, some of it is undoubtedly due to differences in sensitivity to psychedelic compounds, and perhaps also to differences in the response to the uncertainty and change brought about by these therapies. In addition, genetics play a role not only in pharmacokinetics but also in suggestibility and the development and maintenance of emotional memories [ 110 ] and may therefore also impact the effects of psychedelic therapies. One would hope that, as precision medicine advances, and as adaptive trials and genetic testing enable us to better tailor treatments to individual patients, biological and behavioral factors will be used to ensure that the potential therapeutic impact of psychedelic therapies is maximized.
Psychedelics are powerful compounds that are capable of enabling great change. As such, they should be approached with care and caution. Under the best of circumstances, and when properly facilitated, psychedelic therapy can kindle the release of some of the most deeply entrenched negative affective states and thought processes, resulting in clinical recovery and positive growth. However, the experiential flipside is equally relevant: occasionally, and especially when taken under suboptimal conditions, without adequate support, or at too high a dose, psychedelics can trigger dysphoria, disorganize thought, and spark delusional perceptions [ 111 , 112 , 113 , 114 ]. In addition, given the largely explanatory trials dataset available to date, it remains to be seen how clinical outcomes will be shaped by different real-world factors such as personality disorders, significant psychiatric and medical comorbidities, and the combination of psychedelics with different behavioral therapies or even with other psychedelics (e.g., psilocybin plus MDMA). We must therefore move forward with care and forethought. These compounds may potently manifest aspects of the human psyche in a manner that can both help and harm. As such, scientific investigations into the judicious use of psychedelics test our capacity for, and professional commitment to, the proper uses of clinical power in the service of healing. It is time that psychedelic therapies be carefully reconsidered [ 115 ].
Therapeutic Goods Administration (Australian Government). 2023. Change to classification of psilocybin and MDMA to enable prescribing by authorised psychiatrists. https://www.tga.gov.au/news/media-releases/change-classification-psilocybin-and-mdma-enable-prescribing-authorised-psychiatrists Accessed 4 June 2023.
Health Canada. Notice to stakeholders: Requests to the Special Access Program (SAP) involving psychedelic-assisted psychotherapy. 2023. https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/announcements/requests-special-access-program-psychedelic-assisted-psychotherapy.html Accessed 4 June 2023.
Delay P, Lemperiere Q. Effet therapeutique de la psilocybine sur une nevrose convulsive. Annales Medico-Psychologiques: Revue Psychiatrique. Masson & CLE, editors. Paris: Libraires De L'Academie de Medicine; 1959. p. 509–15.
Mangini M. Treatment of alcoholism using psychedelic drugs: a review of the program of research. J Psychoact Drugs. 1998;30(Dec):381–418.
Article CAS Google Scholar
Rucker JJ, Iliff J, Nutt DJ. Psychiatry & the psychedelic drugs. Past, present & future. Neuropharmacology 2018;142:200–18.
Article CAS PubMed Google Scholar
O’Brien CP, Jones RT. Methodological issues in the evaluation of a medication for its potential benefits in enhancing psychotherapy. Fifty Years of LSD: Current Status and Perspectives of Hallucinogens, New York, Parthenon. 1994:213–21.
Nutt DJ, King LA, Nichols DE. Effects of Schedule I drug laws on neuroscience research and treatment innovation. Nat Rev Neurosci. 2013;14:577–85.
Barrett FS, Doss MK, Sepeda ND, Pekar JJ, Griffiths RR. Emotions and brain function are altered up to one month after a single high dose of psilocybin. Sci Rep. 2020;10:1–4.
Article Google Scholar
Ho JT, Preller KH, Lenggenhager B. Neuropharmacological modulation of the aberrant bodily self through psychedelics. Neurosci Biobehav Rev. 2020;108:526–41.
Article PubMed Google Scholar
Reiff CM, Richman EE, Nemeroff CB, Carpenter LL, Widge AS, Rodriguez CI, et al. Work Group on Biomarkers and Novel Treatments, a Division of the American Psychiatric Association Council of Research. Psychedelics and psychedelic-assisted psychotherapy. Am J Psychiatry. 2020;177:391–410.
Johnson MW, Richards WA, Griffiths RR. Human hallucinogen research: guidelines for safety. J Psychopharmacol. 2008;22:603–20.
Article CAS PubMed PubMed Central Google Scholar
Horton DM, Morrison B, Schmidt J. Systematized review of psychotherapeutic components of psilocybin-assisted psychotherapy. Am J Psychother. 2021;74:140–9.
David E. Nichols, Charles D. Nichols, and Peter S. Hendricks.Proposed Consensus Statement on Defining Psychedelic Drugs.Psychedelic Medicine.Mar 2023.12–13. https://doi.org/10.1089/psymed.2022.0008 .
Krupitsky EM, Grinenko AY. Ketamine psychedelic therapy (KPT): a review of the results of ten years of research. J Psychoact Drugs. 1997;29:165–83.
Villoldo A. An introduction to the psychodelic psychotherapy of Salvador. Roquet J Humanist Psychol 1997;17:45–58.
Google Scholar
Naranjo C, Shulgin AT, Sargent T. Evaluation of 3, 4-methylenedioxyamphetamine (MDA) as an adjunct to psychotherapy. Pharmacology 1978;17:359–64.
Haijen ECHM, Kaelen M, Roseman L, Timmermann C, Kettner H, Russ S, et al. Predicting Responses to Psychedelics: A Prospective Study. Front Pharm. 2018;9:897.
Studerus E, Gamma A, Kometer M, Vollenweider FX. Prediction of psilocybin response in healthy volunteers. PloS ONE. 2012;7:e30800.
Studerus E, Vizeli P, Harder S, Ley L, Liechti ME. Prediction of MDMA response in healthy humans: a pooled analysis of placebo-controlled studies. J Psychopharmacol. 2021;35:556–65.
Goutarel R, Gollnhofer O, Sillans R. Pharmacodynamics and therapeutic applications of iboga and ibogaine. Psychedelic Monogr Essays 1993;6:71–111.
Maillet EL, Milon N, Heghinian MD, Fishback J, Schürer SC, Garamszegi N, et al. Noribogaine is a G-protein biased κ-opioid receptor agonist. Neuropharmacology 2015;99:675–88.
Mash DC, Kovera CA, Buck BE, Norenberg MD, Shapshak P, Hearn WL, et al. Medication Development of Ibogaine as a Pharmacotherapy for Drug Dependence. Ann N. Y Acad Sci. 1998;844:274–92. https://doi.org/10.1111/j.1749-6632.1998.tb08242.x .
Mash DC, Kovera CA, Pablo J, Tyndale RF, Ervin FD, Williams IC, et al. Ibogaine: complex pharmacokinetics, concerns for safety, and preliminary efficacy measures. Ann N Y Acad Sci. 2000;914:394–401.
Schenberg EE, de Castro Comis MA, Chaves BR, da Silveira DX. Treating drug dependence with the aid of ibogaine: A retrospective study. J Psychopharmacol. 2014;28:993–1000.
Litjens RP, Brunt TM. How toxic is ibogaine? Clin Toxicol (Philos). 2016;54:297–302. https://doi.org/10.3109/15563650.2016.1138226 .
Köck P, Froelich K, Walter M, Lang U, Dürsteler KM J Subst Abuse Treat. 2022 A systematic literature review of clinical trials and therapeutic applications of ibogaine. Jul;138:108717.
Ona G, Rocha JM, Bouso JC, Hallak JEC, Borràs T, Colomina MT, et al. The adverse events of ibogaine in humans: an updated systematic review of the literature (2015–2020). Psychopharmacology (Berl). 2022;239:1977–87. https://doi.org/10.1007/s00213-021-05964-y .
KR Alper, Stajić M, JR Gill. Fatalities Temporally Associated with the Ingestion of Ibogaine. 2012;57:398–412.
Patrick M, Could an illegal psychedelic substance ease the opioid crisis? Daniel Cameron wants to find out. News from the States. 2023. https://www.newsfromthestates.com/article/could-illegal-psychedelic-substance-ease-opioid-crisis-daniel-cameron-wants-find-out Accessed, 4 June, 2023.
Knuijver T, Schellekens A, Belgers M, Donders R, van Oosteren T, Kramers K, et al. Safety of ibogaine administration in detoxification of opioid-dependent individuals: a descriptive open-label observational study. Addiction. 2022;117:118–28. https://doi.org/10.1111/add.15448 .
Rickli A, Moning OD, Hoener MC, Liechti ME. Receptor interaction profiles of novel psychoactive tryptamines compared with classic hallucinogens. Eur Neuropsychopharmacol. 2016;26:1327–37.
Watts VJ, Lawler CP, Rox DR, Neve KA, Nichols DE, Mailman RB. LSD and structural analogs: pharmacological evaluation at D 1 dopamine receptors. Psychopharmacology 1995;118:401–9.
Marona-Lewicka D, Chemel BR, Nichols DE. Dopamine D4 receptor involvement in the discriminative stimulus effects in rats of LSD, but not the phenethylamine hallucinogen DOI. Psychopharmacol (Berl). 2009;203:265–77.
Dyck E. ‘Hitting highs at rock bottom’: LSD treatment for alcoholism, 1950–1970. Soc Hist Med. 2006;19:313–29.
Krebs TS, Johansen PØ. Lysergic acid diethylamide (LSD) for alcoholism: meta-analysis of randomized controlled trials. J Psychopharmacol. 2012;26:994–1002.
B Liester M. A review of lysergic acid diethylamide (LSD) in the treatment of addictions: historical perspectives and future prospects. Curr Drug Abus Rev. 2014;7:146–56.
Leonard HL, Rapoport JL. Relief of obsessive-compulsive symptoms by LSD and psilocin. Am J Psychiatry. 1987.
Gasser P, Kirchner K, Passie T. LSD-assisted psychotherapy for anxiety associated with a life-threatening disease: a qualitative study of acute and sustained subjective effects. J Psychopharmacol. 2015;29:57–68. https://doi.org/10.1177/0269881114555249 .
Sewell RA, Halpern JH, Pope HG Jr. Response of cluster headache to psilocybin and LSD. Neurology 2006;66:1920–2. https://doi.org/10.1212/01.wnl.0000219761.05466.43 .
Haijen EC, Hurks PP, Kuypers KP. Microdosing with psychedelics to self-medicate for ADHD symptoms in adults: A prospective naturalistic study. Neurosci Appl. 2022;1:101012.
Gasser P. Psycholytic Therapy with MDMA and LSD in Switzerland. Newsletter of the Multidisciplinary Association for Psychedelic Studies MAPS - Volume 5 Number 3 Winter 1994–95 - p. 3–7.
Pahnke WN, Kurland AA, Unger S, Savage C, Grof S. The experimental use of psychedelic (LSD) psychotherapy. JAMA. 1970;212:1856–63.
Gasser P, Holstein D, Michel Y, Doblin R, Yazar-Klosinski B, Passie T, et al. Safety and efficacy of lysergic acid diethylamide-assisted psychotherapy for anxiety associated with life-threatening diseases. Nerv Ment Dis. 2014;202:513–20.
Schindler EA, Gottschalk CH, Weil MJ, Shapiro RE, Wright DA, Sewell RA. Indoleamine Hallucinogens in Cluster Headache: Results of the Clusterbusters Medication Use Survey. J Psychoact Drugs. 2015;47:372–81. https://doi.org/10.1080/02791072.2015.1107664 .
Family N, Maillet EL, Williams LT, Krediet E, Carhart-Harris RL, Williams TM, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of low dose lysergic acid diethylamide (LSD) in healthy older volunteers. Psychopharmacology 2020;237:841–53.
Passie T, Seifert J, Schneider U, Emrich HM. The pharmacology of psilocybin. Addict Biol. 2002;7:357–64. https://doi.org/10.1080/1355621021000005937 .
Moreno JL, Holloway T, Albizu L, Sealfon SC, González-Maeso J. Metabotropic glutamate mGlu2 receptor is necessary for the pharmacological and behavioral effects induced by hallucinogenic 5-HT2A receptor agonists. Neurosci Lett. 2011;493:76–9.
Davis AK, Barrett FS, Griffiths RR. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J Contextual Behav Sci. 2020;15:39–45.
Carhart-Harris RL, Bolstridge M, Rucker J, Day CM, Erritzoe D, Kaelen M, et al. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. 2016;3:619–27.
Bogenschutz MP, Ross S, Bhatt S, Baron T, Forcehimes AA, Laska E, et al. Percentage of Heavy Drinking Days Following Psilocybin-Assisted Psychotherapy vs Placebo in the Treatment of Adult Patients With Alcohol Use Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2022;79:953–62. https://doi.org/10.1001/jamapsychiatry.2022.2096 .
Article PubMed PubMed Central Google Scholar
Johnson MW, Garcia-Romeu A, Cosimano MP, Griffiths RR. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J Psychopharmacol. 2014;28:983–92.
Moreno FA, Wiegand CB, Taitano EK, Delgado PL. Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J Clin Psychiatry. 2006;67:1735–40.
Anderson BT, Danforth A, Daroff PR, Stauffer C, Ekman E, Agin-Liebes G, et al. Psilocybin-assisted group therapy for demoralized older long-term AIDS survivor men: An open-label safety and feasibility pilot study. EClinicalMedicine. 2020;27:100538 https://doi.org/10.1016/j.eclinm.2020.100538 .
Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abus. 2017;43:55–60.
James E, Robertshaw TL, Hoskins M, Sessa B. Psilocybin occasioned mystical-type experiences. Hum Psychopharmacol Clin Exp. 2020;35:e2742.
Goodwin GM, Aaronson ST, Alvarez O, Arden PC, Baker A, Bennett JC, et al. Single-Dose Psilocybin for a Treatment-Resistant Episode of Major Depression. N Engl J Med 2022;387:1637–48. https://doi.org/10.1056/NEJMoa2206443 .
Davis AK, Barrett FS, May DG, Cosimano MP, Sepeda ND, Johnson MW, et al. Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78:481–9. https://doi.org/10.1001/jamapsychiatry.2020.3285 .
Gukasyan N, Davis AK, Barrett FS, Cosimano MP, Sepeda ND, Johnson MW, et al. Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: Prospective 12-month follow-up. J Psychopharmacol. 2022;36:151–8.
Labate BC, Cavnar C, editors. Ayahuasca shamanism in the Amazon and beyond. Oxford Ritual Studies; 2014.
Dos Santos RG, Hallak JEC. Therapeutic use of serotoninergic hallucinogens: A review of the evidence and of the biological and psychological mechanisms. Neurosci Biobehav Rev. 2020;108:423–34. https://doi.org/10.1016/j.neubiorev.2019.12.001 .
González D, Cantillo J, Pérez I, Farré M, Feilding A, Obiols JE, et al. Therapeutic potential of ayahuasca in grief: a prospective, observational study. Psychopharmacology 2020;237:1171–82.
Lafrance A, Loizaga-Velder A, Fletcher J, Renelli M, Files N, Tupper KW. Nourishing the Spirit: Exploratory Research on Ayahuasca Experiences along the Continuum of Recovery from Eating Disorders. J Psychoact Drugs. 2017;49:427–35. https://doi.org/10.1080/02791072.2017.1361559 .
Fábregas JM, González D, Fondevila S, Cutchet M, Fernández X, Barbosa PCR, et al. "Assessment of addiction severity among ritual users of ayahuasca". Drug Alcohol Depend. 2010;111:257–61.
Harris R, Gurel L. "A Study of Ayahuasca Use in North America". J Psychoact Drugs. 2012;44:209–15.
Barbosa PC, Strassman RJ, Da Silveira DX, Areco K, Hoy R, Pommy J, et al. Psychological and neuropsychological assessment of regular hoasca users. Compr Psychiatry. 2016;71:95–105.
Sarris J, Perkins D, Cribb L, Schubert V, Opaleye E, Bouso JC, et al. Ayahuasca use and reported effects on depression and anxiety symptoms: An international cross-sectional study of 11,912 consumers. J Affect Disord Rep. 2021;4:100098.
Durante Í, Dos Santos RG, Bouso JC, Hallak JE. Risk assessment of ayahuasca use in a religious context: self-reported risk factors and adverse effects. Braz J Psychiatry. 2020;43:362–9.
Article PubMed Central Google Scholar
Palhano-Fontes F, Barreto D, Onias H, Andrade KC, Novaes MM, Pessoa JA, et al. "Rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression: a randomized placebo-controlled trial". Psychological Med. 2018;49:655–63.
Bunzow JR, Sonders MS, Arttamangkul S, Harrison LM, Zhang G, Quigley DI, et al. Amphetamine, 3,4-methylenedioxymethamphetamine, lysergic acid diethylamide, and metabolites of the catecholamine neurotransmitters are agonists of a rat trace amine receptor. Mol Pharm. 2001;60:1181–8. https://doi.org/10.1124/mol.60.6.1181 .
Fontanilla D, Johannessen M, Hajipour AR, Cozzi NV, Jackson MB, Ruoho AE. The hallucinogen N,N-dimethyltryptamine (DMT) is an endogenous sigma-1 receptor regulator. Science. 2009;323:934–7. https://doi.org/10.1126/science.1166127 .
Carbonaro TM, Eshleman AJ, Forster MJ, Cheng K, Rice KC, Gatch MB. The role of 5-HT2A, 5-HT 2C and mGlu2 receptors in the behavioral effects of tryptamine hallucinogens N,N-dimethyltryptamine and N,N-diisopropyltryptamine in rats and mice. Psychopharmacol (Berl). 2015;232:275–84. https://doi.org/10.1007/s00213-014-3658-3 .
Strassman RJ, Qualls CR. Dose-response study of N,N-dimethyltryptamine in humans. I. Neuroendocrine, autonomic, and cardiovascular effects. Arch Gen Psychiatry. 1994;51:85–97. https://doi.org/10.1001/archpsyc.1994.03950020009001 .
Adamson S, (Ed). Through the gateway of the heart: Accounts of experiences with MDMA and other empathogenic substances. San Francisco: Four Trees Publications; 1985.
Greer G, Tolbert R. Subjective reports of the effects of MDMA in a clinical setting. J Psychoact Drugs. 1986;18:319–27. https://doi.org/10.1080/02791072.1986.10472364 . PMID: 2880946
Shulgin AT, Shulgin A. PiHKAL: A Chemical Love Story, Transform Press; 1991.
Verrico CD, Miller GM, Madras BK. MDMA (Ecstasy) and human dopamine, norepinephrine, and serotonin transporters: implications for MDMA-induced neurotoxicity and treatment. Psychopharmacology (Berl). 2007;189:489–503. https://doi.org/10.1007/s00213-005-0174-5 .
Nichols DE, Lloyd DH, Hoffman AJ, Nichols MB, Yim G. Effects of certain hallucinogenic amphetamine analogs on the release of [3H]-serotonin from rat brain synaptosomes. J Med Chem. 1982;25:530–5.
Rudnick G, Wall SC. The molecular mechanism of “ecstasy” [3, 4-methylenedioxy-methamphetamine (MDMA)]: serotonin transporters are targets for MDMA-induced serotonin release. Proc Natl Acad Sci. 1992;89:1817–21.
Kirkpatrick MG, Francis SM, Lee R, de Wit H, Jacob S. Plasma oxytocin concentrations following MDMA or intranasal oxytocin in humans. Psychoneuroendocrinology. 2014;46:23–31. https://doi.org/10.1016/j.psyneuen.2014.04.006 .
Bos PA, Panksepp J, Bluthé RM, van Honk J. Acute effects of steroid hormones and neuropeptides on human social-emotional behavior: a review of single administration studies. Front Neuroendocrinol. 2012;33:17–35. https://doi.org/10.1016/j.yfrne.2011.01.002 .
Bedi G, Phan KL, Angstadt M, de Wit H. Effects of MDMA on sociability and neural response to social threat and social reward. Psychopharmacol (Berl). 2009;207:73–83. https://doi.org/10.1007/s00213-009-1635-z .
Singleton SP, Wang JB, Mithoefer M, Hanlon C, George MS, Mithoefer A, et al. Altered brain activity and functional connectivity after MDMA-assisted therapy for post-traumatic stress disorder. Front Psychiatry. 2023;13:947622 https://doi.org/10.3389/fpsyt.2022.947622 .
Mitchell JM, Bogenschutz M, Lilienstein A, Harrison C, Kleiman S, Parker-Guilbert K, et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med. 2021;27:1025–33. https://doi.org/10.1038/s41591-021-01336-3 .
Smith KW, Sicignano DJ, Hernandez AV, White CM. MDMA-Assisted Psychotherapy for Treatment of Posttraumatic Stress Disorder: A Systematic Review with Meta-Analysis. J Clin Pharm. 2022;62:463–71. https://doi.org/10.1002/jcph.1995 .
Danforth AL, Grob CS, Struble C, Feduccia AA, Walker N, Jerome L, et al. Reduction in social anxiety after MDMA-assisted psychotherapy with autistic adults: a randomized, double-blind, placebo-controlled pilot study. Psychopharmacol (Berl). 2018;235:3137–48. https://doi.org/10.1007/s00213-018-5010-9 .
Kamboj SK, Kilford EJ, Minchin S, Moss A, Lawn W, Das RK, et al. Recreational 3,4-methylenedioxy-N-methylamphetamine (MDMA) or 'ecstasy' and self-focused compassion: Preliminary steps in the development of a therapeutic psychopharmacology of contemplative practices. J Psychopharmacol. 2015;29:961–70. https://doi.org/10.1177/0269881115587143 .
El-Seedi HR, De Smet PA, Beck O, Possnert G, Bruhn JG. "Prehistoric peyote use: alkaloid analysis and radiocarbon dating of archaeological specimens of Lophophora from Texas". J Ethnopharmacol. 2005;101:238–42.
Albaugh BJ, Anderson PO. Peyote in the treatment of alcoholism among American Indians. Am J Psychiatry. 1974;131:1247–50. https://doi.org/10.1176/ajp.131.11.1247 .
Blum K, Futterman SL, Pascarosa P. Peyote, a potential ethnopharmacologic agent for alcoholism and other drug dependencies: possible biochemical rationale. Clin Toxicol. 1977;11:459–72. https://doi.org/10.3109/15563657708988210 .
Garcia-Romeu A, Davis AK, Erowid F, Erowid E, Griffiths RR, Johnson MW. Cessation and reduction in alcohol consumption and misuse after psychedelic use. J Psychopharmacol. 2019;33:1088–101. https://doi.org/10.1177/0269881119845793 .
Agin-Liebes G, Haas TF, Lancelotta R, Uthaug MV, Ramaekers JG, Davis AK. Naturalistic Use of Mescaline Is Associated with Self-Reported Psychiatric Improvements and Enduring Positive Life Changes. ACS Pharm Transl Sci. 2021;4:543–52. https://doi.org/10.1021/acsptsci.1c00018 .
Beck TC, Hapstack MA, Beck KR, Dix TA. Therapeutic potential of kappa opioid agonists. Pharmaceuticals 2019;12:95.
Rasakham K, Liu-Chen LY. Sex differences in kappa opioid pharmacology. Life Sci 2011;88:2–16. https://doi.org/10.1016/j.lfs.2010.10.007 .
Johnson MW, Griffiths RR. P. 1. c. 057 Human psychopharmacology of the kappa opioid agonist salvinorin A. Eur Neuropsychopharmacol. 2010;20:S267–8.
Doss MK, May DG, Johnson MW, Clifton JM, Hedrick SL, Prisinzano TE, et al. The Acute Effects of the Atypical Dissociative Hallucinogen Salvinorin A on Functional Connectivity in the Human Brain. Sci Rep. 2020;10:16392 https://doi.org/10.1038/s41598-020-73216-8 .
Corriger A, Pickering G. Ketamine and depression: a narrative review. Drug Des Devel Ther. 2019;13:3051–67. https://doi.org/10.2147/DDDT.S221437 .
Tully JL, Dahlén AD, Haggarty CJ, Schiöth HB, Brooks S. Ketamine treatment for refractory anxiety: A systematic review. Br J Clin Pharm. 2022;88:4412–26. https://doi.org/10.1111/bcp.15374 .
Feder A, Costi S, Rutter SB, Collins AB, Govindarajulu U, Jha MK, et al. A Randomized Controlled Trial of Repeated Ketamine Administration for Chronic Posttraumatic Stress Disorder. Am J Psychiatry. 2021;178:193–202. https://doi.org/10.1176/appi.ajp.2020.20050596 .
Abdallah CG, Roache JD, Gueorguieva R, Averill LA, Young-McCaughan S, Shiroma PR, et al. Dose-related effects of ketamine for antidepressant-resistant symptoms of posttraumatic stress disorder in veterans and active duty military: a double-blind, randomized, placebo-controlled multi-center clinical trial. Neuropsychopharmacology. 2022;47:1574–81. https://doi.org/10.1038/s41386-022-01266-9 .
Walsh Z, Mollaahmetoglu OM, Rootman J, Golsof S, Keeler J, Marsh B, et al. Ketamine for the treatment of mental health and substance use disorders: comprehensive systematic review. BJPsych Open. 2022;8:e19.
Rodriguez CI, Kegeles LS, Levinson A, Feng T, Marcus SM, Vermes D, et al. Randomized controlled crossover trial of ketamine in obsessive-compulsive disorder: proof-of-concept. Neuropsychopharmacology. 2013;38:2475–83. https://doi.org/10.1038/npp.2013.150 .
Price RB, Spotts C, Panny B, Griffo A, Degutis M, Cruz N, et al. A novel, brief, fully automated intervention to extend the antidepressant effect of a single ketamine infusion: a randomized clinical trial. Am J Psychiatry. 2022;179:959–68.
Drozdz SJ, Goel A, McGarr MW, Katz J, Ritvo P, Mattina GF, et al. Ketamine assisted psychotherapy: A systematic narrative review of the literature. J Pain Res. 2022:1691–706.
Leary T, Litwin GH, Metzner R. Reactions to psilocybin administered in a supportive environment. J Nerv Ment Dis. 1963;137:561–73. https://doi.org/10.1097/00005053-196312000-00007 .
Agrawal M, Emanuel E, Richards B, Richards W, Roddy K, Thambi P. Assessment of Psilocybin Therapy for Patients with Cancer and Major Depression Disorder. JAMA Oncol. 2023. https://doi.org/10.1001/jamaoncol.2023.0351 .
Gasser P. Psychedelic group therapy. In Disruptive Psychopharmacology. Cham: Springer International Publishing; 2022. p 23–34.
Bouso JC, González D, Fondevila S, Cutchet M, Fernández X, Ribeiro Barbosa PC, et al. Personality, psychopathology, life attitudes and neuropsychological performance among ritual users of ayahuasca: a longitudinal study. PLoS ONE. 2012. https://doi.org/10.1371/journal.pone.0042421 .
Csordas TJ. The Navajo healing project. Med Anthropol Q. 2000;14:463–75.
Muthukumaraswamy SD, Forsyth A, Lumley T. Blinding and expectancy confounds in psychedelic randomized controlled trials. Expert Rev Clin Pharmacol. 2021;14:1133–52.
Norrholm SD, Ressler KJ. Genetics of anxiety and trauma-related disorders. Neuroscience. 2009;164:272–87. https://doi.org/10.1016/j.neuroscience.2009.06.036 .
Strassman RJ. Adverse reactions to psychedelic drugs. A review of the literature. J Nerv Ment Dis. 1984;172:577–95.
Freedman DX. "On the Use and Abuse of LSD.". Arch Gen Psychiatry. 1968;18:330–47.
Carbonaro TM, Bradstreet MP, Barrett FS, MacLean KA, Jesse R, Johnson MW, et al. Survey study of challenging experiences after ingesting psilocybin mushrooms: Acute and enduring positive and negative consequences. J Psychopharmacol. 2016;30:1268–78.
Bender D, Hellerstein DJ. Assessing the risk–benefit profile of classical psychedelics: A clinical review of second-wave psychedelic research. Psychopharmacology. 2022:1–26.
Grinspoon L, Bakalar J. Psychedelic drugs reconsidered. New York: Basic Books; 1979.
Download references
Author information
Authors and affiliations.
Department of Neurology, University of California San Francisco, San Francisco, CA, USA
Jennifer M. Mitchell
Department of Psychiatry and Behavioral Sciences, University of California San Francisco, San Francisco, CA, USA
Jennifer M. Mitchell & Brian T. Anderson
Department of Veterans Affairs, Research Service, San Francisco VA Medical Center, San Francisco, CA, USA
Berkeley Center for the Science of Psychedelics, University of California Berkeley, Berkeley, CA, USA
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributed equally to the writing of this paper.

Corresponding author
Correspondence to Jennifer M. Mitchell .
Ethics declarations
Competing interests.
In the last 3 years, BA has received consulting fees from Journey Colab and JM has received grant support from the Multidisciplinary Association for Psychedelic Studies.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mitchell, J.M., Anderson, B.T. Psychedelic therapies reconsidered: compounds, clinical indications, and cautious optimism. Neuropsychopharmacol. 49 , 96–103 (2024). https://doi.org/10.1038/s41386-023-01656-7
Download citation
Received : 17 April 2023
Revised : 05 June 2023
Accepted : 06 July 2023
Published : 21 July 2023
Issue Date : January 2024
DOI : https://doi.org/10.1038/s41386-023-01656-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
A rapid narrative review of the clinical evolution of psychedelic treatment in clinical trials.
- Ronit Kishon
- Nadav Liam Modlin
- James Rucker
npj Mental Health Research (2024)
Psychedelic experiences and long-term spiritual growth: a systematic review
- William A. Schutt
- Julie J. Exline
- Joshua A. Wilt
Current Psychology (2024)
Current Understanding of Compulsive Sexual Behavior Disorder and Co-occurring Conditions: What Clinicians Should Know about Pharmacological Options
- Gemma Mestre-Bach
- Marc N. Potenza
CNS Drugs (2024)
The effects of Lysergic Acid Diethylamide (LSD) on the Positive Valence Systems: A Research Domain Criteria (RDoC)-Informed Systematic Review
- Niloufar Pouyan
- Farnaz Younesi Sisi
- Jonathan D. Morrow
CNS Drugs (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
The independent source for health policy research, polling, and news.
Exploring the Rise in Mental Health Care Use by Demographics and Insurance Status
Nirmita Panchal and Justin Lo Published: Aug 01, 2024
Many people in the United States experience mental health conditions, which raises questions about mental health service utilization patterns and what barriers exist with connecting people to services. Prior research suggests that mental health service utilization increased over time. This analysis explores more recent data, from 2019 to 2022, to understand the latest trends in utilization of mental health services and how it differs by demographics and insured status. In this analysis, receipt of mental health care is measured as the share of people who say they received mental health counseling and/or prescription medication for mental health concerns in the last year. Estimates shown are KFF analyses of National Health Interview Survey (NHIS) data among adults in the U.S. from 2019 to 2022.
In 2022, 23% of adults received mental health treatment, up from 19% in 2019 (Figure 1). Specifically, the share of adults saying they received mental health counseling in the past year increased from 10% in 2019 to 13% in 2022. Similarly, the share of adults reporting they took prescription medication for mental health conditions increased from 16% to 19% during the same period. Receipt of prescription medication remained consistently higher than counseling (19% vs. 13%, respectively, in 2022).
Compared to older adults, young adults (ages 18-26) were more likely to receive mental health treatment and experienced the highest increase in receipt of treatment over time. In 2022, 26% of young adults reported receiving counseling and/or prescription medications for mental health conditions in the past year, representing a significantly higher share compared to all other adults (ages 27 and above) (Figure 2).
Young adults also experienced the largest percent increase in the share of adults receiving mental health treatment from 2019 to 2022 (45%), followed by adults ages 27-50 (29%), 51-64 (13%), and 65 and above (1%) (Figure 2). Although receipt of mental health services has increased among young adults in recent years, other KFF analyses found that leading up to the pandemic, many young adults with mental health conditions did not receive treatment. The lack of treatment among this population may be linked to costs , transitioning from pediatric to adult health care , and difficulties accessing mental health services in college settings .
Women are nearly twice as likely to report receiving mental health treatment in the past year compared to men. In 2022, 29% of women reported receiving mental health services, compared to 17% of men (Figure 3). Research suggests men may be less likely to seek mental health care than women. Men are also more likely to be uninsured and less likely to report a usual source of health care. Separately, women are more likely than men to report experiencing mental health disorders, including serious mental illness.
Across racial and ethnic groups, past year receipt of mental health treatment was highest among White adults and lowest among Asian adults. In 2022, 28% of White adults reported receiving counseling and/or prescription medication for mental health conditions in the past year, compared to 16% of Hispanic and Black adults and 9% of Asian adults. A recent KFF poll found that, compared to their White peers, Hispanic, Black, and Asian adults disproportionately report challenges with mental health care utilization, including finding a provider who can understand their background and experiences, lack of information, and stigma or embarrassment. Additionally, the lack of a diverse mental health care workforce, absence of culturally informed treatment options, and stereotypes and discrimination associated with poor mental health may also contribute to limited mental health treatment among Black and Asian adults. Specifically among Asian people , cultural attitudes towards mental health are a factor that may lead to both lower reporting of mental health concerns and lower service utilization.
Adults with insurance coverage are more likely to report past year receipt of mental health care than adults without insurance coverage (25% vs. 11% in 2022, Figure 5). Despite higher utilization of mental health care over time – driven by insured adults – challenges remain with accessing services. For instance, KFF’s 2023 Consumer Survey found that 43% of insured adults with mental health concerns said there was a time in the past year when they did not get the mental health treatment they thought they needed, and 45% gave their insurance a negative rating for the availability of mental health providers. Further, KFF’s 2023 Employer Health Benefits Survey found that among employers offering health benefits, a higher share reported having a sufficient number of primary care providers in their plan’s networks (91%) compared to those who reported having a sufficient number of behavioral health care providers (67%).
This work was supported in part by the Well Being Trust. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
- Mental Health
- Utilization
news release
- The Share of Young Adults Who Received Mental Health Treatment Jumped 45% from 2019 to 2022, the Largest Increase Among Any Age Group
Also of Interest
- Racial and Ethnic Disparities in Mental Health Care: Findings from the KFF Survey of Racism, Discrimination and Health
- Recent Trends in Mental Health and Substance Use Concerns Among Adolescents
- Gaps in Mental Health Care for Asian and Pacific Islander People and Other People of Color

Workers appreciate and seek mental health support in the workplace

APA’s 2022 Work and Well-being Survey results
More than two years into the covid -19 pandemic, the workplace looks very different than it did before many businesses were forced to shut down or adjust their practices. Facing the stress of isolation, fears of the virus, and an overwhelming news cycle, it appears many workplace leaders have realized the need to address mental health concerns among their staff.
The results of APA’s 2022 Work and Well-being Survey reveal that seven in 10 workers (71%) believe their employer is more concerned about the mental health of employees now than in the past. This new focus is highly valued by employees. In fact, 81% of individuals said they will be looking for workplaces that support mental health when they seek future job opportunities.

There is, however, a need for improvement. The data reveals that mental health problems are associated with a number of workplace issues, such as compensation failing to keep up with inflation, electronic monitoring of employees, certain groups experiencing discrimination and feeling a lack of acceptance, and some employees even experiencing toxic or abusive workplaces. Further, those who work in manual labor and customer service are not having the same experience as those doing office work. Employers, therefore, should look for opportunities to make improvements and listen to feedback from workers .
APA commissioned The Harris Poll to conduct the survey to look at workplace experiences and how they have changed (or not changed) in light of the pandemic; measure employee stress related to work; and capture what employees are looking for from their employers regarding their mental health in the context of the pandemic and changing priorities. This survey builds upon prior APA Work and Well-being surveys that explored Americans’ attitudes toward the workplace.
Why—and how—employers should support their workers’ mental health
A majority (81%) of survey respondents said that employers’ support for mental health will be an important consideration when they look for work in the future—including 30% of workers who strongly agreed that employer support for mental health will factor into their future job decisions. Given this insight, employers should consider mental health initiatives as a way to recruit and retain talent.
Employers can offer mental health support to their employees in different ways. When asked to select from a list of a dozen possible supports that they would like to see employers offer, flexible work hours was the most commonly chosen support (41% of workers), followed by a workplace culture that respects time off (34%), the ability to work remotely (33%), and a four-day work week (31%).
Many employees reported that their employers already offer some of these supports , such as flexible work schedules (46%) and remote work options (37%). Fewer reported that their employers already offer a culture where time off is respected (28%) or four-day work weeks (14%). Interestingly, less than a third (30%) reported that their employer offers health insurance with coverage for mental health and substance use disorders. However, of those who reported that their employer does offer such insurance, 93% reported that such insurance is an effective mental health support.
When such supports are offered, many employees consider them beneficial. For example, among those whose employers offer flexible work hours and the opportunity to work remotely, 95% reported that these are effective supports. Only 11% reported that their employer has people on-site who have received mental health training. But of those who reported their employer does offer this support, 94% considered this support effective, including 45% who said the support is very effective. Similarly, although only 28% reported that their employer offers a culture where time off is respected, 96% of those whose employers respect time off said that it is effective, and 63% called it very effective.

Overall, employer-provided support for mental health has increased; 71% reported believing their employer is more concerned about the mental health of employees now than they were in the past. When asked specifically whether mental health and safety initiatives have gotten better compared with before the covid -19 pandemic, one-third (31%) said they had. The experience appears to be different depending on work context. About one-third of both office workers (34%) and customer service/client/patient services workers (32%) said it has gotten better compared with before the covid -19 pandemic, but only one-quarter of manual laborers (25%) reported the same. Further, those in customer service/client/patient services roles were more likely to say that mental health and safety initiatives have gotten worse (10%), compared with office workers (6%) and manual laborers (5%).
With the array of challenges and stresses that employees face at work, employers should look at opportunities to improve well-being and health—including the suggestions their own workers offer.
Concerns about compensation failing to keep up with inflation may be related to workers’ well-being
A majority of employees (71%) said they are worried that their compensation has not kept up with inflation. Further, nearly one-quarter (24%) reported that they do not feel they receive adequate compensation. The workers who do not feel they receive adequate compensation cited two main factors for feeling this way: Pay has not kept up with inflation (60%) and does not reflect all of the work they do (52%).
Those who are worried that their compensation has not kept up with inflation were also significantly more likely to report negative impacts of work on their psychological well-being than their counterparts. Nearly two in five of those worried their compensation has not kept up with inflation (39%) said their work environment has had a negative impact on their mental health compared with 21% of those who were not worried about compensation, and more than half of those who were worried about inflation’s impact on their compensation (54%) typically felt tense or stressed compared with 34% of those who were not worried.

Employees who worried about their compensation not keeping pace with inflation not only were more likely to express work as having negative impacts on their mental health but also indicated openness to other opportunities. Around two in five of these workers said they intend to look for a new job (37% compared with 25% who were not worried) and were nearly twice as likely to say they have a desire to quit their job (21% vs. 12%).

Compensation has long been a key driver for attracting and retaining talent. However, these results suggest that it may be more important now than ever for employers to keep a careful eye on compensation given our current environment of surging inflation.
Workplace monitoring is common—and sometimes harmful
More than half of employees (53%) said their employer uses computers, software, cameras, bar-code scanners, or other technologies to monitor them while they work, while 47% said that their employer does not monitor them (to their knowledge). Of those who reported knowing that they are monitored, about half (51%) said they felt uncomfortable with the way their employer uses technology to track them.

Working in environments with electronic monitoring was also associated with a variety of mental health concerns. Employees who said they are monitored at work were more likely to report problems with emotional or psychological well-being at work. Six in 10 (60%) of those who said their employer monitors them also said that they typically feel tense or stressed during the workday, in comparison with fewer than four in 10 (35%) of those who said they are not, to their knowledge, monitored at work. Employees who said they are monitored at work were also more likely to report that their work environment has a negative impact on their mental health (45% vs. 22% of those who are not monitored).

In addition, nearly one-quarter (23%) of those who said their employer monitors them consider their workplace experience somewhat or very toxic, compared with 13% of those who said their employer does not monitor them.
The use of monitoring technologies is not only associated with employees’ negative feelings about the workplace but also how they view their industry. More than half of employees who are monitored at work reported worrying about the future of their industry (51%). In contrast, less than one-third (31%) of those who said they are not monitored expressed concern for the future of their industry.
The data does not indicate whether such concerns and worries are due to monitoring or whether monitoring happens to be more prevalent in work environments where workers are more likely to express such concerns. Nonetheless, this data raises questions for employers who are electronically monitoring employees or considering doing so.

Diverse leadership at companies associated with equity, diversity, and inclusion policies
With recent heightened attention to issues related to race, sexual harassment, and gender, some employers have tried to cultivate more welcoming and inclusive workplaces. Based on the findings in this survey, companies with women, people of color, and LGBTQ+ individuals in senior leadership roles were more likely to have equity, diversity, and inclusion (EDI) policies, though whether an organization has such policies varied depending on the type of workplace.
Valuing equity helps diverse populations succeed and thrive. Diversity initiatives involve the representation or composition of various social identity groups in the workplace. Inclusion policies help ensure an environment that offers affirmation, celebration, and appreciation of different approaches, perspectives, and experiences.
Nearly two-thirds of workers at organizations with women (65%), racial and ethnic diversity (64%), or LGBTQ+ representation (66%) in senior leadership reported that their organization has diversity policies in place. These numbers were similar with regard to equity policies, which were reported by 67% of workers at organizations with women or racial and ethnic diversity in senior leadership, as well as 65% of those working for employers with LGBTQ+ representation in leadership positions. Comparable percentages of workers said their organizations have inclusion policies, with 65% of those whose employers have women or racial and ethnic diversity in senior leadership and 66% of those working for employers with LGBTQ+ representation reporting the presence of these policies in their workplace.
EDI policies are more commonly found in office settings than in manual labor workplaces. Compared with manual laborers, office workers were more likely to report their company has equity policies (61%) compared with manual laborers (49%), as well as diversity policies (60%) to (45%) and inclusion policies (60%) to (50%).

Younger workers more likely to view EDI policies as “mostly for show”
Even when an office has EDI initiatives, workers questioned whether they make a difference in the workplace culture. Among those who reported that their company has EDI initiatives, nearly half (47%) felt the efforts are mostly for show.
This view of EDI policies was most common for employees between ages 26 and 43; three-fifths (60%) of workers in this age group said the efforts are mostly for show. More than half of 18- to 25-year-olds (53%) also said they think the efforts are mostly for show, with much smaller percentages of older groups feeling the same. The percentage dropped to 37% among workers between ages 44 and 57, dropped to 29% among those 58 to 64, and to 25% of those 65 and older.

Overall, this data suggests that employers need to ensure that their EDI policies are meaningful, lead to measurable results, and are not merely “for show.”
Toxic and abusive workplace experiences are too common
Nearly one in five (18%) employees described their workplace as somewhat or very toxic. A toxic workplace was reported by 22% of employees in manual labor and 21% in customer service/client/patient services jobs, but a significantly lower percentage (15%) among those who have office jobs.

Harm in the form of harassment, verbal abuse, or physical violence in the workplace—either by someone within their organization or outside of it—has been experienced by three in 10 workers (30%) within the last year. More than one in five employees (22%) said someone within their organization (such as a coworker or manager) or outside their organization had abused them verbally in the workplace.

Many workers may not have experienced an abusive workplace but said they feel scared while at work. Black and Latino adults were more likely to say that they are often scared at work (29% for Black adults and 31% for Latino adults). Younger adults were also more likely to say that they are often scared when compared with adults ages 44 or older. A total of 38% of 18- to 25-year-olds and 32% of 26- to 43-year-olds reported feeling frightened at work compared with 17% of 44- to 57-year-olds, 10% of 58- to 64-year-olds, and 6% of workers age 65 and older.
While toxic and abusive workplaces are far from ubiquitous, this data suggests they remain too common, particularly in manual labor and customer service/client/patient services settings. This is an important issue for employers to monitor and address.
Workers from marginalized groups more likely to report discrimination
While 13% of all workers said they have been the target of discrimination (i.e., unequal treatment based on some aspect of identity such as race/ethnicity, gender, sexual orientation, ability status, age, etc.) in their workplace, this number was higher for employees from marginalized populations.
More than one-quarter of workers with a disability (27%) said they have been the target of discrimination in their workplace, while fewer than one in 10 workers without a disability (8%) said the same. Discrimination was experienced by more LGBTQ+ workers than non-LGBTQ+ workers (22% vs. 12%), and Black workers were nearly twice as likely as White workers to report that they have experienced discrimination on the job (21% vs. 11%). Workers with children were more than twice as likely as workers who are not parents or caregivers to say they have been the target of discrimination (19% vs. 9%).

Overall, this data shows that discrimination in the workplace unfortunately remains a serious issue, especially for those who are disabled, LGBTQ+, or Black.
Overall job satisfaction is high, but less so among manual laborers and service workers
The good news is that most Americans are very satisfied or somewhat satisfied with their jobs. However, Americans feel different about their satisfaction at work depending on their workplace environment. While 91% of all workers said they are very or somewhat satisfied with their jobs, this feeling was more common among office workers (92%) than among those who do manual labor (86%).

The survey also found variations in workers’ satisfaction across different demographics. For instance, a smaller percentage of LGBTQ+ workers (85%) reported being satisfied than non-LGBTQ+ workers (92%).
Respondents also varied in their satisfaction at work depending on socioeconomic, education, and workplace factors. A larger percentage of workers who have an annual household income of $50,000 or more (92%) reported that they are satisfied at work than those with an income under $50,000 (84%). Workers who have at least some post-high school education were more likely than those with a high school degree or less to feel satisfied at work (92% vs. 86%). And while most of those in upper-level roles (95%) were satisfied with their job, a smaller percentage of those in frontline positions (87%) said the same.
Similarly, those who work in an office were the most likely to say that changes related to work schedules are better today than they were prior to the pandemic (38% of office workers vs. 27% of manual laborers and 29% of customer service/client/patient services workers). One in 10 manual laborers (10%) said that work schedules are now worse, with a similar percentage of customer service/client/patient services workers saying the same (9%). Only 5% of office workers reported that current work schedules are worse than prepandemic.

With the shift toward remote office work resulting from the pandemic, attention to the psychological well-being of office workers has increased. This data, however, suggests employers may need to do more to focus on the needs of those in manual labor and customer service/client/patient services roles.
A variety of factors linked to job satisfaction
Just as they are satisfied at work overall, employees reported satisfaction with specific aspects of their jobs. Work schedule—which includes factors such as the number of hours worked and flexible scheduling options—was cited by 86% of workers as a satisfying aspect of their work. A majority of workers also said they are satisfied with the opportunities to be innovative or creative in their work (84%), how well their workplace is preparing them for their industry’s future (84%), the communication they receive from their employer (83%), the mental health support their employer provides (81%), and opportunities for growth and development where they work (81%).

The research was conducted online in the United States by The Harris Poll on behalf of APA among 2,016 adults aged 18+ who reside in the U.S. and are employed full-time, part-time, or self-employed. The survey was conducted April 22–May 2, 2022.
Data are weighted where necessary by age by gender, race/ethnicity, region, education, marital status, household size, work status, household income, and propensity to be online to bring them in line with their actual proportions in the population.
Respondents for this survey were selected from among those who have agreed to participate in our surveys. The sampling precision of Harris online polls is measured by using a Bayesian credible interval. For this study, the sample data is accurate to within plus or minus 3.3 percentage points using a 95% confidence level. This credible interval will be wider among subsets of the surveyed population of interest.
All sample surveys and polls, whether or not they use probability sampling, are subject to other multiple sources of error which are most often not possible to quantify or estimate, including, but not limited to coverage error, error associated with nonresponse, error associated with question wording and response options, and postsurvey weighting and adjustments.
Related resources
Survey resources.
- Survey questions (PDF, 156KB)
- Press release: APA poll shows employees plan to seek workplaces with mental health supports
- 2021 Work and Well-being report
- Press contact: Sophie Bethune Telephone: (202) 336-6134
Psychology and the workplace
- Topic: Healthy workplaces
- 5 ways to improve employee mental health
- Supporting employees’ psychological well-being for maximum return
- How organizations are leading in making employee mental health a priority
Webinar recording
How to foster mental health excellence in your workplace
Tune in as experts get to the core of APA’s 2022 Work and Well-being survey and break down how you can use this information. This event features a panel with leaders from two organizations who have made commitments to mental health excellence in their workplaces.
United States Institute of Peace
Home ▶ Publications
Six Lessons for Addressing Myanmar’s Mental Health Crisis
KEY TAKEAWAYS
- Years of conflict and the junta’s violence have created a mental health crisis in Myanmar.
- Local leaders have found innovative ways to address their communities’ emotional wellbeing.
- International organizations should support these local efforts to boost their inclusivity and effectiveness.
Tuesday, August 6, 2024
/ READ TIME: 8 minutes
By: Yu Yu Htay; Sarah Harper-Johnston; Divya Moorjani
There is a growing mental health crisis in Myanmar — one fueled by the junta’s violent atrocities against the population and a humanitarian crisis that has displaced an estimated 3.1 million people.

And even though Myanmar’s resistance maintains immense popular support and continues to gain momentum in its fight against the junta, the cumulative impact of sustained conflict and instability — both over the last three years and over the previous seven decades — means the crisis will only grow more dire the longer the struggle continues.
Meanwhile, years of systemic neglect and disinvestment have left resources for mental health scarce. But new USIP research reveals that local leaders are finding innovative ways to support their community’s mental health and emotional wellbeing — including through partnerships with religious actors.
USIP coordinated with The Network for Religious and Traditional Peacebuilders to learn more from these community support networks providing mental health and psychosocial support (MHPSS) to displaced people from Myanmar. Through this research initiative, we discovered that small-scale initiatives led by local community members — in collaboration with religious leaders — and mental health practitioners have proven effective despite limited resources. Integrating scientific knowledge with spiritual beliefs at the local level can significantly assist communities facing high-distress situations. Based on our findings, we have developed six recommendations for international organizations implementing MHPSS initiatives in Myanmar.
1. Support existing efforts of local actors rather than implementing new MHPSS initiatives.
Since the COVID pandemic and the 2021 military coup, there is a growing awareness of and interest in MHPSS needs in Myanmar. While much progress is still to be made, non-state actors and community-based providers, including local religious actors, have been pivotal in filling critical service delivery gaps amid the health system’s collapse. International organizations must develop creative mechanisms to support providers and religious leaders who are already implementing MHPSS initiatives and are enthusiastic to improve their technical capacity.
Religion serves as a primary source of strength and resilience in Myanmar — 99 percent of the population is affiliated with a religion — which makes religious leaders and actors uniquely positioned to offer effective MHPSS. Some religious actors and MHPSS providers in Myanmar are already linking MHPSS to religion and spirituality.
This integration is particularly evident among Christian and Buddhist leaders. Between the two, Christian communities appear to have better access to MHPSS systems, in part because pastoral counseling is a component of Christian religious leaders’ training. Buddhist leaders often provide psychosocial support through mindfulness and meditation practice, though it is currently more accessible to men than women.
International organizations should encourage both horizontal learning within and between these religious groups to enhance and build support for their services, share successful practices, and destigmatize MHPSS.
2. Complex layers of stigma require expertise and framing to be reversed effectively.
Most community support network participants agreed that there has been less stigma around struggling with and seeking mental health care since COVID and the coup. However, stigma remains — especially in rural communities.
This negative perception is further exacerbated when people seeking MHPSS wish to discuss topics that are considered taboo, such as domestic or sexual violence, discrimination on the basis of ethnic or sexual identity, or displacement due to armed conflict.
The topic of displacement is particularly of note. There is shame and fear associated with IDP (internally displaced person) status in Myanmar, as IDP camps have been a target of the junta’s violence toward civilians. So, although IDPs residing in camps supported by international organizations often have better access to MHPSS, individuals may be reluctant to reside in these camps and label themselves as IDPs.
Addressing these intersecting layers of stigma requires experts from Myanmar who understand cultural and social nuances. Mental health providers in Myanmar recommended utilizing non-clinical language and labeling MHPSS initiatives as resilience trainings, awareness raising or as community well-being meetings.
Community support networks explained that actors who hold influence in Myanmar, such as religious leaders, can also tackle the stigma directly by advocating that it is normal for individuals to struggle with their mental health given the current context. Additionally, community support networks from Myanmar noted it’s important to recognize and formalize practices such as community dialogue, creative activities and engagement in community events as valid methods of MHPSS.
Leveraging existing community practices will help frame interventions as opportunities for communal healing.
Leveraging existing community practices will help frame interventions as opportunities for communal healing, which better aligns with local and cultural perceptions, reduces reliance on external interventions, and ensures that MHPSS initiatives can integrate more seamlessly into the community fabric. Utilizing this localized approach will allow local vocabulary, beliefs rituals and understanding to guide the conversation, fostering a more inclusive and effective MHPSS environment.
3. Encourage women’s participation through a culturally intelligent lens.
Religious leadership across Buddhist, Christian, Hindu and Muslim communities in Myanmar is predominantly male. This gender dynamic creates barriers for women seeking psychosocial support, particularly when it is deemed inappropriate for women to interact privately with male religious figures. Such barriers are even more pronounced for women seeking care after experiencing sexual or gender-based violence, due to heightened fear of judgement.
To address these challenges, international organizations should ensure that women, even those not in leadership positions, are included in trainings. It is essential to involve women not only as training participants, but also to support MHPSS initiatives with women in visible and impactful roles. This requires creating connections with local actors who can facilitate women’s involvement in a manner than respects cultural and religious practices while also empowering women to take on leadership roles in their communities.
4. Uplift and empower youth participation, while not excluding elder leaders.
Younger people in Myanmar tend to have more knowledge regarding MHPSS and are open to incorporating mental health practices into religious psychosocial support. In comparison, some older generations tend to have stronger stigmas against individuals suffering from mental health disorders.
However, it is important that elder religious leaders are still involved in local-level MHPSS initiatives because they often have longstanding trust and respect within their communities. In some places, it can even be perceived as inappropriate or threatening if an activity is implemented without receiving endorsement from community elders.
Strategies for promoting intergenerational collaboration in MHPSS initiatives that include both youth and elder leaders should be explored. Furthermore, as with gender, there is a need to redefine participation and leadership roles within MHPSS initiatives to allow young people to take active, visible leadership positions while also ensuring that elders have significant, ongoing input into the direction and decisions of the initiatives. Such models could support the bridging of generational divides and leverage the unique strengths of each group.
5. To effectively navigate the diversity and complexity of Myanmar, develop and implement MHPSS projects in collaboration with local actors.
These actors, especially those already providing MHPSS, have the cultural understanding and social context to combat stigma, navigate ethnic or religious tensions, and meaningfully include marginalized groups.
International providers who do not understand the complexities of the local context risk inadvertently causing harm. For example, there are social hierarchies within ethnic groups that can inhibit an MHPSS provider’s ability to build trust within certain communities. If a religious leader provides psychosocial care to somebody who does not practice the same religion, this could exacerbate ethnic tensions and discrimination or be perceived as proselytizing.
International providers who do not understand the complexities of the local context risk inadvertently causing harm.
This does not mean that involving providers or trainers of different religions and ethnic groups will always exacerbate divisions — these trainings can be opportunities for inter-religious inter-ethnic relationships to form — but it is important for the implementer to be a local actor who has experience and awareness on how to successfully navigate these dynamics.
Community support networks from Myanmar also shared there is a negative perception among people in Myanmar of some international organizations. This stems from the fact some international organizations registered with the junta to maintain an in-country office or receive visas for their international staff to work in the country. By partnering with trusted local leaders and uplifting their initiatives, international programs can overcome this perception, and reach displaced communities in need that are unable to access other forms of MHPSS.
6. Collaborate safely with local actors in Myanmar to assess challenges and mitigate risk.
Safety concerns associated with the ongoing armed conflict often impede mental service providers’ travel from urban areas to rural conflict areas, and it is difficult to hold online sessions due to limited electricity , internet access and recent restrictions on VPNs .
As mentioned previously, partnering with local organizations that are already implementing MHPSS in Myanmar is crucial, as they have a better grasp of how to navigate the operational challenges. Local partners understand the risks associated with holding activities better than international organizations and can help make informed decisions.
For example, research participants spoke of trainings that required long, dangerous travel. As one community support network member explained, travel should be organized in collaboration with actors currently residing in Myanmar, to identify routes that are safe from active conflict and natural disasters. It is imperative that MHPSS initiatives are developed with individuals who have recent experience on how to safely travel and conduct activities. Collaborations should emphasize adaptive programming that can swiftly respond to the volatile political and social dynamics within Myanmar, particularly in conflict-prone and border areas.
Religious actors and mental health providers are the best source for localizing MHPSS in Myanmar. With the violent conflict escalating , there are a growing number of areas where the military is no longer present. A reconstruction effort in those areas must include a MHPSS component to effectively address the intergenerational trauma and impact of violent conflict. By setting the MHPSS groundwork now, the future leaders will be better equipped to support a new transition once the military falls.
Yu Yu Htay is a program officer for the Myanmar team at USIP.
Sarah Harper-Johnston is a program specialist for Myanmar at USIP.
Divya Moorjani is the regional programme manager for Asia at the Network for Religious and Traditional Peacemakers.
The views expressed in this publication are those of the author(s).
PUBLICATION TYPE: Analysis
Back to The Library

Yes, Play Is Good for Children’s Mental Health — Here’s What the Data Says
July 30, 2024
Data that highlights how free play affects children’s mental health, including happiness, social skills, and more.
By: Charlie Health Editorial Team
Clinically Reviewed By: Meghan Jensen
Learn more about our Clinical Review Process
Table of Contents
Children are playing independently less than they used to — and, according to many experts, missing out on this quintessential childhood experience is taking a toll on their mental health. Some even say that decreased free play, defined as unstructured play without adult supervision, is fueling the youth mental health crisis more than social media usage .
To be sure, more time on screens, as well as an increase in parental supervision and academic pressures , may all contribute to the reduction in free play in the last half-century. Between 1950 and 2010, the average length of the school year in the United States increased by five weeks, and by 2014, the average elementary schooler spent less than 30 minutes a day in recess, data shows . Also, homework, which was once rare or nonexistent in elementary school, is now common even in kindergarten. All told, there’s less time for play.
Among the staunchest advocates of free play is renowned psychologist Dr. Peter Gray . In a 2011 study , Dr. Gray found that free play teaches young people how to learn decision-making and problem-solving skills, regulate their emotions , build friendships, and more. Without play, rates of anxiety, depression, suicide, and narcissism increase, the study posits. “Everything that I know about play suggests that if you take play away from children, there’s going to be negative consequences,” Dr. Gray told the Boston Globe earlier this year.
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
Thank you for signing up!
You can unsubscribe anytime..
To assess how play impacts youth mental health, Charlie Health combed through the numbers, looking at data on how play is linked with happiness, social skills, and more. Keep reading to see what the data reveals.
Play is linked to stronger social skills among children
A 2015 review of 18 international studies involving about 50,000 children and youth found that play is positively associated with children’s social skills . The studies, which explored various types of risky play (a kind of free play that involves risk within safe boundaries), found that children who can disappear or get lost during play or play involving great heights or rough and tumble activities are shown to have increased social competence. Similarly, an earlier study of children (ages six months to 2.5 years) in an orphanage found that months of play improved social skills by nearly 50% (61.9 to 91.3 according to the study’s metrics).
Children’s physical ability is also linked to play
The same studies positively linked play with children’s physical abilities. The 2015 review found that risky play is linked to increased regular and intense physical activity in children. Similarly, after months of play, the children in the orphanage saw a roughly 30% increase in motor skills (63.7 to 91.3 according to the study’s metrics). According to the study, children in the orphanage also became more active, playful, and responsive to play.
Happiness and play are linked among children
Even a small amount of play is positively linked with happiness among children, one study found. According to research conducted in 2020 with 42 preschool children (aged four to six), one hour of play and 10 minutes of indoor mindfulness over five days increased children’s happiness by nearly 20% (pretest happiness score: 4; posttest happiness score: 4.7). This increase is considered significant according to the researchers.
Rising childhood ADHD rates may be linked to reduced free play
An increasing number of children are getting diagnosed with attention-deficit/hyperactivity disorder (ADHD), and free play could be part of the equation. One study found that reduced opportunities for preschool children to engage in spontaneous social play may contribute to rising ADHD diagnoses. The study notes that play helps develop the brain’s ability to regulate impulsive emotions — a classic symptom of ADHD, which may worsen without play, according to the study.
Similarly, a 2013 study of children found that more time spent in unstructured quiet play during toddler and preschool years correlated with better self-regulation abilities later on, even when earlier self-regulation skills and other factors were considered. Additionally, the 2013 study found that preschoolers who engaged in one to five hours of unstructured active play showed significant improvements in self-regulation two years later.
How to support children’s mental health through play
Supporting children’s mental health with play is, first and foremost, a systemic issue. Above all, providers, researchers, and lawmakers need to raise awareness of how play impacts mental health and create more opportunities for children to play. Below are some other steps that can be taken to promote play and children’s mental health.
Encourage free play
Limit screen time.
Seek play therapy (and mental healthcare) as needed
It may seem obvious, but encourage your children to engage in unstructured, self-directed play at any time during the day. As shown in the above studies, even a limited amount of free play can help young people develop social skills and improve their overall physical ability and happiness. Free play can include outdoor play, play with other children, and play using diverse materials, such as building blocks, art supplies, dress-up clothes, and more.
A growing body of research suggests that prolonged screen time can negatively impact children's physical health, sleep patterns, and social development. Instead, encourage activities that promote physical movement and creativity, such as outdoor play, sports, arts and crafts, and imaginative games. These activities not only support physical health but also foster social skills, cognitive development, and emotional well-being.
Seek play therapy (and mental healthcare) as needed
Just like play itself, data shows that play therapy (a therapeutic approach that uses play) can give children useful tools and experiences to manage and improve their mental health. If your child is struggling with their mental health, consider looking for providers or organizations that incorporate play therapy into treatment — like Charlie Heath .
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8812369/
https://www.sciencedirect.com/science/article/pii/S0885200621001411
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2242642/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7432887/
https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-2214.2002.00246.x
https://www.mdpi.com/1660-4601/12/6/6423
https://neurosciencenews.com/child-psychology-play-22750/
Comprehensive mental health treatment from home
90% of Charlie Health clients and their families would recommend Charlie Health
More like this

Ways To Practice Self-Care as a Teen
Charlie Health Editorial Team

11 Best Parenting Books, According to Charlie Health Providers

5 Ways For Parents To Tell Their Kids That It’s Okay To Not Be Okay

Get the mental health treatment you deserve
Need additional mental health support? Charlie Health can help. Get started with virtual intensive therapy now.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Association of breastfeeding with mental disorders in mother and child: a systematic review and meta-analysis
Affiliations.
- 1 Charité - Universitätsmedizin Berlin, Einstein Center for Neurosciences, Berlin, Germany.
- 2 V. Serbsky Federal Medical Research Center for Psychiatry and Narcology of the Ministry of Health of the Russian Federation, Moscow, Russia.
- 3 Moscow Research and Clinical Centre for Neuropsychiatry, Moscow, Russia.
- 4 Moscow City Clinical Hospital After V.M. Buyanov, Moscow, Russia.
- 5 Department of Brain Sciences, Faculty of Medicine, Dementia Research Institute UK, Imperial College London, London, UK.
- 6 Endocrinology Research Centre, Moscow, Russia.
- 7 Stroke Unit, Santa Maria Della Misericordia Hospital, University of Perugia, Perugia, Italy.
- 8 Division of Clinical Immunology & Allergy, Department of Medicine, and Department of Health Research Methods, Evidence & Impact, McMaster University, Hamilton, Canada.
- 9 Department of Pediatrics, Pediatric Epidemiology, Medical Faculty, Leipzig University, Leipzig, Germany.
- 10 German Center for Child and Youth Health, Leipzig, Germany.
- 11 Department of Pediatrics, Paracelsus Medical University, Klinikum Nürnberg, Universitätsklinik Der Paracelsus Medizinischen Privatuniversität Nürnberg, Nuremberg, Germany.
- 12 Department of Pediatrics, Paracelsus Medical University, Salzburg, Austria.
- 13 Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK.
- 14 Department of Paediatrics and Paediatric Infectious Diseases, Institute of Child's Health, I.M. Sechenov First Moscow State Medical University, Sechenov University, Moscow, Russia.
- 15 National Heart and Lung Institute, Imperial College London, London, UK. [email protected].
- 16 National Heart and Lung Institute, Imperial College London, London, UK. [email protected].
- 17 Care for Long Term Conditions Division, Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, King's College London, London, UK. [email protected].
- 18 I.M. Sechenov First Moscow State Medical University, Sechenov University, Moscow, Russia. [email protected].
- 19 Department of Infectious Disease, Faculty of Medicine, Imperial College London, London, United Kingdom. [email protected].
- PMID: 37840122
- PMCID: PMC10577970
- DOI: 10.1186/s12916-023-03071-7
Background: Breastfeeding has long been associated with numerous benefits for both mothers and infants. While some observational studies have explored the relationship between breastfeeding and mental health outcomes in mothers and children, a systematic review of the available evidence is lacking. The purpose of this study is to systematically evaluate the association between breastfeeding and mental health disorders in mothers and children.
Methods: We systematically searched MEDLINE and EMBASE from inception to June 2, 2023. The inclusion criteria consisted of all studies evaluating links between breastfeeding and development of mental health disorders in children and mothers. Risk of bias was assessed using the Newcastle-Ottawa Scale (NOS) while grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to assess the certainty of evidence. A random-effects meta-analysis was used if possible, to estimate the odds ratio for the association between breastfeeding and mental health outcomes. The Mantel-Haenszel method was utilised for pooling ORs across studies. Study heterogeneity was assessed using the I 2 statistic.
Results: Our review identified twenty-one original study. Of these, 18 focused on the association between breastfeeding and child health, assessing depressive disorders, schizophrenia, anxiety disorders, eating disorders and borderline personality disorder. Three studies evaluated the associations between breastfeeding and maternal mental health disorders. Three studies looking at outcomes in children showed no significant association between breastfeeding and occurrence of schizophrenia later in life (OR 0.98; 95% CI 0.57-1.71; I 2 = 29%). For depressive disorders (5 studies) and anxiety disorders (3 studies), we found conflicting evidence with some studies showing a small protective effect while others found no effect. The GRADE certainty for all these findings was very low due to multiple limitations. Three studies looking at association between breastfeeding and maternal mental health, were too heterogeneous to draw any firm conclusions.
Conclusions: We found limited evidence to support a protective association between breastfeeding and the development of mental health disorders in children later in life. The data regarding the association between breastfeeding and maternal mental health beyond the postnatal period is also limited. The methodological limitations of the published literature prevent definitive conclusions, and further research is needed to better understand the relationship between breastfeeding and mental health in mothers and children.
Keywords: Anxiety disorders; Breastfeeding; Child health; Depressive disorders; Maternal health; Mental health; Schizophrenia; Systematic review.
© 2023. BioMed Central Ltd., part of Springer Nature.
PubMed Disclaimer
Conflict of interest statement
The authors declare no support from any organisation for the submitted work. Outside of the submitted work, JG benefit from unrestricted research grants from Danone Nutricia Research to Leipzig University for research into human milk composition within the Ulm Birth Cohort Studies—this work is not related to the present publication; author RJB declares consultancy payment from Cochrane, Wiley and the British Society for Allergy and Clinical Immunology for editorial work and payment for expert witness work in cases involving food anaphylaxis and a disputed infant formula health claim.
PRISMA flow diagram
Meta-analysis of case–control studies. Breastfeeding…
Meta-analysis of case–control studies. Breastfeeding (ever vs. never) and risk of schizophrenia. 1.1.1.…
Similar articles
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P. Crider K, et al. Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217. Cochrane Database Syst Rev. 2022. PMID: 36321557 Free PMC article.
- Schedules for home visits in the early postpartum period. Yonemoto N, Nagai S, Mori R. Yonemoto N, et al. Cochrane Database Syst Rev. 2021 Jul 21;7(7):CD009326. doi: 10.1002/14651858.CD009326.pub4. Cochrane Database Syst Rev. 2021. PMID: 34286512 Free PMC article.
- Interventions for supporting the initiation and continuation of breastfeeding among women who are overweight or obese. Fair FJ, Ford GL, Soltani H. Fair FJ, et al. Cochrane Database Syst Rev. 2019 Sep 17;9(9):CD012099. doi: 10.1002/14651858.CD012099.pub2. Cochrane Database Syst Rev. 2019. PMID: 31529625 Free PMC article.
- Early skin-to-skin contact for mothers and their healthy newborn infants. Moore ER, Bergman N, Anderson GC, Medley N. Moore ER, et al. Cochrane Database Syst Rev. 2016 Nov 25;11(11):CD003519. doi: 10.1002/14651858.CD003519.pub4. Cochrane Database Syst Rev. 2016. PMID: 27885658 Free PMC article. Review.
- Efficacy of behavioral interventions to improve maternal mental health and breastfeeding outcomes: a systematic review. Pezley L, Cares K, Duffecy J, Koenig MD, Maki P, Odoms-Young A, Clark Withington MH, Lima Oliveira M, Loiacono B, Prough J, Tussing-Humphreys L, Buscemi J. Pezley L, et al. Int Breastfeed J. 2022 Sep 5;17(1):67. doi: 10.1186/s13006-022-00501-9. Int Breastfeed J. 2022. PMID: 36064573 Free PMC article. Review.
- Breastfeeding is associated with enhanced intestinal gluconeogenesis in infants. Ni D, Tan J, Macia L, Nanan R. Ni D, et al. BMC Med. 2024 Mar 7;22(1):106. doi: 10.1186/s12916-024-03327-w. BMC Med. 2024. PMID: 38454391 Free PMC article.
- Novel insights from our special issue on maternal factors during pregnancy that influence maternal, fetal and childhood outcomes. Tong S, Benhalima K, Muglia L, Ozanne S. Tong S, et al. BMC Med. 2024 Feb 20;22(1):79. doi: 10.1186/s12916-024-03278-2. BMC Med. 2024. PMID: 38378546 Free PMC article. No abstract available.
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications a systematic review and meta-analysis. JAMA Psychiat. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. - DOI - PMC - PubMed
- Mental GBD, Collaborators D Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50. doi: 10.1016/S2215-0366(21)00395-3. - DOI - PMC - PubMed
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858. - PMC - PubMed
- Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. - DOI - PMC - PubMed
- Sickel AE, Seacat JD, Nabors NA. Mental health stigma update: a review of consequences. Adv Ment Heal. 2014;12(3):202–215. doi: 10.1080/18374905.2014.11081898. - DOI
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
- MedlinePlus Consumer Health Information
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Two research teams awarded grants toward student mental health studies

Professors Emily Seto and Daniel Grace are among five University of Toronto researchers who have been awarded 2023-24 Inlight Research Development Grants to advance knowledge and develop solutions to complex issues related to student mental health.
The grant program grew out of U of T’s response to the 2020 final report U of T’s Presidential & Provostial Task Force on Student Mental Health that resulted in a partnership with the Centre for Addictions & Mental Health (CAMH) to collaboratively determine new research directions that may require integrated, interdisciplinary approaches.
Supporting international students living on campus
Associate Prof. Seto’s research project titled Residence-Based Mental Health Literacy Education for International Students targets the needs of international students living in residence and will explore ways to support and promote their mental health as they adjust to a new country and the university environment. Seto is a Professional Engineer of Ontario and the incoming Program Director of the Health Systems Research Program at the Institute of Health, Policy, Management and Evaluation (IHPME).
Amika Shah, a PhD student supervised by Seto, is leading the research. “This is a drastic transition for international students, beyond just the traditional life stage transition,” says Shah. “We want to focus on providing support to them where they are, since there is a strong residence life system with staff who support students 24/7. There’s an opportunity to provide specific resources and materials tailored to the students’ needs.”

Amika Shah, a PhD student supervised by Seto, is leading the research project on international students living in residence.
Seto notes that the research is very timely, given the impact that the pandemic has had on mental health and the impact of world events on students, who don’t have the same support networks as their domestic counterparts.
Their work will involve interviewing students, including them in the co-design of programs and materials and creating prototypes to share with residence staff for feedback. Their hope is that the resulting materials and programs can be included in residence life staff training to support international students better.
“We are thrilled and grateful to have received this award so that we can develop novel ways to support the well-being of international students, particularly at this time when there are so many pressing factors that can impact their mental health,” says Seto. “I’m also excited that this award will support Amika to expand her impactful research on tailored tools to improve well-being and mental health literacy.”
Improving mental health care services for 2SLGBTQ+ students
Associate Prof. Grace’s research project is titled Strengthening Services to Support the Mental Health Needs of Diverse 2SLGBTQ+ Students Across the University of Toronto: Planning and Partnership Development. The research will be led by Sarah Smith, PhD, lead research associate on Grace’s team. It continues a project that is exploring the experiences that 2SLGBTQ+ students have in accessing healthcare.
Previously, Smith and the team interviewed 30 2SLGBTQ+ students about their interactions with the health care system, along with a few U of T student life and equity, diversity and inclusion (EDI) professionals. Now, thanks to the grant, they plan to engage with university mental health care professionals to determine “how they understand what 2SLGBTQ+ students need and how comfortable they feel supporting these students on issues such as gender and sexuality,” Smith says. “Are there things they need to know and things that get missed in translation?”

Sarah Smith, PhD, is the lead research associate focusing on the health needs of 2SLGBTQ+ students.
Smith hopes to bridge the gap between students and providers and offer guidance that will make sure the system meets their needs.
“We realize things won’t change overnight, but it’s important to bring our data, observations and recommendations to the university,” Smith says. “Currently, a lot of 2SLGBTQ+ students cannot find the care they need in the university health care system and opt to pay for services elsewhere.
“I am so looking forward to connecting with other folks at the University of Toronto whose passions also lie in student mental health. I know there are a lot of really exciting and productive discussions to be had.”
Grace, the 2SLGBTQ+ Health Lead at DLSPH and director of DLSPH’s Centre for Sexual and Gender Minority Health Research, is eager to have his team pursue this project.
“We are committed to leading research and knowledge mobilization efforts to improve the experiences of diverse 2SLGBTQ+ students across the University, including available mental health services,” he says. “It is necessary that we listen to the needs of 2SLGBTQ+ students, and work collectively across the university to remove structural barriers to accessing services.”
“Our research to date has highlighted the importance of hiring more 2SLGBTQ+ counsellors and making counsellors who specialize in 2SLGBTQ+ issues more easily identifiable. Students want increased access to consistent, ongoing counselling as well as increased access to trauma-informed therapy. We must also do a better job at ensuring that students know what mental health services are available at the university.”
By Elaine Smith
- Programs+Policy

Heartland Forward has identified opportunities to improve mental health care across the heartland as we work to be a resource for states and local communities – supporting quality of life and overall economic success in the middle of the country.
- “Mental health services tailored for the unique needs of pregnant and postpartum women are indispensable in supporting their mental and emotional health during this transformative period. Additionally, timely and appropriate mental health care can bolster physical health, offering long-term wellness benefits.”
- “Maternal Mortality Review Committees (MMRCs) highlight mental health conditions, including suicide and overdose related to substance use disorder, as the leading underlying causes of maternal mortality, accounting for more than 23% of pregnancy-related deaths between 2017 and 2019.”
- “ Good physical and mental health is an important economic development and a quality-of-life issue for rural America. It is key to having a happier and more productive community and workforce, which, in turn, leads to a higher gross regional product (GRP), reducing the strain on state budgets related to overall health care spending.”
- “The advancement of telehealth helps bridge gaps in access to care and improves outcomes for pregnant women and their babies.”
- “Telehealth allows for closer monitoring of high-risk pregnancies, with regular check-ins and remote monitoring of vital signs and fetal health.”
Programming
- One of the primary actions of the Heartland Health Caucus is to focus on making community health workers a sustainable workforce across the heartland. Community health workers like paraprofessionals can effectively target less complex cases in mental health by providing early intervention – with an opportunity to potentially cut health care costs down the road.

- Liberty University
- Jerry Falwell Library
- Special Collections
- < Previous
Home > ETD > Doctoral > 5903
Doctoral Dissertations and Projects
Triple-negative breast cancer survivors: post-traumatic stress disorder, post-traumatic growth, quality of life, and unmet mental health needs.
Carla Horton Gray , Liberty University Follow
School of Behavioral Sciences
Doctor of Philosophy in Psychology (PhD)
Natalie Hamrick
PTSD, breast cancer, hormone-fed breast cancer, triple-negative breast cancer, TNBC, depression, anxiety, chemotherapy, survivor
Disciplines
Recommended citation.
Gray, Carla Horton, "Triple-Negative Breast Cancer Survivors: Post-Traumatic Stress Disorder, Post-Traumatic Growth, Quality of Life, and Unmet Mental Health Needs" (2024). Doctoral Dissertations and Projects . 5903. https://digitalcommons.liberty.edu/doctoral/5903
The purpose of this mixed-method study was to investigate levels of PTSD, PTG, QOL, their relationships, and unmet mental health needs of triple-negative breast cancer survivors diagnosed between stages 2b-4 and 2-5 years post-treatment. Participants were recruited through two cancer organizations, breast health navigators, TNBC support groups, and online breast cancer support groups. Sixty-one participants completed the PTSD Checklist-Civilian Version (PCL-C), Post-Traumatic Growth Inventory, and the Functional Assessment of Cancer Therapy-Breast (FACT-B). Thirty participants completed the optional short answer questions about unmet mental health needs. Participants’ mean score of 48 (SD=12.22) on the PCL-C was higher than 44, PTSD scores above 44 are considered indicative of PTSD (t(60) 2.38, p = 0.02), according to the Department of Veteran Affairs. Participants had moderate levels of PTG and moderate levels of QOL. Compared to the published sample of TNBC patients during treatment, this sample of TNBC survivors 2-5 years post-treatment had lower total QOL (M = 80.67,SD = 19.88) (t(60) =-3.70, p < .001), as well as lower QOL for all subscales. Lower PTSD (b = -1.15, p < .001) and higher PTG (b = -1.15, p < .001) both predicted higher total QOL. The qualitative short answer questions revealed important themes for mental health like the need for therapy and counseling, lack of information and support, and lack of understanding, care, and information on the transition into survivorship. Anxiety and fear of recurrence were the top reported mental health challenges. Mental health symptoms of depression, anxiety, and the need for support were identified as unmet mental health needs currently, which supports current research’s future application of prevention, identification, and interventions or treatments.
Since August 09, 2024
Included in
Psychology Commons
- Collections
- Faculty Expert Gallery
- Theses and Dissertations
- Conferences and Events
- Open Educational Resources (OER)
- Explore Disciplines
Advanced Search
- Notify me via email or RSS .
Faculty Authors
- Submit Research
- Expert Gallery Login
Student Authors
- Undergraduate Submissions
- Graduate Submissions
- Honors Submissions
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Social Media and Mental Health: Benefits, Risks, and Opportunities for Research and Practice
John a. naslund.
a Department of Global Health and Social Medicine, Harvard Medical School, Boston, MA
Ameya Bondre
b CareNX Innovations, Mumbai, India
John Torous
c Department of Psychiatry, Beth Israel Deaconess Medical Center, Boston, MA
Kelly A. Aschbrenner
d Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, NH
Social media platforms are popular venues for sharing personal experiences, seeking information, and offering peer-to-peer support among individuals living with mental illness. With significant shortfalls in the availability, quality, and reach of evidence-based mental health services across the United States and globally, social media platforms may afford new opportunities to bridge this gap. However, caution is warranted, as numerous studies highlight risks of social media use for mental health. In this commentary, we consider the role of social media as a potentially viable intervention platform for offering support to persons with mental disorders, promoting engagement and retention in care, and enhancing existing mental health services. Specifically, we summarize current research on the use of social media among mental health service users, and early efforts using social media for the delivery of evidence-based programs. We also review the risks, potential harms, and necessary safety precautions with using social media for mental health. To conclude, we explore opportunities using data science and machine learning, for example by leveraging social media for detecting mental disorders and developing predictive models aimed at characterizing the aetiology and progression of mental disorders. These various efforts using social media, as summarized in this commentary, hold promise for improving the lives of individuals living with mental disorders.
Introduction
Social media has become a prominent fixture in the lives of many individuals facing the challenges of mental illness. Social media refers broadly to web and mobile platforms that allow individuals to connect with others within a virtual network (such as Facebook, Twitter, Instagram, Snapchat, or LinkedIn), where they can share, co-create, or exchange various forms of digital content, including information, messages, photos, or videos ( Ahmed, Ahmad, Ahmad, & Zakaria, 2019 ). Studies have reported that individuals living with a range of mental disorders, including depression, psychotic disorders, or other severe mental illnesses, use social media platforms at comparable rates as the general population, with use ranging from about 70% among middle-age and older individuals, to upwards of 97% among younger individuals ( Aschbrenner, Naslund, Grinley, et al., 2018 ; M. L. Birnbaum, Rizvi, Correll, Kane, & Confino, 2017 ; Brunette et al., 2019 ; Naslund, Aschbrenner, & Bartels, 2016 ). Other exploratory studies have found that many of these individuals with mental illness appear to turn to social media to share their personal experiences, seek information about their mental health and treatment options, and give and receive support from others facing similar mental health challenges ( Bucci, Schwannauer, & Berry, 2019 ; Naslund, Aschbrenner, Marsch, & Bartels, 2016b ).
Across the United States and globally, very few people living with mental illness have access to adequate mental health services ( Patel et al., 2018 ). The wide reach and near ubiquitous use of social media platforms may afford novel opportunities to address these shortfalls in existing mental health care, by enhancing the quality, availability, and reach of services. Recent studies have explored patterns of social media use, impact of social media use on mental health and wellbeing, and the potential to leverage the popularity and interactive features of social media to enhance the delivery of interventions. However, there remains uncertainty regarding the risks and potential harms of social media for mental health ( Orben & Przybylski, 2019 ), and how best to weigh these concerns against potential benefits.
In this commentary, we summarized current research on the use of social media among individuals with mental illness, with consideration of the impact of social media on mental wellbeing, as well as early efforts using social media for delivery of evidence-based programs for addressing mental health problems. We searched for recent peer reviewed publications in Medline and Google Scholar using the search terms “mental health” or “mental illness” and “social media”, and searched the reference lists of recent reviews and other relevant studies. We reviewed the risks, potential harms, and necessary safety precautions with using social media for mental health. Overall, our goal was to consider the role of social media as a potentially viable intervention platform for offering support to persons with mental disorders, promoting engagement and retention in care, and enhancing existing mental health services, while balancing the need for safety. Given this broad objective, we did not perform a systematic search of the literature and we did not apply specific inclusion criteria based on study design or type of mental disorder.
Social Media Use and Mental Health
In 2020, there are an estimated 3.8 billion social media users worldwide, representing half the global population ( We Are Social, 2020 ). Recent studies have shown that individuals with mental disorders are increasingly gaining access to and using mobile devices, such as smartphones ( Firth et al., 2015 ; Glick, Druss, Pina, Lally, & Conde, 2016 ; Torous, Chan, et al., 2014 ; Torous, Friedman, & Keshavan, 2014 ). Similarly, there is mounting evidence showing high rates of social media use among individuals with mental disorders, including studies looking at engagement with these popular platforms across diverse settings and disorder types. Initial studies from 2015 found that nearly half of a sample of psychiatric patients were social media users, with greater use among younger individuals ( Trefflich, Kalckreuth, Mergl, & Rummel-Kluge, 2015 ), while 47% of inpatients and outpatients with schizophrenia reported using social media, of which 79% reported at least once-a-week usage of social media websites ( Miller, Stewart, Schrimsher, Peeples, & Buckley, 2015 ). Rates of social media use among psychiatric populations have increased in recent years, as reflected in a study with data from 2017 showing comparable rates of social media use (approximately 70%) among individuals with serious mental illness in treatment as compared to low-income groups from the general population ( Brunette et al., 2019 ).
Similarly, among individuals with serious mental illness receiving community-based mental health services, a recent study found equivalent rates of social media use as the general population, even exceeding 70% of participants ( Naslund, Aschbrenner, & Bartels, 2016 ). Comparable findings were demonstrated among middle-age and older individuals with mental illness accessing services at peer support agencies, where 72% of respondents reported using social media ( Aschbrenner, Naslund, Grinley, et al., 2018 ). Similar results, with 68% of those with first episode psychosis using social media daily were reported in another study ( Abdel-Baki, Lal, D.-Charron, Stip, & Kara, 2017 ).
Individuals who self-identified as having a schizophrenia spectrum disorder responded to a survey shared through the National Alliance of Mental Illness (NAMI), and reported that visiting social media sites was one of their most common activities when using digital devices, taking up roughly 2 hours each day ( Gay, Torous, Joseph, Pandya, & Duckworth, 2016 ). For adolescents and young adults ages 12 to 21 with psychotic disorders and mood disorders, over 97% reported using social media, with average use exceeding 2.5 hours per day ( M. L. Birnbaum et al., 2017 ). Similarly, in a sample of adolescents ages 13-18 recruited from community mental health centers, 98% reported using social media, with YouTube as the most popular platform, followed by Instagram and Snapchat ( Aschbrenner et al., 2019 ).
Research has also explored the motivations for using social media as well as the perceived benefits of interacting on these platforms among individuals with mental illness. In the sections that follow (see Table 1 for a summary), we consider three potentially unique features of interacting and connecting with others on social media that may offer benefits for individuals living with mental illness. These include: 1) Facilitate social interaction; 2) Access to a peer support network; and 3) Promote engagement and retention in services.
Summary of potential benefits and challenges with social media for mental health
| Features of Social Media | Examples | Studies |
|---|---|---|
| 1) Facilitate social interaction | • Online interactions may be easier for individuals with impaired social functioning and facing symptoms • Anonymity can help individuals with stigmatizing conditions connect with others • Young adults with mental illness commonly form online relationships • Social media use in individuals with serious mental illness associated with greater community and civic engagement • Individuals with depressive symptoms prefer communicating on social media than in-person • Online conversations do not require iimnediate responses or non-verbal cues | ( ; ; ; ; ; ; ; ) |
| 2) Access to peer support network | • Online peer support helps seek information, discuss symptoms and medication, share experiences, learn to cope and for self-disclosure. • Individuals with mental disorders establish new relationships, feel less alone or reconnect with people. • Various support patterns are noted in these networks (e.g. ‘informational’, ‘esteem’, ‘network’ and ‘emotional’) | ( ; ; ; ; ; ; ; ; ) |
| 3) Promote engagement and retention in services | • Individuals with mental disorders connect with care providers and access evidence-based services • Online peer support augments existing interventions to improve client engagement and compliance. • Peer networks increase social connectedness and empowerment during recovery. • Interactive peer-to-peer features of social media enhance social functioning • Mobile apps can monitor symptoms, prevent relapses and help users set goals • Digital peer-based interventions target fitness and weight loss in people with mental disorders • Online networks support caregivers of those with mental disorders | ( ; ; ; ; ; ; ; ; ; ; ; ; ) |
| 1) Impact on symptoms | • Studies show increased exposure to harm, social isolation, depressive symptoms and bullying • Social comparison pressure and social isolation after being rejected on social media is coimnon • More frequent visits and more nmnber of social media platforms has been linked with greater depressive symptoms, anxiety and suicide • Social media replaces in-person interactions to contribute to greater loneliness and worsens existing mental symptoms | ( ; ; ; ; ; ; ; ; ; ; ; ) |
| 2) Facing hostile interactions | • Cyberbullying is associated with increased depressive and anxiety symptoms • Greater odds of online harassment in individuals with major depressive symptoms than those with mild or no symptoms. | ( ; ; ; ) |
| 3) Consequences for daily life | • Risks pertain to privacy, confidentiality, and unintended consequences of disclosing personal health information • Misleading information or conflicts of interest, when the platforms promote popular content • Individuals have concerns about privacy, threats to employment, stigma and being judged, adverse impact on relationships and online hostility | ( ; ; ; ) |
Facilitate Social Interaction
Social media platforms offer near continuous opportunities to connect and interact with others, regardless of time of day or geographic location. This on demand ease of communication may be especially important for facilitating social interaction among individuals with mental disorders experiencing difficulties interacting in face-to-face settings. For example, impaired social functioning is a common deficit in schizophrenia spectrum disorders, and social media may facilitate communication and interacting with others for these individuals ( Torous & Keshavan, 2016 ). This was suggested in one study where participants with schizophrenia indicated that social media helped them to interact and socialize more easily ( Miller et al., 2015 ). Like other online communication, the ability to connect with others anonymously may be an important feature of social media, especially for individuals living with highly stigmatizing health conditions ( Berger, Wagner, & Baker, 2005 ), such as serious mental disorders ( Highton-Williamson, Priebe, & Giacco, 2015 ).
Studies have found that individuals with serious mental disorders ( Spinzy, Nitzan, Becker, Bloch, & Fennig, 2012 ) as well as young adults with mental illness ( Gowen, Deschaine, Gruttadara, & Markey, 2012 ) appear to form online relationships and connect with others on social media as often as social media users from the general population. This is an important observation because individuals living with serious mental disorders typically have few social contacts in the offline world, and also experience high rates of loneliness ( Badcock et al., 2015 ; Giacco, Palumbo, Strappelli, Catapano, & Priebe, 2016 ). Among individuals receiving publicly funded mental health services who use social media, nearly half (47%) reported using these platforms at least weekly to feel less alone ( Brusilovskiy, Townley, Snethen, & Salzer, 2016 ). In another study of young adults with serious mental illness, most indicated that they used social media to help feel less isolated ( Gowen et al., 2012 ). Interestingly, more frequent use of social media among a sample of individuals with serious mental illness was associated with greater community participation, measured as participation in shopping, work, religious activities or visiting friends and family, as well as greater civic engagement, reflected as voting in local elections ( Brusilovskiy et al., 2016 ).
Emerging research also shows that young people with moderate to severe depressive symptoms appear to prefer communicating on social media rather than in-person ( Rideout & Fox, 2018 ), while other studies have found that some individuals may prefer to seek help for mental health concerns online rather than through in-person encounters ( Batterham & Calear, 2017 ). In a qualitative study, participants with schizophrenia described greater anonymity, the ability to discover that other people have experienced similar health challenges, and reducing fears through greater access to information as important motivations for using the Internet to seek mental health information ( Schrank, Sibitz, Unger, & Amering, 2010 ). Because social media does not require the immediate responses necessary in face-to-face communication, it may overcome deficits with social interaction due to psychotic symptoms that typically adversely affect face-to-face conversations ( Docherty et al., 1996 ). Online social interactions may not require the use of non-verbal cues, particularly in the initial stages of interaction ( Kiesler, Siegel, & McGuire, 1984 ), with interactions being more fluid, and within the control of users, thereby overcoming possible social anxieties linked to in-person interaction ( Indian & Grieve, 2014 ). Furthermore, many individuals with serious mental disorders can experience symptoms including passive social withdrawal, blunted affect and attentional impairment, as well as active social avoidance due to hallucinations or other concerns ( Hansen, Torgalsbøen, Melle, & Bell, 2009 ); thus, potentially reinforcing the relative advantage, as perceived by users, of using social media over in person conversations.
Access to a Peer Support Network
There is growing recognition about the role that social media channels could play in enabling peer support ( Bucci et al., 2019 ; Naslund, Aschbrenner, et al., 2016b ), referred to as a system of mutual giving and receiving where individuals who have endured the difficulties of mental illness can offer hope, friendship, and support to others facing similar challenges ( Davidson, Chinman, Sells, & Rowe, 2006 ; Mead, Hilton, & Curtis, 2001 ). Initial studies exploring use of online self-help forums among individuals with serious mental illnesses have found that individuals with schizophrenia appeared to use these forums for self-disclosure, and sharing personal experiences, in addition to providing or requesting information, describing symptoms, or discussing medication ( Haker, Lauber, & Rössler, 2005 ), while users with bipolar disorder reported using these forums to ask for help from others about their illness ( Vayreda & Antaki, 2009 ). More recently, in a review of online social networking in people with psychosis, Highton-Williamson et al (2015) highlight that an important purpose of such online connections was to establish new friendships, pursue romantic relationships, maintain existing relationships or reconnect with people, and seek online peer support from others with lived experience ( Highton-Williamson et al., 2015 ).
Online peer support among individuals with mental illness has been further elaborated in various studies. In a content analysis of comments posted to YouTube by individuals who self-identified as having a serious mental illness, there appeared to be opportunities to feel less alone, provide hope, find support and learn through mutual reciprocity, and share coping strategies for day-to-day challenges of living with a mental illness ( Naslund, Grande, Aschbrenner, & Elwyn, 2014 ). In another study, Chang (2009) delineated various communication patterns in an online psychosis peer-support group ( Chang, 2009 ). Specifically, different forms of support emerged, including ‘informational support’ about medication use or contacting mental health providers, ‘esteem support’ involving positive comments for encouragement, ‘network support’ for sharing similar experiences, and ‘emotional support’ to express understanding of a peer’s situation and offer hope or confidence ( Chang, 2009 ). Bauer et al. (2013) reported that the main interest in online self-help forums for patients with bipolar disorder was to share emotions with others, allow exchange of information, and benefit by being part of an online social group ( Bauer, Bauer, Spiessl, & Kagerbauer, 2013 ).
For individuals who openly discuss mental health problems on Twitter, a study by Berry et al. (2017) found that this served as an important opportunity to seek support and to hear about the experiences of others ( Berry et al., 2017 ). In a survey of social media users with mental illness, respondents reported that sharing personal experiences about living with mental illness and opportunities to learn about strategies for coping with mental illness from others were important reasons for using social media ( Naslund et al., 2017 ). A computational study of mental health awareness campaigns on Twitter provides further support with inspirational posts and tips being the most shared ( Saha et al., 2019 ). Taken together, these studies offer insights about the potential for social media to facilitate access to an informal peer support network, though more research is necessary to examine how these online interactions may impact intentions to seek care, illness self-management, and clinically meaningful outcomes in offline contexts.
Promote Engagement and Retention in Services
Many individuals living with mental disorders have expressed interest in using social media platforms for seeking mental health information ( Lal, Nguyen, & Theriault, 2018 ), connecting with mental health providers ( M. L. Birnbaum et al., 2017 ), and accessing evidence-based mental health services delivered over social media specifically for coping with mental health symptoms or for promoting overall health and wellbeing ( Naslund et al., 2017 ). With the widespread use of social media among individuals living with mental illness combined with the potential to facilitate social interaction and connect with supportive peers, as summarized above, it may be possible to leverage the popular features of social media to enhance existing mental health programs and services. A recent review by Biagianti et al (2018) found that peer-to-peer support appeared to offer feasible and acceptable ways to augment digital mental health interventions for individuals with psychotic disorders by specifically improving engagement, compliance, and adherence to the interventions, and may also improve perceived social support ( Biagianti, Quraishi, & Schlosser, 2018 ).
Among digital programs that have incorporated peer-to-peer social networking consistent with popular features on social media platforms, a pilot study of the HORYZONS online psychosocial intervention demonstrated significant reductions in depression among patients with first episode psychosis ( Alvarez-Jimenez et al., 2013 ). Importantly, the majority of participants (95%) in this study engaged with the peer-to-peer networking feature of the program, with many reporting increases in perceived social connectedness and empowerment in their recovery process ( Alvarez-Jimenez et al., 2013 ). This moderated online social therapy program is now being evaluated as part of a large randomized controlled trial for maintaining treatment effects from first episode psychosis services ( Alvarez-Jimenez et al., 2019 ).
Other early efforts have demonstrated that use of digital environments with the interactive peer-to-peer features of social media can enhance social functioning and wellbeing in young people at high risk of psychosis ( Alvarez-Jimenez et al., 2018 ). There has also been a recent emergence of several mobile apps to support symptom monitoring and relapse prevention in psychotic disorders. Among these apps, the development of PRIME (Personalized Real-time Intervention for Motivational Enhancement) has involved working closely with young people with schizophrenia to ensure that the design of the app has the look and feel of mainstream social media platforms, as opposed to existing clinical tools ( Schlosser et al., 2016 ). This unique approach to the design of the app is aimed at promoting engagement, and ensuring that the app can effectively improve motivation and functioning through goal setting and promoting better quality of life of users with schizophrenia ( Schlosser et al., 2018 ).
Social media platforms could also be used to promote engagement and participation in in-person services delivered through community mental health settings. For example, the peer-based lifestyle intervention called PeerFIT targets weight loss and improved fitness among individuals living with serious mental illness through a combination of in-person lifestyle classes, exercise groups, and use of digital technologies ( Aschbrenner, Naslund, Shevenell, Kinney, & Bartels, 2016 ; Aschbrenner, Naslund, Shevenell, Mueser, & Bartels, 2016 ). The intervention holds tremendous promise as lack of support is one of the largest barriers toward exercise in patients with serious mental illness ( Firth et al., 2016 ) and it is now possible to use social media to counter such. Specifically, in PeerFIT, a private Facebook group is closely integrated into the program to offer a closed platform where participants can connect with the lifestyle coaches, access intervention content, and support or encourage each other as they work towards their lifestyle goals ( Aschbrenner, Naslund, & Bartels, 2016 ; Naslund, Aschbrenner, Marsch, & Bartels, 2016a ). To date, this program has demonstrate preliminary effectiveness for meaningfully reducing cardiovascular risk factors that contribute to early mortality in this patient group ( Aschbrenner, Naslund, Shevenell, Kinney, et al., 2016 ), while the Facebook component appears to have increased engagement in the program, while allowing participants who were unable to attend in-person sessions due to other health concerns or competing demands to remain connected with the program ( Naslund, Aschbrenner, Marsch, McHugo, & Bartels, 2018 ). This lifestyle intervention is currently being evaluated in a randomized controlled trial enrolling young adults with serious mental illness from a variety of real world community mental health services settings ( Aschbrenner, Naslund, Gorin, et al., 2018 ).
These examples highlight the promise of incorporating the features of popular social media into existing programs, which may offer opportunities to safely promote engagement and program retention, while achieving improved clinical outcomes. This is an emerging area of research, as evidenced by several important effectiveness trials underway ( Alvarez-Jimenez et al., 2019 ; Aschbrenner, Naslund, Gorin, et al., 2018 ), including efforts to leverage online social networking to support family caregivers of individuals receiving first episode psychosis services ( Gleeson et al., 2017 ).
Challenges with Social Media for Mental Health
The science on the role of social media for engaging persons with mental disorders needs a cautionary note on the effects of social media usage on mental health and well being, particularly in adolescents and young adults. While the risks and harms of social media are frequently covered in the popular press and mainstream news reports, careful consideration of the research in this area is necessary. In a review of 43 studies in young people, many benefits of social media were cited, including increased self-esteem, and opportunities for self-disclosure ( Best, Manktelow, & Taylor, 2014 ). Yet, reported negative effects were an increased exposure to harm, social isolation, depressive symptoms and bullying ( Best et al., 2014 ). In the sections that follow (see Table 1 for a summary), we consider three major categories of risk related to use of social media and mental health. These include: 1) Impact on symptoms; 2) Facing hostile interactions; and 3) Consequences for daily life.
Impact on Symptoms
Studies consistently highlight that use of social media, especially heavy use and prolonged time spent on social media platforms, appears to contribute to increased risk for a variety of mental health symptoms and poor wellbeing, especially among young people ( Andreassen et al., 2016 ; Kross et al., 2013 ; Woods & Scott, 2016 ). This may partly be driven by the detrimental effects of screen time on mental health, including increased severity of anxiety and depressive symptoms, which have been well documented ( Stiglic & Viner, 2019 ). Recent studies have reported negative effects of social media use on mental health of young people, including social comparison pressure with others and greater feeling of social isolation after being rejected by others on social media ( Rideout & Fox, 2018 ). In a study of young adults, it was found that negative comparisons with others on Facebook contributed to risk of rumination and subsequent increases in depression symptoms ( Feinstein et al., 2013 ). Still, the cross sectional nature of many screen time and mental health studies makes it challenging to reach causal inferences ( Orben & Przybylski, 2019 ).
Quantity of social media use is also an important factor, as highlighted in a survey of young adults ages 19 to 32, where more frequent visits to social media platforms each week were correlated with greater depressive symptoms ( Lin et al., 2016 ). More time spent using social media is also associated with greater symptoms of anxiety ( Vannucci, Flannery, & Ohannessian, 2017 ). The actual number of platforms accessed also appears to contribute to risk as reflected in another national survey of young adults where use of a large number of social media platforms was associated with negative impact on mental health ( Primack et al., 2017 ). Among survey respondents using between 7 and 11 different social media platforms compared to respondents using only 2 or fewer platforms, there was a 3 times greater odds of having high levels of depressive symptoms and a 3.2 times greater odds of having high levels of anxiety symptoms ( Primack et al., 2017 ).
Many researchers have postulated that worsening mental health attributed to social media use may be because social media replaces face-to-face interactions for young people ( Twenge & Campbell, 2018 ), and may contribute to greater loneliness ( Bucci et al., 2019 ), and negative effects on other aspects of health and wellbeing ( Woods & Scott, 2016 ). One nationally representative survey of US adolescents found that among respondents who reported more time accessing media such as social media platforms or smartphone devices, there was significantly greater depressive symptoms and increased risk of suicide when compared to adolescents who reported spending more time on non-screen activities, such as in-person social interaction or sports and recreation activities ( Twenge, Joiner, Rogers, & Martin, 2018 ). For individuals living with more severe mental illnesses, the effects of social media on psychiatric symptoms have received less attention. One study found that participation in chat rooms may contribute to worsening symptoms in young people with psychotic disorders ( Mittal, Tessner, & Walker, 2007 ), while another study of patients with psychosis found that social media use appeared to predict low mood ( Berry, Emsley, Lobban, & Bucci, 2018 ). These studies highlight a clear relationship between social media use and mental health that may not be present in general population studies ( Orben & Przybylski, 2019 ), and emphasize the need to explore how social media may contribute to symptom severity and whether protective factors may be identified to mitigate these risks.
Facing Hostile Interactions
Popular social media platforms can create potential situations where individuals may be victimized by negative comments or posts. Cyberbullying represents a form of online aggression directed towards specific individuals, such as peers or acquaintances, which is perceived to be most harmful when compared to random hostile comments posted online ( Hamm et al., 2015 ). Importantly, cyberbullying on social media consistently shows harmful impact on mental health in the form of increased depressive symptoms as well as worsening of anxiety symptoms, as evidenced in a review of 36 studies among children and young people ( Hamm et al., 2015 ). Furthermore, cyberbullying disproportionately impacts females as reflected in a national survey of adolescents in the United States, where females were twice as likely to be victims of cyberbullying compared to males ( Alhajji, Bass, & Dai, 2019 ). Most studies report cross-sectional associations between cyberbullying and symptoms of depression or anxiety ( Hamm et al., 2015 ), though one longitudinal study in Switzerland found that cyberbullying contributed to significantly greater depression over time ( Machmutow, Perren, Sticca, & Alsaker, 2012 ).
For youth ages 10 to 17 who reported major depressive symptomatology, there was over 3 times greater odds of facing online harassment in the last year compared to youth who reported mild or no depressive symptoms ( Ybarra, 2004 ). Similarly, in a 2018 national survey of young people, respondents ages 14 to 22 with moderate to severe depressive symptoms were more likely to have had negative experiences when using social media, and in particular, were more likely to report having faced hostile comments, or being “trolled”, from others when compared to respondents without depressive symptoms (31% vs. 14%) ( Rideout & Fox, 2018 ). As these studies depict risks for victimization on social media and the correlation with poor mental health, it is possible that individuals living with mental illness may also experience greater hostility online compared to individuals without mental illness. This would be consistent with research showing greater risk of hostility, including increased violence and discrimination, directed towards individuals living with mental illness in in-person contexts, especially targeted at those with severe mental illnesses ( Goodman et al., 1999 ).
A computational study of mental health awareness campaigns on Twitter reported that while stigmatizing content was rare, it was actually the most spread (re-tweeted) demonstrating that harmful content can travel quickly on social media ( Saha et al., 2019 ). Another study was able to map the spread of social media posts about the Blue Whale Challenge, an alleged game promoting suicide, over Twitter, YouTube, Reddit, Tumblr and other forums across 127 countries ( Sumner et al., 2019 ). These findings show that it is critical to monitor the actual content of social media posts, such as determining whether content is hostile or promotes harm to self or others. This is pertinent because existing research looking at duration of exposure cannot account for the impact of specific types of content on mental health and is insufficient to fully understand the effects of using these platforms on mental health.
Consequences for Daily Life
The ways in which individuals use social media can also impact their offline relationships and everyday activities. To date, reports have described risks of social media use pertaining to privacy, confidentiality, and unintended consequences of disclosing personal health information online ( Torous & Keshavan, 2016 ). Additionally, concerns have been raised about poor quality or misleading health information shared on social media, and that social media users may not be aware of misleading information or conflicts of interest especially when the platforms promote popular content regardless of whether it is from a trustworthy source ( Moorhead et al., 2013 ; Ventola, 2014 ). For persons living with mental illness there may be additional risks from using social media. A recent study that specifically explored the perspectives of social media users with serious mental illnesses, including participants with schizophrenia spectrum disorders, bipolar disorder, or major depression, found that over one third of participants expressed concerns about privacy when using social media ( Naslund & Aschbrenner, 2019 ). The reported risks of social media use were directly related to many aspects of everyday life, including concerns about threats to employment, fear of stigma and being judged, impact on personal relationships, and facing hostility or being hurt ( Naslund & Aschbrenner, 2019 ). While few studies have specifically explored the dangers of social media use from the perspectives of individuals living with mental illness, it is important to recognize that use of these platforms may contribute to risks that extend beyond worsening symptoms and that can affect different aspects of daily life.
In this commentary we considered ways in which social media may yield benefits for individuals living with mental illness, while contrasting these with the possible harms. Studies reporting on the threats of social media for individuals with mental illness are mostly cross-sectional, making it difficult to draw conclusions about direction of causation. However, the risks are potentially serious. These risks should be carefully considered in discussions pertaining to use of social media and the broader use of digital mental health technologies, as avenues for mental health promotion, or for supporting access to evidence-based programs or mental health services. At this point, it would be premature to view the benefits of social media as outweighing the possible harms, when it is clear from the studies summarized here that social media use can have negative effects on mental health symptoms, can potentially expose individuals to hurtful content and hostile interactions, and can result in serious consequences for daily life, including threats to employment and personal relationships. Despite these risks, it is also necessary to recognize that individuals with mental illness will continue to use social media given the ease of accessing these platforms and the immense popularity of online social networking. With this in mind, it may be ideal to raise awareness about these possible risks so that individuals can implement necessary safeguards, while also highlighting that there could also be benefits. For individuals with mental illness who use social media, being aware of the risks is an essential first step, and then highlighting ways that use of these popular platforms could also contribute to some benefits, ranging from finding meaningful interactions with others, engaging with peer support networks, and accessing information and services.
To capitalize on the widespread use of social media, and to achieve the promise that these platforms may hold for supporting the delivery of targeted mental health interventions, there is need for continued research to better understand how individuals living with mental illness use social media. Such efforts could inform safety measures and also encourage use of social media in ways that maximize potential benefits while minimizing risk of harm. It will be important to recognize how gender and race contribute to differences in use of social media for seeking mental health information or accessing interventions, as well as differences in how social media might impact mental wellbeing. For example, a national survey of 14- to 22-year olds in the United States found that female respondents were more likely to search online for information about depression or anxiety, and to try to connect with other people online who share similar mental health concerns, when compared to male respondents ( Rideout & Fox, 2018 ). In the same survey, there did not appear to be any differences between racial or ethnic groups in social media use for seeking mental health information ( Rideout & Fox, 2018 ). Social media use also appears to have a differential impact on mental health and emotional wellbeing between females and males ( Booker, Kelly, & Sacker, 2018 ), highlighting the need to explore unique experiences between gender groups to inform tailored programs and services. Research shows that lesbian, gay, bisexual or transgender individuals frequently use social media for searching for health information and may be more likely compared to heterosexual individuals to share their own personal health experiences with others online ( Rideout & Fox, 2018 ). Less is known about use of social media for seeking support for mental health concerns among gender minorities, though this is an important area for further investigation as these individuals are more likely to experience mental health problems and more likely to experience online victimization when compared to heterosexual individuals ( Mereish, Sheskier, Hawthorne, & Goldbach, 2019 ).
Similarly, efforts are needed to explore the relationship between social media use and mental health among ethnic and racial minorities. A recent study found that exposure to traumatic online content on social media showing violence or hateful posts directed at racial minorities contributed to increases in psychological distress, PTSD symptoms, and depression among African American and Latinx adolescents in the United States ( Tynes, Willis, Stewart, & Hamilton, 2019 ). These concerns are contrasted by growing interest in the potential for new technologies including social media to expand the reach of services to underrepresented minority groups ( Schueller, Hunter, Figueroa, & Aguilera, 2019 ). Therefore, greater attention is needed to understanding the perspectives of ethnic and racial minorities to inform effective and safe use of social media for mental health promotion efforts.
Research has found that individuals living with mental illness have expressed interest in accessing mental health services through social media platforms. A survey of social media users with mental illness found that most respondents were interested in accessing programs for mental health on social media targeting symptom management, health promotion, and support for communicating with health care providers and interacting with the health system ( Naslund et al., 2017 ). Importantly, individuals with serious mental illness have also emphasized that any mental health intervention on social media would need to be moderated by someone with adequate training and credentials, would need to have ground rules and ways to promote safety and minimize risks, and importantly, would need to be free and easy to access.
An important strength with this commentary is that it combines a range of studies broadly covering the topic of social media and mental health. We have provided a summary of recent evidence in a rapidly advancing field with the goal of presenting unique ways that social media could offer benefits for individuals with mental illness, while also acknowledging the potentially serious risks and the need for further investigation. There are also several limitations with this commentary that warrant consideration. Importantly, as we aimed to address this broad objective, we did not conduct a systematic review of the literature. Therefore, the studies reported here are not exhaustive, and there may be additional relevant studies that were not included. Additionally, we only summarized published studies, and as a result, any reports from the private sector or websites from different organizations using social media or other apps containing social media-like features would have been omitted. Though it is difficult to rigorously summarize work from the private sector, sometimes referred to as “gray literature”, because many of these projects are unpublished and are likely selective in their reporting of findings given the target audience may be shareholders or consumers.
Another notable limitation is that we did not assess risk of bias in the studies summarized in this commentary. We found many studies that highlighted risks associated with social media use for individuals living with mental illness; however, few studies of programs or interventions reported negative findings, suggesting the possibility that negative findings may go unpublished. This concern highlights the need for a future more rigorous review of the literature with careful consideration of bias and an accompanying quality assessment. Most of the studies that we described were from the United States, as well as from other higher income settings such as Australia or the United Kingdom. Despite the global reach of social media platforms, there is a dearth of research on the impact of these platforms on the mental health of individuals in diverse settings, as well as the ways in which social media could support mental health services in lower income countries where there is virtually no access to mental health providers. Future research is necessary to explore the opportunities and risks for social media to support mental health promotion in low-income and middle-income countries, especially as these countries face a disproportionate share of the global burden of mental disorders, yet account for the majority of social media users worldwide ( Naslund et al., 2019 ).
Future Directions for Social Media and Mental Health
As we consider future research directions, the near ubiquitous social media use also yields new opportunities to study the onset and manifestation of mental health symptoms and illness severity earlier than traditional clinical assessments. There is an emerging field of research referred to as ‘digital phenotyping’ aimed at capturing how individuals interact with their digital devices, including social media platforms, in order to study patterns of illness and identify optimal time points for intervention ( Jain, Powers, Hawkins, & Brownstein, 2015 ; Onnela & Rauch, 2016 ). Given that most people access social media via mobile devices, digital phenotyping and social media are closely related ( Torous et al., 2019 ). To date, the emergence of machine learning, a powerful computational method involving statistical and mathematical algorithms ( Shatte, Hutchinson, & Teague, 2019 ), has made it possible to study large quantities of data captured from popular social media platforms such as Twitter or Instagram to illuminate various features of mental health ( Manikonda & De Choudhury, 2017 ; Reece et al., 2017 ). Specifically, conversations on Twitter have been analyzed to characterize the onset of depression ( De Choudhury, Gamon, Counts, & Horvitz, 2013 ) as well as detecting users’ mood and affective states ( De Choudhury, Gamon, & Counts, 2012 ), while photos posted to Instagram can yield insights for predicting depression ( Reece & Danforth, 2017 ). The intersection of social media and digital phenotyping will likely add new levels of context to social media use in the near future.
Several studies have also demonstrated that when compared to a control group, Twitter users with a self-disclosed diagnosis of schizophrenia show unique online communication patterns ( Michael L Birnbaum, Ernala, Rizvi, De Choudhury, & Kane, 2017 ), including more frequent discussion of tobacco use ( Hswen et al., 2017 ), symptoms of depression and anxiety ( Hswen, Naslund, Brownstein, & Hawkins, 2018b ), and suicide ( Hswen, Naslund, Brownstein, & Hawkins, 2018a ). Another study found that online disclosures about mental illness appeared beneficial as reflected by fewer posts about symptoms following self-disclosure (Ernala, Rizvi, Birnbaum, Kane, & De Choudhury, 2017). Each of these examples offers early insights into the potential to leverage widely available online data for better understanding the onset and course of mental illness. It is possible that social media data could be used to supplement additional digital data, such as continuous monitoring using smartphone apps or smart watches, to generate a more comprehensive ‘digital phenotype’ to predict relapse and identify high-risk health behaviors among individuals living with mental illness ( Torous et al., 2019 ).
With research increasingly showing the valuable insights that social media data can yield about mental health states, greater attention to the ethical concerns with using individual data in this way is necessary ( Chancellor, Birnbaum, Caine, Silenzio, & De Choudhury, 2019 ). For instance, data is typically captured from social media platforms without the consent or awareness of users ( Bidargaddi et al., 2017 ), which is especially crucial when the data relates to a socially stigmatizing health condition such as mental illness ( Guntuku, Yaden, Kern, Ungar, & Eichstaedt, 2017 ). Precautions are needed to ensure that data is not made identifiable in ways that were not originally intended by the user who posted the content, as this could place an individual at risk of harm or divulge sensitive health information ( Webb et al., 2017 ; Williams, Burnap, & Sloan, 2017 ). Promising approaches for minimizing these risks include supporting the participation of individuals with expertise in privacy, clinicians, as well as the target individuals with mental illness throughout the collection of data, development of predictive algorithms, and interpretation of findings ( Chancellor et al., 2019 ).
In recognizing that many individuals living with mental illness use social media to search for information about their mental health, it is possible that they may also want to ask their clinicians about what they find online to check if the information is reliable and trustworthy. Alternatively, many individuals may feel embarrassed or reluctant to talk to their clinicians about using social media to find mental health information out of concerns of being judged or dismissed. Therefore, mental health clinicians may be ideally positioned to talk with their patients about using social media, and offer recommendations to promote safe use of these sites, while also respecting their patients’ autonomy and personal motivations for using these popular platforms. Given the gap in clinical knowledge about the impact of social media on mental health, clinicians should be aware of the many potential risks so that they can inform their patients, while remaining open to the possibility that their patients may also experience benefits through use of these platforms. As awareness of these risks grows, it may be possible that new protections will be put in place by industry or through new policies that will make the social media environment safer. It is hard to estimate a number needed to treat or harm today given the nascent state of research, which means the patient and clinician need to weigh the choice on a personal level. Thus offering education and information is an important first step in that process. As patients increasingly show interest in accessing mental health information or services through social media, it will be necessary for health systems to recognize social media as a potential avenue for reaching or offering support to patients. This aligns with growing emphasis on the need for greater integration of digital psychiatry, including apps, smartphones, or wearable devices, into patient care and clinical services through institution-wide initiatives and training clinical providers ( Hilty, Chan, Torous, Luo, & Boland, 2019 ). Within a learning healthcare environment where research and care are tightly intertwined and feedback between both is rapid, the integration of digital technologies into services may create new opportunities for advancing use of social media for mental health.
As highlighted in this commentary, social media has become an important part of the lives of many individuals living with mental disorders. Many of these individuals use social media to share their lived experiences with mental illness, to seek support from others, and to search for information about treatment recommendations, accessing mental health services, and coping with symptoms ( Bucci et al., 2019 ; Highton-Williamson et al., 2015 ; Naslund, Aschbrenner, et al., 2016b ). As the field of digital mental health advances, the wide reach, ease of access, and popularity of social media platforms could be used to allow individuals in need of mental health services or facing challenges of mental illness to access evidence-based treatment and support. To achieve this end and to explore whether social media platforms can advance efforts to close the gap in available mental health services in the United States and globally, it will be essential for researchers to work closely with clinicians and with those affected by mental illness to ensure that possible benefits of using social media are carefully weighed against anticipated risks.
Acknowledgements
Dr. Naslund is supported by a grant from the National Institute of Mental Health (U19MH113211). Dr. Aschbrenner is supported by a grant from the National Institute of Mental Health (1R01MH110965-01).
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest
The authors have nothing to disclose.
- Abdel-Baki A, Lai S, D.-Charron O, Stip E, & Kara N, (2017). Understanding access and use of technology among youth with first - episode psychosis to inform the development of technology - enabled therapeutic interventions . Early intervention in psychiatry , 77 ( 1 ), 72–76. [ PubMed ] [ Google Scholar ]
- Ahmed YA, Ahmad MN, Ahmad N, & Zakaria NH (2019). Social media for knowledge-sharing: A systematic literature review . Telematics and informatics , 37 , 72–112 . [ Google Scholar ]
- Alhajji M, Bass S, & Dai T (2019). Cyberbullying, mental health, and violence in adolescents and associations with sex and race: data from the 2015 Youth Risk Behavior Survey . Global pediatric health , 6 , 2333794X19868887. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alvarez-Jimenez M, Bendall S, Koval P, Rice S, Cagliarini D, Valentine L, … Penn DL (2019). HORYZONS trial: protocol for a randomised controlled trial of a moderated online social therapy to maintain treatment effects from first-episode psychosis services . BMJ open , 9 ( 2 ), e024104. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alvarez-Jimenez M, Bendall S, Lederman R, Wadley G, Chinnery G, Vargas S, … Gleeson JF (2013). On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis . Schizophrenia research , 143 ( 1 ), 143–149. [ PubMed ] [ Google Scholar ]
- Alvarez-Jimenez M, Gleeson J, Bendall S, Penn D, Yung A, Ryan R, … Miles C (2018). Enhancing social functioning in young people at Ultra High Risk (UHR) for psychosis: A pilot study of a novel strengths and mindfulness-based online social therapy . Schizophrenia research , 202 , 369–377. [ PubMed ] [ Google Scholar ]
- Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, & Pallesen S (2016). The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study . Psychology of Addictive Behaviors , 30 ( 2 ), 252. [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, & Bartels SJ (2016). A mixed methods study of peer-to-peer support in a group-based lifestyle intervention for adults with serious mental illness . Psychiatric rehabilitation journal , 39 ( 4 ), 328. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Gorin AA, Mueser KT, Scherer EA, Viron M, … Bartels SJ, (2018). Peer support and mobile health technology targeting obesity-related cardiovascular risk in young adults with serious mental illness: Protocol for a randomized controlled trial . Contemporary clinical trials , 74 , 97–106. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Grinley T, Bienvenida JCM, Bartels SJ, & Brunette M (2018). A Survey of Online and Mobile Technology Use at Peer Support Agencies . Psychiatric Quarterly , 1–10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Shevenell M, Kinney E, & Bartels SJ (2016). A pilot study of a peer-group lifestyle intervention enhanced with mHealth technology and social media for adults with serious mental illness . The Journal of nervous and mental disease , 204 ( 6 ), 483–486. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Shevenell M, Mueser KT, & Bartels SJ (2016). Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness . Psychiatric Quarterly , 57 ( 3 ), 401–415. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aschbrenner KA, Naslund JA, Tomlinson EF, Kinney A, Pratt SI, & Brunette MF (2019). Adolescents’ Use of Digital Technologies and Preferences for Mobile Health Coaching in Mental Health Settings . Frontiers in Public Health . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Badcock JC, Shah S, Mackinnon A, Stain HJ, Galletly C, Jablensky A, & Morgan VA (2015). Loneliness in psychotic disorders and its association with cognitive function and symptom profile . Schizophrenia research , 169 ( 1-3 ), 268–273. [ PubMed ] [ Google Scholar ]
- Batterham PJ, & Calear AJ (2017). Preferences for internet-based mental health interventions in an adult online sample: Findings from ann online community survey . JMIR mental health , 4 ( 2 ), e26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bauer R, Bauer M, Spiessl H, & Kagerbauer T (2013). Cyber-support: an analysis of online self-help forums (online self-help forums in bipolar disorder) . Nordic journal of psychiatry , 67 ( 3 ), 185–190. [ PubMed ] [ Google Scholar ]
- Berger M, Wagner TH, & Baker LC (2005). Internet use and stigmatized illness . Social science & medicine , 67 ( 8 ), 1821–1827. [ PubMed ] [ Google Scholar ]
- Berry N, Emsley R, Lobban F, & Bucci S (2018). Social media and its relationship with mood, self - esteem and paranoia in psychosis . Acta Psychiatrica Scandinavica , 138 , 558–570. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berry N, Lobban F, Belousov M, Emsley R, Nenadic G, & Bucci S (2017). # Why We Tweet MH: understanding why people use Twitter to discuss mental health problems . Journal of medical Internet research , 19 ( 4 ), e107. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Best P, Manktelow R, & Taylor B (2014). Online communication, social media and adolescent wellbeing: A systematic narrative review . Children and Youth Services Review , 41 , 27–36. [ Google Scholar ]
- Biagianti B, Quraishi SH, & Schlosser DA (2018). Potential benefits of incorporating peer-to-peer interactions into digital interventions for psychotic disorders: a systematic review . Psychiatric Services , 69 ( 4 ), 377–388. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bidargaddi N, Musiat P, Makinen V-P, Ermes M, Schrader G, & Licinio J (2017). Digital footprints: facilitating large-scale environmental psychiatric research in naturalistic settings through data from everyday technologies . Molecular psychiatry , 22 ( 2 ), 164. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Birnbaum ML, Emala SK, Rizvi AF, De Choudhury M, & Kane JM (2017). A Collaborative Approach to Identifying Social Media Markers of Schizophrenia by Employing Machine Learning and Clinical Appraisals . Journal of medical Internet research , 79 ( 8 ), e289. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Birnbaum ML, Rizvi AF, Correll CU, Kane JM, & Confino J (2017). Role of social media and the Internet in pathways to care for adolescents and young adults with psychotic disorders and non - psychotic mood disorders . Early intervention in psychiatry , 77 ( 4 ), 290–295. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Booker CL, Kelly YJ, & Sacker A (2018). Gender differences in the associations between age trends of social media interaction and well-being among 10-15 year olds in the UK . BMC public health , 18 ( 1 ), 321. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brunette M, Achtyes E, Pratt S, Stilwell K, Opperman M, Guarino S, & Kay-Lambkin F (2019). Use of smartphones, computers and social media among people with SMI: opportunity for intervention . Community mental health journal , 1–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brusilovskiy E, Townley G, Snethen G, & Salzer MS (2016). Social media use, community participation and psychological well-being among individuals with serious mental illnesses . Computers in Human Behavior , 65 , 232–240. [ Google Scholar ]
- Bucci S, Schwannauer M, & Berry N (2019). The digital revolution and its impact on mental health care . Psychology and Psychotherapy: Theory, Research and Practice , 1–21. [ PubMed ] [ Google Scholar ]
- Chancellor S, Birnbaum ML, Caine ED, Silenzio V, & De Choudhury M (2019). A taxonomy of ethical tensions in inferring mental health states from social media . Paper presented at the Proceedings of the Conference on Fairness, Accountability, and Transparency. [ Google Scholar ]
- Chang HJ (2009). Online supportive interactions: Using a network approach to examine communication patterns within a psychosis social support group in Taiwan . Journal of the American Society for Information Science and Technology , 60 ( 7 ), 1504–1517. [ Google Scholar ]
- Davidson L, Chinman M, Sells D, & Rowe M (2006). Peer support among adults with serious mental illness: a report from the field . Schizophrenia bulletin , 32 ( 3 ), 443–450. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- De Choudhury M, Gamon M, & Counts S (2012). Happy, nervous or surprised? classification of human affective states in social media . Paper presented at the Sixth International AAAI Conference on Weblogs and Social Media. [ Google Scholar ]
- De Choudhury M, Gamon M, Counts S, & Horvitz E (2013). Predicting Depression via Social Media . Paper presented at the Association for the Advancement of Artificial Intelligence. [ Google Scholar ]
- Docherty NM, Hawkins KA, Hoffman RE, Quinlan DM, Rakfeldt J, & Sledge WH (1996). Working memory, attention, and communication disturbances in schizophrenia . Journal of Abnormal Psychology , 105 ( 2 ), 212. [ PubMed ] [ Google Scholar ]
- Emala SK, Rizvi AF, Birnbaum ML, Kane JM, & De Choudhury M (2017). Linguistic Markers Indicating Therapeutic Outcomes of Social Media Disclosures of Schizophrenia . Proc. ACMHum.-Comput. Interact , 1 ( 1 ), 43. [ Google Scholar ]
- Feinstein BA, Hershenberg R, Bhatia V, Latack JA, Meuwly N, & Davila J (2013). Negative social comparison on Facebook and depressive symptoms: Rumination as a mechanism . Psychology of Popular Media Culture , 2 ( 3 ), 161. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, & Yung AR (2015). Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies . Schizophrenia bulletin , 42 ( 2 ), 448–455. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, & Vancampfort D (2016). Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis . Psychological medicine , 46 ( 14 ), 2869–2881. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gay K, Torous J, Joseph A, Pandya A, & Duckworth K (2016). Digital technology use among individuals with schizophrenia: results of an online survey . JMIR mental health , 3 ( 2 ), el5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Giacco D, Palumbo C, Strappelli N, Catapano F, & Priebe S (2016). Social contacts and loneliness in people with psychotic and mood disorders . Comprehensive Psychiatry , 66 , 59–66. [ PubMed ] [ Google Scholar ]
- Gleeson J, Lederman R, Herrman H, Koval P, Eleftheriadis D, Bendall S, … Alvarez-Jimenez M (2017). Moderated online social therapy for carers of young people recovering from first-episode psychosis: study protocol for a randomised controlled trial . Trials , 75 ( 1 ), 27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Glick G, Druss B, Pina J, Lally C, & Conde M (2016). Use of mobile technology in a community mental health setting . Journal of telemedicine and telecare , 22 ( 7 ), 430–435. [ PubMed ] [ Google Scholar ]
- Goodman LA, Thompson KM, Weinfurt K, Corl S, Acker P, Mueser KT, & Rosenberg SD (1999). Reliability of reports of violent victimization and posttraumatic stress disorder among men and women with serious mental illness . Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies , 12 ( 4 ), 587–599. [ PubMed ] [ Google Scholar ]
- Gowen K, Deschaine M, Gruttadara D, & Markey D (2012). Young adults with mental health conditions and social networking websites: seeking tools to build community . Psychiatric rehabilitation journal , 35 ( 3 ), 245–250. [ PubMed ] [ Google Scholar ]
- Guntuku SC, Yaden DB, Kern ML, Ungar LH, & Eichstaedt JC (2017). Detecting depression and mental illness on social media: an integrative review . Current Opinion in Behavioral Sciences , 18 , 43–49. [ Google Scholar ]
- Haker EL, Lauber C, & Rossler W (2005). Internet forums: a self - help approach for individuals with schizophrenia? Acta Psychiatrica Scandinavica , 112 ( 6 ), 474–477. [ PubMed ] [ Google Scholar ]
- Hamm MP, Newton AS, Chisholm A, Shulhan J, Milne A, Sundar P, … Hartling L (2015). Prevalence and effect of cyberbullying on children and young people: A scoping review of social media studies . JAMA pediatrics , 769 ( 8 ), 770–777. [ PubMed ] [ Google Scholar ]
- Hansen CF, Torgalsboen A-K, Melle I, & Bell MD (2009). Passive/apathetic social withdrawal and active social avoidance in schizophrenia: difference in underlying psychological processes . The Journal of nervous and mental disease , 197 ( 4 ), 274–277. [ PubMed ] [ Google Scholar ]
- Highton-Williamson E, Priebe S, & Giacco D (2015). Online social networking in people with psychosis: a systematic review . International Journal of Social Psychiatry , 61 ( 1 ), 92–101. [ PubMed ] [ Google Scholar ]
- Hilty DM, Chan S, Torous J, Luo J, & Boland RJ (2019). Mobile health, smartphone/device, and apps for psychiatry and medicine: competencies, training, and faculty development issues . Psychiatric Clinics , 42 ( 2 ), 513–534. [ PubMed ] [ Google Scholar ]
- Hswen Y, Naslund JA, Brownstein JS, & Hawkins JB (2018a). Monitoring online discussions about suicide among Twitter users with schizophrenia: exploratory study . JMIR mental health , 5 ( 4 ), e11483. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hswen Y, Naslund JA, Brownstein JS, & Hawkins JB (2018b). Online communication about depression and anxiety among twitter users with schizophrenia: preliminary findings to inform a digital phenotype using social media . Psychiatric Quarterly , 89 ( 3 ), 569–580. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hswen Y, Naslund JA, Chandrashekar P, Siegel R, Brownstein JS, & Hawkins JB (2017). Exploring online communication about cigarette smoking among Twitter users who self-identify as having schizophrenia . Psychiatry research , 257 , 479–484. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Indian M, & Grieve R (2014). When Facebook is easier than face-to-face: social support dervied from Facebook in socially anxious individuals . Personality and Individual Differences , 59 , 102–106. [ Google Scholar ]
- Jain SH, Powers BW, Hawkins JB, & Brownstein JS (2015). The digital phenotype . Nature Biotechnology , 33 ( 5 ), 462. [ PubMed ] [ Google Scholar ]
- Kiesler S, Siegel J, & McGuire TW (1984). Social psychological aspects of computer-mediated communication . American Psychologist , 39 , 1123–1134. [ Google Scholar ]
- Kross E, Verduyn P, Demiralp E, Park J, Lee DS, Lin N, … Ybarra O (2013). Facebook use predicts declines in subjective well-being in young adults . PloS one , 5 ( 8 ), e69841. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lai S, Nguyen V, & Theriault J (2018). Seeking mental health information and support online: experiences and perspectives of young people receiving treatment for first - episode psychosis . Early intervention in psychiatry , 72 ( 3 ), 324–330. [ PubMed ] [ Google Scholar ]
- Lin LY, Sidani JE, Shensa A, Radovic A, Miller E, Colditz JB, … Primack BA (2016). Association between social media use and depression among US young adults . Depression and anxiety , 22 ( 4 ), 323–331. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Machmutow K, Perren S, Sticca F, & Alsaker FD (2012). Peer victimisation and depressive symptoms: can specific coping strategies buffer the negative impact of cybervictimisation? Emotional and Behavioural Difficulties , 17 ( 3-4 ), 403–420. [ Google Scholar ]
- Manikonda L, & De Choudhury M (2017). Modeling and understanding visual attributes of mental health disclosures in social media . Paper presented at the Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems. [ Google Scholar ]
- Mead S, Hilton D, & Curtis L (2001). Peer support: A theoretical perspective . Psychiatric rehabilitation journal , 25 ( 2 ), 134. [ PubMed ] [ Google Scholar ]
- Mereish EH, Sheskier M, Hawthorne DJ, & Goldbach JT (2019). Sexual orientation disparities in mental health and substance use among Black American young people in the USA: effects of cyber and bias-based victimisation . Culture, health & sexuality , 21 ( 9 ), 985–998. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miller BJ, Stewart A, Schrimsher J, Peeples D, & Buckley PF (2015). How connected are people with schizophrenia? Cell phone, computer, email, and social media use . Psychiatry research , 225 ( 3 ), 458–463. [ PubMed ] [ Google Scholar ]
- Mittal VA, Tessner KD, & Walker EF (2007). Elevated social Internet use and schizotypal personality disorder in adolescents . Schizophrenia research , 94 ( 1-3 ), 50–57. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, & Hoving C (2013). A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication . Journal of medical Internet research , 15 ( 4 ), e85. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, & Aschbrenner KA (2019). Risks to privacy with use of social media: understanding the views of social media users with serious mental illness . Psychiatric Services , appi. ps. 201800520. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, & Bartels SJ (2016). How people living with serious mental illness use smartphones, mobile apps, and social media . Psychiatric rehabilitation journal , 39 ( 4 ), 364–367. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, Marsch LA, & Bartels SJ (2016a). Feasibility and acceptability of Facebook for health promotion among people with serious mental illness . Digital health , 2 , 2055207616654822. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, Marsch LA, & Bartels SJ (2016b). The future of mental health care: peer-to-peer support and social media . Epidemiology and Psychiatric Sciences , 25 ( 2 ), 113–122. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, Marsch LA, McHugo GJ, & Bartels SJ (2018). Facebook for supporting a lifestyle intervention for people with major depressive disorder, bipolar disorder, and schizophrenia: an exploratory study . Psychiatric Quarterly , 59 ( 1 ), 81–94. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Aschbrenner KA, McHugo GJ, Unutzer J, Marsch LA, & Bartels SJ (2017). Exploring opportunities to support mental health care using social media: A survey of social media users with mental illness . Early intervention in psychiatry . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Gonsalves PP, Gruebner O, Pendse SR, Smith SL, Sharma A, & Raviola G (2019). Digital innovations for global mental health: opportunities for data science, task sharing, and early intervention . Current Treatment Options in Psychiatry , 1–15. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Naslund JA, Grande SW, Aschbrenner KA, & Elwyn G (2014). Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube . PloS one , 9 ( 10 ), e110171. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Onnela J-P, & Rauch SL (2016). Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health . Neuropsychopharmacology , 41 ( 7 ), 1691. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Orben A, & Przybylski AK (2019). The association between adolescent well-being and digital technology use . Nature Human Behaviour , 3 ( 2 ), 173. [ PubMed ] [ Google Scholar ]
- Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, … Eaton J (2018). The Lancet Commission on global mental health and sustainable development . The Lancet . [ PubMed ] [ Google Scholar ]
- Primack BA, Shensa A, Escobar-Viera CG, Barrett EL, Sidani JE, Colditz JB, & James AE (2017). Use of multiple social media platforms and symptoms of depression and anxiety: A nationally-representative study among US young adults . Computers in Human Behavior , 69 , 1–9. [ Google Scholar ]
- Reece AG, & Danforth CM (2017). Instagram photos reveal predictive markers of depression . EPJ Data Science , 6 ( 1 ), 15. [ Google Scholar ]
- Reece AG, Reagan AJ, Lix KL, Dodds PS, Danforth CM, & Langer EJ (2017). Forecasting the onset and course of mental illness with Twitter data . Scientific reports , 7 ( 1 ), 13006. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rideout V, & Fox S (2018). Digital health practices, social media use, and mental well-being among teens and young adults in the U.S Retrieved from San Francisco, CA: https://www.hopelab.org/reports/pdf/a-national-survey-by-hopelab-and-well-being-trust-2018.pdf [ Google Scholar ]
- Saha K, Torous J, Ernala SK, Rizuto C, Stafford A, & De Choudhury M (2019). A computational study of mental health awareness campaigns on social media . Translational behavioral medicine . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schlosser DA, Campellone T, Kim D, Truong B, Vergani S, Ward C, & Vinogradov S (2016). Feasibility of PRIME: a cognitive neuroscience-informed mobile app intervention to enhance motivated behavior and improve quality of life in recent onset schizophrenia . JMIR research protocols , 5 ( 2 ). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schlosser DA, Campellone TR, Truong B, Etter K, Vergani S, Komaiko K, & Vinogradov S (2018). Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia . Schizophrenia bulletin , 44 ( 5 ), 1010–1020. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schrank B, Sibitz I, Unger A, & Amering M (2010). How patients with schizophrenia use the internet: qualitative study . Journal of medical Internet research , 12 ( 5 ), e70. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schueller SM, Hunter JF, Figueroa C, & Aguilera A (2019). Use of digital mental health for marginalized and underserved populations . Current Treatment Options in Psychiatry , 6 ( 3 ), 243–255. [ Google Scholar ]
- Shatte AB, Hutchinson DM, & Teague SJ (2019). Machine learning in mental health: a scoping review of methods and applications . Psychological medicine , 49 ( 9 ), 1426–1448. [ PubMed ] [ Google Scholar ]
- Spinzy Y, Nitzan U, Becker G, Bloch Y, & Fennig S (2012). Does the Internet offer social opportunities for individuals with schizophrenia? a cross-sectional pilot study . Psychiatry research , 198 ( 2 ), 319–320. [ PubMed ] [ Google Scholar ]
- Stiglic N, & Viner RM (2019). Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews . BMJopen , 9 ( 1 ), e023191. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sumner SA, Galik S, Mathieu J, Ward M, Kiley T, Bartholow B, … Mork P (2019). Temporal and geographic patterns of social media posts about an emerging suicide game . Journal of Adolescent Health . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Torous J, Chan SR, Tan SY-M, Behrens J, Mathew I, Conrad EJ, … Keshavan M (2014). Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: a survey in four geographically distinct psychiatric clinics . JMIR mental health , 1 ( 1 ), e5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Torous J, Friedman R, & Keshavan M (2014). Smartphone ownership and interest in mobile applications to monitor symptoms of mental health conditions . JMIR mHealth and uHealth , 2 ( 1 ), e2. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Torous J, & Keshavan M (2016). The role of social media in schizophrenia: evaluating risks, benefits, and potential . Current opinion in psychiatry , 29 ( 3 ), 190–195. [ PubMed ] [ Google Scholar ]
- Torous J, Wisniewski H, Bird B, Carpenter E, David G, Elejalde E, … Henson P (2019). Creating a digital health smartphone app and digital phenotyping platform for mental health and diverse healthcare needs: an interdisciplinary and collaborative approach . Journal of Technology in Behavioral Science , 1–13. [ Google Scholar ]
- Trefflich F, Kalckreuth S, Mergl R, & Rummel-Kluge C (2015). Psychiatric patients’ internet use corresponds to the internet use of the general public . Psychiatry research , 226 , 136–141. [ PubMed ] [ Google Scholar ]
- Twenge JM, & Campbell WK (2018). Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study . Preventive medicine reports , 12 , 271–283. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Twenge JM, Joiner TE, Rogers ML, & Martin GN (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time . Clinical Psychological Science , 6 ( 1 ), 3–17. [ Google Scholar ]
- Tynes BM, Willis HA, Stewart AM, & Hamilton MW (2019). Race-related traumatic events online and mental health among adolescents of color . Journal of Adolescent Health , 65 ( 3 ), 371–377. [ PubMed ] [ Google Scholar ]
- Vannucci A, Flannery KM, & Ohannessian CM (2017). Social media use and anxiety in emerging adults . Journal of affective disorders , 207 , 163–166. [ PubMed ] [ Google Scholar ]
- Vayreda A, & Antaki C (2009). Social support and unsolicited advice in a bipolar disorder online forum . Qualitative health research , 19 ( 7 ), 931–942. [ PubMed ] [ Google Scholar ]
- Ventola CL (2014). Social media and health care professionals: benefits, risks, and best practices . Pharmacy and Therapeutics , 39 ( 7 ), 491. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- We Are Social. (2020). Digital in 2020 . Retrieved from https://wearesocial.com/global-digital-report-2019
- Webb H, Jirotka M, Stahl BC, Housley W, Edwards A, Williams M, … Burnap P (2017). The ethical challenges of publishing Twitter data for research dissemination . Paper presented at the Proceedings of the 2017 ACM on Web Science Conference. [ Google Scholar ]
- Williams ML, Burnap P, & Sloan L (2017). Towards an ethical framework for publishing Twitter data in social research: Taking into account users’ views, online context and algorithmic estimation . Sociology , 57 ( 6 ), 1149–1168. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Woods HC, & Scott H (2016). # Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem . Journal of adolescence , 57 , 41–49. [ PubMed ] [ Google Scholar ]
- Ybarra ML (2004). Linkages between depressive symptomatology and Internet harassment among young regular Internet users . Cyber Psychology & Behavior , 7 ( 2 ), 247–257. [ PubMed ] [ Google Scholar ]
Care Coordinator, Behavioral Health-1
Community health workers.
- 1 Boston Medical Center Place, Boston, Massachusetts
POSITION SUMMARY:
The Behavioral Health (BH) Community Partners (CP) Program is a set of community-based organizations serving MassHealth members enrolled in either an Accountable Care Organization (ACO) or Managed Care Organization (MCO). The CP Program partners with health care providers, social services organizations and community resources to support members with complex behavioral health needs. This role will be based in the community and serve as a vital link connecting homeless individuals with serious mental illness, substance use disorders, and/or complex medical illnesses with needed care including mental health, substance use, and primary care as well as services that address social determinants of health needs.
The BH CP Care Coordinator will work as part of an interdisciplinary BH CP team and take responsibility for coordinating the care for up to 50 enrollees. The BH CP Care Coordinator will work closely with other care team members and will be responsible for engaging their enrollees regularly (several times a month), mostly face to face, and making sure that the enrollee is getting connected to vital services and progressing towards the goals outlined in their Person-Centered Care Plan.
Position: Care Coordinator, Behavioral Health
Department: Pop Health Care Management
Schedule: Full Time
ESSENTIAL RESPONSIBILITIES / DUTIES:
Essential Functions :
- Under the direction of the assigned Enrollee, develop a BH Care Plan with nurse case managers.
- Work with the nurse care managers, conduct timely Comprehensive Assessments
- Communicate and engages with enrollees regularly and helps enrollee progress on goals identified in Patient Centered Care Plan.
- Document into data platform regarding enrollee progress on Care Plan goals, all enrollee encounters, care coordination notes. All patients on panel require at least once/month contact and documentation.
- Assist nurse care managers and BH CP teams with arranging enrollee appointments for services needed and other related assessments; accompanies enrollees to appointments as needed
- Triage and troubleshoot care need issues for enrollees; works with nurse care managers to address needs
- Participate in team case conferences and advocate for enrollees’ needs
- Participate in BH CP training and learning initiatives.
- Remind enrollees about keeping appointments, filling prescriptions, etc.
- Work with BH CP team on dev & implementation of Patient Centered Care Plan
- Request & send medical records to for care coordination purposes to providers, ACO, MCO as needed
- Be flexible and able to multi-task.
Other Duties
- Please note this job description is not designed to cover or contain a comprehensive listing of activities, duties or responsibilities that are required of the employee for this job. Duties, responsibilities and activities may change at any time with or without notice.
Supervision Received:
- Weekly and ongoing from Clinical Care Manager and Registered Nurses
JOB REQUIREMENTS:
Education :
- (A.) LICSW or LCSW; or (B.) Bachelor’s degree in social work, human services, nursing, psychology, sociology, or related field; or (C.) Associate’s degree and at least one year of professional experience in the field; or (D.) at least three years of relevant professional experience.
Experience :
- Experience working with homeless populations and/or populations with mental illness and substance use disorders.
Preferred/Desirable :
- Bilingual English/Spanish, or English/Haitian Creole preferred
- Experience with Epic, eHana, or other EHR system
Certification or Conditions of Employment :
- Pre-employment background check
- Regular and reliable transportation and the ability to conduct face-to-face appointments with members, providers, community and state agencies
Competencies, Skills, and Attributes :
- Ability to visit consumers in the environment in which they reside such as the individual’s home, apartment, shelter, group home, etc.
- Must possess advanced skills in consumer assessment and be able to assess the physical conditions of the consumer's home as well as the consumer.
- Exhibit interpersonal flexibility, initiative, and teamwork.
- Solid organizational skills
- Ability to use computer systems in various environments (mobile phone, desktop, tablet).
- Ability to learn and utilize various software programs.
- Acceptance of the right to self-determination.
- Maintains consumers’ rights, privacy and confidentiality in all aspects of the job, including those relating to diagnosis and consumer records.
- Promotes and employs ethical actions at all times with consumer’s families and others.
- Participates in performance improvement activities as requested to do so.
- Identifies and communicates opportunities for improvement.
- Demonstrates excellent customer service by conducting daily activities, communications and interactions in a cooperative, positive and professional manner.
- Proficient in reading, writing, and communicating in English
- Communicate in a manner appropriate and respectful to the comprehension level of the consumer and/or family.
- Maintains the responsibility for punctuality and attendance as defined in the agency policy to ensure optimal operation of the program.
- Submits requests for vacation, days off, etc. in accordance with department policy.
- Regular and reliable attendance is an essential function of the position.
- Work may be performed in a typical interior/office work environment or in a home office except when conducting face-to-face visits.
- Face-to-face visits may be conducted in a member’s home, shelters, physician practices, hospitals, or at a mutually agreed upon location between the member and the care manager and with community and state agencies, as appropriate.
- No or very limited physical effort required. No or very limited exposure to physical risk.
Equal Opportunity Employer/Disabled/Veterans
Privacy policy
By clicking Submit, you acknowledge that you are willing to receive messages from Boston Medical Center relating to the status of your application or other recruitment related information to any mobile / cell phone number entered in the form above. You can easily opt-out of receiving messages by replying STOP to any messages you receive.
Not the right fit? Check out these other jobs
Pediatric ambulatory medical assistant, clinical research nurse i, community wellness advocate (greater boston area), mental health specialist, brockton behavioral health center, 24hrs (evenings/nights), medical transcriptionist (per diem)(not remote), refer a friend.
Your information:
Apply for this job now
EEO & Accommodation Statement Boston Medical Center is an equal employment/affirmative action employer. We ensure equal employment opportunities for all, without regard to race, color, religion, sex, national origin, age, disability, veteran status, sexual orientation, gender identity and/or expression or any other non-job-related characteristic. If you need accommodation for any part of the application process because of a medical condition or disability, please send an e-mail to [email protected] or call 617-638-8582 to let us know the nature of your request
E-Verify Program Boston Medical Center participates in the Electronic Employment Verification Program. As an E-Verify employer, prospective employees of BMC must complete a background check and receive medical clearance before beginning their employment at the hospital.
Federal Trade Commission Statement: According to the FTC, there has been a rise in employment offer scams. Our current job openings are listed on our website and applications are received only through our website. We do not ask or require downloads of any applications, or “apps” job offers are not extended over text messages or social media platforms. We do not ask individuals to purchase equipment for or prior to employment. To avoid becoming a victim of an employment offer scam, please follow these tips from the FTC: FTC Tips
Join the BMC Talent Community
Before you go, don't forget to join our talent community!

We use cookies to make your interactions with our website more meaningful. They help us better understand how our websites are used, so we can tailor content for you. For more information about the different cookies we are using, read the Privacy Statement . By continuing to navigate the site, you agree to the use of cookies on our behalf.

IMAGES
COMMENTS
Therefore, in the current review, we aimed to synthesize existing literature on various mental health promotion and prevention interventions and their effectiveness. Additionally, we intend to highlight various novel approaches to mental health care and their implications across different resource settings and provide future directions.
Abstract Background: Research increasingly shows how selective and targeted use of technology within care and welfare can have several advantages including improved quality of care and active user involvement. Purpose: The current overview of reviews aims to summarize the research on the effectiveness of technology for mental health and wellbeing.
The investment in mental health research is critical for enhancing access to care and developing appropriate interventions. These interventions are vital for addressing the immediate need to overhaul and expand mental health care services for a significant impact within various communities (WHO, 2022). To maintain and amplify this impact, there ...
Amid a shortage of mental health providers, digital therapeutics could play an important role in providing support for underserved communities.
A systematic review of interventions to support mental health and wellbeing of university and college students, based on review-level evidence.
Peer support for mental health is recommended across international policy guidance and provision. Our systematic umbrella review summarises evidence on the effectiveness, implementation, and experiences of paid peer support approaches for mental health.
Further, NIMH is committed to working with researchers, communities, payors, advocacy groups, state policymakers, federal agencies, and others to help support intervention and services science that will significantly impact mental health policy and care practices—ultimately helping people access better mental health care.
Although there can be major barriers to accessing mental health care prompted by cultural influences, access itself is subject to community and country-level constraints, including funding for ...
The COVID-19 pandemic required mental health clinicians globally to transition to the delivery of care via telehealth. This study aimed to gain an understanding of clients' satisfaction with and attitudes towards telehealth mental health services.
The National Institute of Mental Health (NIMH) is the Nation's leader in research on mental disorders, supporting research to transform the understanding and treatment of mental illnesses. Below you can learn more about NIMH funded research areas, policies, resources, initiatives, and research conducted by NIMH on the NIH campus.
Goal 4: Research to improve choice of, and access to, mental health care, treatment and support in hospital and community settings. There is a failure to reach all the people who need care and support, as well as enabling them timely access to evidence-based treatment and support.
The AAMC Research and Action Institute looks at the mental health crisis—including workforce shortages, lack of insurance parity, and how to fix it.
The Surgeon General's Framework for Mental Health and Well-Being in the Workplace, which cites research from APA, is designed to encourage organizations to rethink how they protect workers from harm, foster a sense of connection among workers, show workers that they matter, make space for their lives outside work, and support their growth.
In this article we aim to scope existing literature regarding (a) the associations between social support, mental health and recovery, and (b) describe features of community mental health services that incorporate social support. Further, we discuss facilitators and barriers for social work and social support.
Mental health disparities are significant and easily documented. In this Director's Message, Dr. Gordon discusses NIMH-funded research that aims to close the gap, ensuring that improved mental health care meets the needs of all Americans.
Family engagement in care has been advocated to promote recovery for patients with mental health conditions. Attitudes of mental health nurses toward the importance of families influence the way they partner with families in mental healthcare. However, little is known about how mental health nurses engage with families and quality of family ...
This article is cited by A rapid narrative review of the clinical evolution of psychedelic treatment in clinical trials Ronit Kishon Nadav Liam Modlin James Rucker npj Mental Health Research (2024)
Many people experience mental health conditions, which raises questions about mental health service utilization patterns and what barriers exist with connecting people to services. This analysis ...
This paper examines the current landscape of remote mental health care as a viable treatment delivery method and uses clinical outcomes data from patients undergoing in-person and telehealth mental health treatment at a large, multistate behavioral health system to illustrate telehealth's comparability to traditional, in-person care.
The results of APA's 2022 Work and Well-being Survey reveal that seven in 10 workers (71%) believe their employer is more concerned about the mental health of employees now than in the past. This new focus is highly valued by employees. In fact, 81% of individuals said they will be looking for workplaces that support mental health when they seek future job opportunities.
Peer support is recognized as an evidence-based practice for individuals with mental health conditions or challenges. Quantitative and qualitative evidence indicates that peer support: lowers the overall cost of mental health services by reducing re-hospitalization rates and the days spent in inpatient services; increases and improves ...
This report provides recommendations to support mental health and well-being of residents, families, and care providers in long-term care.
Meanwhile, years of systemic neglect and disinvestment have left resources for mental health scarce. But new USIP research reveals that local leaders are finding innovative ways to support their community's mental health and emotional wellbeing — including through partnerships with religious actors.
How to support children's mental health through play. Supporting children's mental health with play is, first and foremost, a systemic issue. Above all, providers, researchers, and lawmakers need to raise awareness of how play impacts mental health and create more opportunities for children to play.
We found limited evidence to support a protective association between breastfeeding and the development of mental health disorders in children later in life. The data regarding the association between breastfeeding and maternal mental health beyond the postnatal period is also limited. The methodolo …
The grants support studies to advance post-secondary student mental health and wellness. Professors Emily Seto and Daniel Grace are among five University of Toronto researchers who have been awarded 2023-24 Inlight Research Development Grants to advance knowledge and develop solutions to complex issues related to student mental health.
Heartland Forward has identified opportunities to improve mental health care across the heartland as we work to be a resource for states and local communities - supporting quality of life and overall economic success in the middle of the country. Research Programming
The purpose of this mixed-method study was to investigate levels of PTSD, PTG, QOL, their relationships, and unmet mental health needs of triple-negative breast cancer survivors diagnosed between stages 2b-4 and 2-5 years post-treatment. Participants were recruited through two cancer organizations, breast health navigators, TNBC support groups, and online breast cancer support groups.
Social media platforms are popular venues for sharing personal experiences, seeking information, and offering peer-to-peer support among individuals living with mental illness. With significant shortfalls in the availability, quality, and reach of evidence-based mental health services across the United States and globally, social media ...
POSITION SUMMARY: The Behavioral Health (BH) Community Partners (CP) Program is a set of community-based organizations serving MassHealth members enrolled in either an Accountable Care Organization (ACO) or Managed Care Organization (MCO). The CP Program partners with health care providers, social services organizations and community resources to support members with complex behavioral health ...