Lung Cancer Research Results and Study Updates
See Advances in Lung Cancer Research for an overview of recent findings and progress, plus ongoing projects supported by NCI.
Lorlatinib (Lorbrena) is superior to crizotinib (Xalkori) as an initial treatment for people with ALK-positive advanced non-small cell lung cancer, according to new clinical trial results. Treatment with lorlatinib also helped prevent new brain metastases.
The immunotherapy drug durvalumab (Imfinzi) can help people with early-stage small cell lung cancer live longer, results from a large clinical trial show. Three years after starting treatment, nearly 60% of people who received the drug were still alive.
FDA has approved alectinib (Alecensa) as adjuvant therapy for people with lung cancer who have ALK-positive tumors. In a clinical trial, alectinib helped people live longer after surgery without their cancer returning than chemotherapy.
The results of the clinical trial that led to FDA’s 2023 approval of repotrectinib (Augtyro) for lung cancers with ROS1 fusions have been published. The drug shrank tumors in 80% of people receiving the drug as an initial treatment.
A collection of material about the ALCHEMIST lung cancer trials that will examine tumor tissue from patients with certain types of early-stage, completely resected non-small cell lung cancer for gene mutations in the EGFR and ALK genes, and assign patients with these gene mutations to treatment trials testing post-surgical use of drugs targeted against these mutations.
Tarlatamab, a new type of targeted immunotherapy, shrank small cell lung cancer (SCLC) tumors in more than 30% of participants in an early-stage clinical trial. Participants had SCLC that had progressed after previous treatments with other drugs.
For people with lung cancer and medullary thyroid cancer whose tumors have changes in the RET gene, selpercatinib improved progression-free survival compared with other common treatments, according to new clinical trial results.
In the ADAURA clinical trial, people with early-stage lung cancer treated with osimertinib (Tagrisso) after surgery lived longer than people treated with a placebo after surgery. Despite some criticisms about its design, the trial is expected to change patient care.
For certain people with early-stage non-small cell lung cancer, sublobar surgery to remove only a piece of the affected lung lobe is as effective as surgery to remove the whole lobe, new research shows.
Pragmatica-Lung is a clinical trial for people with non-small cell lung cancer that has spread beyond the lungs (stage 4 cancer). The trial will help confirm if the combination of pembrolizumab and ramucirumab helps people with advanced lung cancer live longer.
On August 11, the Food and Drug Administration (FDA) gave accelerated approval to trastuzumab deruxtecan (Enhertu) for adults with non-small cell lung cancer (NSCLC) that has a specific mutation in the HER2 gene. Around 3% of people with NSCLC have this kind of HER2 mutation.
Giving people with early-stage lung cancer the immunotherapy drug nivolumab (Opdivo) and chemotherapy before surgery can substantially delay the progression or return of their cancer, a large clinical trial found.
Atezolizumab (Tecentriq) is now the first immunotherapy approved by FDA for use as an additional, or adjuvant, treatment for some patients with non-small cell lung cancer. The approval was based on results of a clinical trial called IMpower010.
Quitting smoking after a diagnosis of early-stage lung cancer may help people live longer, a new study finds. The study, which included more than 500 patients, also found that quitting smoking delayed the cancer from returning or getting worse.
NCI scientists and their international collaborators have found that the majority of lung cancers in never smokers arise when mutations caused by natural processes in the body accumulate. They also identified three subtypes of lung cancer these individuals.
FDA has approved the first KRAS-blocking drug, sotorasib (Lumakras). The approval, which covers the use of sotorasib to treat some patients with advanced lung cancer, sets the stage for other KRAS inhibitors already in development, researchers said.
Combining the chemotherapy drug topotecan and the investigational drug berzosertib shrank tumors in some patients with small cell lung cancer, results from an NCI-supported phase 1 clinical trial show. Two phase 2 trials of the combination are planned.
Mortality rates from the most common lung cancer, non-small cell lung cancer (NSCLC), have fallen sharply in the United States in recent years, due primarily to recent advances in treatment, an NCI study shows.
In a study of more than 50,000 veterans with lung cancer, those with mental illness who received mental health treatment—including for substance use—lived substantially longer than those who didn’t participate in such programs.
FDA has granted accelerated approval for selpercatinib (Retevmo) to treat certain patients with thyroid cancer or non-small cell lung cancer whose tumors have RET gene alterations. The drug, which works by blocking the activity of RET proteins, was approved based on the results of the LIBRETTO-001 trial.
Osimertinib (Tagrisso) improves survival in people with non-small cell lung cancer with EGFR mutations, updated clinical trial results show. People treated with osimertinib lived longer than those treated with earlier-generation EGFR-targeted drugs.
A large clinical trial showed that adding the immunotherapy drug durvalumab (Imfinzi) to standard chemotherapy can prolong survival in some people with previously untreated advanced small cell lung cancer.
The investigational drug selpercatinib may benefit patients with lung cancer whose tumors have alterations in the RET gene, including fusions with other genes, according to results from a small clinical trial.
FDA has approved entrectinib (Rozlytrek) for the treatment of children and adults with tumors bearing an NTRK gene fusion. The approval also covers adults with non-small cell lung cancer harboring a ROS1 gene fusion.
Clinical recommendations on who should be screened for lung cancer may need to be reviewed when it comes to African Americans who smoke, findings from a new study suggest.
Use of a multipronged approach within hospitals, including community centers, not only eliminated treatment disparities among black and white patients with early-stage lung cancer, it also improved treatment rates for all patients, results from a new study show.
In everyday medical care, there may be more complications from invasive diagnostic procedures performed after lung cancer screening than has been reported in large studies.
The Lung Cancer Master Protocol, or Lung-MAP, is a precision medicine research study for people with advanced non-small cell lung cancer that has continued to grow after treatment. Patients are assigned to different study drug combinations based on the results of genomic profiling of their tumors.
On December 6, 2018, the Food and Drug Administration (FDA) approved atezolizumab (Tecentriq) in combination with a standard three-drug regimen as an initial treatment for advanced lung cancer that does not have EGFR or ALK mutations.
A new study has identified a potential biomarker of early-stage non–small cell lung cancer (NSCLC). The biomarker, the study’s leaders said, could help diagnose precancerous lung growths and early-stage lung cancers noninvasively and distinguish them from noncancerous growths.
Advertisement

Recent advances in lung cancer research: unravelling the future of treatment
- Review Article
- Published: 06 April 2024
Cite this article

- Luca Bertolaccini ORCID: orcid.org/0000-0002-1153-3334 1 ,
- Monica Casiraghi 1 , 2 ,
- Clarissa Uslenghi 1 ,
- Sebastiano Maiorca 1 &
- Lorenzo Spaggiari 1 , 2
779 Accesses
3 Citations
1 Altmetric
Explore all metrics
Lung cancer, a multifaceted disease, demands tailored therapeutic approaches due to its diverse subtypes and stages. This comprehensive review explores the intricate landscape of lung cancer research, delving into recent breakthroughs and their implications for diagnosis, therapy, and prevention. Genomic profiling and biomarker identification have ushered in the era of personalised medicine, enabling targeted therapies that minimise harm to healthy tissues while effectively combating cancer cells. The relationship between pulmonary tuberculosis and lung cancer is examined, shedding light on potential mechanisms linking these two conditions. Early detection methods, notably low-dose computed tomography scans, have significantly improved patient outcomes, emphasising the importance of timely interventions. There has been a growing interest in segmentectomy as a surgical intervention for early-stage lung cancer in recent years. Immunotherapy has emerged as a transformative approach, harnessing the body's immune system to recognise and eliminate cancer cells. Combining immunotherapy with traditional treatments, such as chemotherapy and targeted therapies, has shown enhanced efficacy, addressing the disease's heterogeneity and overcoming drug resistance. Precision medicine, guided by genomic profiling, has enabled the development of targeted therapies like tyrosine kinase inhibitors, offering personalised treatments tailored to individual patients. Challenges such as drug resistance and limited accessibility to advanced therapies persist, emphasising the need for collaborative efforts and innovative technologies like artificial intelligence. Despite challenges, ongoing interdisciplinary collaborations and technological advancements offer hope for a future where lung cancer is treatable and preventable, reducing the burden on patients and healthcare systems worldwide.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

The artificial intelligence and machine learning in lung cancer immunotherapy
Application of clinical bioinformatics in lung cancer-specific biomarkers.
Precision Medicine in Lung Cancer
Data availability.
Not applicable.
Cheng B, Xiong S, Li C, Liang H, Zhao Y, Li J et al (2020) An annual review of the remarkable advances in lung cancer clinical research in 2019. J Thorac Dis 12(3):1056–1069
Article PubMed PubMed Central Google Scholar
Ibodeng GO, Uche IN, Mokua R, Galo M, Odigwe B, Galeas JN, Dasgupta S (2023) A snapshot of lung cancer: where are we now?-a narrative review. Ann Transl Med 11(6):261
Article CAS PubMed PubMed Central Google Scholar
Bertolaccini L, Casiraghi M, Petrella F, Rampinelli C, Tessitore A, Spaggiari L (2022) A methodological quality evaluation of the published guidelines and recommendations about the lung cancer screening. Eur J Cancer Prev 31(1):19–25
Article PubMed Google Scholar
Duma N, Santana-Davila R, Molina JR (2019) Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc 94(8):1623–1640
Article CAS PubMed Google Scholar
Hwang SY, Kim JY, Lee HS, Lee S, Kim D, Kim S et al (2022) Pulmonary tuberculosis and risk of lung cancer: a systematic review and meta-analysis. J Clin Med 11(3):765
Yaegashi LB, Baldavira CM, Prieto TG, Machado-Rugolo J, Velosa APP, da Silveira LKR et al (2021) In situ overexpression of matricellular mechanical proteins demands functional immune signature and mitigates non-small cell lung cancer progression. Front Immunol 12:714230
Bourgot I, Primac I, Louis T, Noel A, Maquoi E (2020) Reciprocal interplay between fibrillar collagens and collagen-binding integrins: implications in cancer progression and metastasis. Front Oncol 10:1488
Horne ZD, Jack R, Gray ZT, Siegfried JM, Wilson DO, Yousem SA et al (2011) Increased levels of tumor-infiltrating lymphocytes are associated with improved recurrence-free survival in stage 1A non-small-cell lung cancer. J Surg Res 171(1):1–5
Jamal-Hanjani M, Wilson GA, McGranahan N, Birkbak NJ, Watkins TBK, Veeriah S et al (2017) Tracking the evolution of non-small-cell lung cancer. N Engl J Med 376(22):2109–2121
Oliver AL (2022) Lung cancer: epidemiology and screening. Surg Clin North Am 102(3):335–344
Ribas A, Wolchok JD (2018) Cancer immunotherapy using checkpoint blockade. Science 359(6382):1350–1355
Sahin U, Derhovanessian E, Miller M, Kloke BP, Simon P, Lower M et al (2017) Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer. Nature 547(7662):222–226
Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ et al (2014) Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med 371(16):1507–1517
Franzi S, Mattioni G, Rijavec E, Croci GA, Tosi D (2022) Neoadjuvant chemo-immunotherapy for locally advanced non-small-cell lung cancer: a review of the literature. J Clin Med 11(9):2629
Szeto CH, Shalata W, Yakobson A, Agbarya A (2021) Neoadjuvant and adjuvant immunotherapy in early-stage non-small-cell lung cancer, past, present, and future. J Clin Med 10(23):5614
Chai Y, Wu X, Bai H, Duan J (2022) Combined immunotherapy with chemotherapy versus bevacizumab with chemotherapy in first-line treatment of driver-gene-negative non-squamous non-small cell lung cancer: an updated systematic review and network meta-analysis. J Clin Med 11(6):1655
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J et al (2002) Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 346(2):92–98
Gandhi L, Rodriguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F et al (2018) Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 378(22):2078–2092
Tsuboi M, Herbst RS, John T, Kato T, Majem M, Grohe C et al (2023) Overall Survival with Osimertinib in Resected EGFR-mutated NSCLC. N Engl J Med 389(2):137–147
Dohopolski M, Iyengar P (2021) Oligometastatic non-small cell lung cancer: a narrative review of stereotactic ablative radiotherapy. Ann Palliat Med 10(5):5944–5953
Yuan Z, Wang Y, Zhang J, Zheng J, Li W (2019) A meta-analysis of clinical outcomes after radiofrequency ablation and microwave ablation for lung cancer and pulmonary metastases. J Am Coll Radiol 16(3):302–314
Chen Y, Luo H, Liu R, Tan M, Wang Q, Wu X et al (2023) Efficacy and safety of particle therapy for inoperable stage II–III non-small cell lung cancer: a systematic review and meta-analysis. Radiat Oncol 18(1):86
Harada H, Suefuji H, Mori K, Ishikawa H, Nakamura M, Tokumaru S et al (2023) Proton and carbon ion radiotherapy for operable early-stage lung cancer: 3-year results of a prospective nationwide registry. Int J Radiation Oncol Biol Phys 117(2):23
Article Google Scholar
de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA et al (2020) reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med 382(6):503–513
Huo B, Manos D, Xu Z, Matheson K, Chun S, Fris J et al (2023) Screening criteria evaluation for expansion in pulmonary neoplasias (SCREEN). Semin Thorac Cardiovasc Surg 35(4):769–780
Passiglia F, Cinquini M, Bertolaccini L, Del Re M, Facchinetti F, Ferrara R et al (2021) Benefits and harms of lung cancer screening by chest computed tomography: a systematic review and meta-analysis. J Clin Oncol 39(23):2574–2585
Qi SA, Wu Q, Chen Z, Zhang W, Zhou Y, Mao K et al (2021) High-resolution metabolomic biomarkers for lung cancer diagnosis and prognosis. Sci Rep 11(1):11805
Madama D, Martins R, Pires AS, Botelho MF, Alves MG, Abrantes AM, Cordeiro CR (2021) Metabolomic profiling in lung cancer: a systematic review. Metabolites 11(9):630
Planchard D, Kim TM, Mazieres J, Quoix E, Riely G, Barlesi F et al (2016) Dabrafenib in patients with BRAF(V600E)-positive advanced non-small-cell lung cancer: a single-arm, multicentre, open-label, phase 2 trial. Lancet Oncol 17(5):642–650
Araujo DC, Veloso AA, Borges KBG, Carvalho MDG (2022) Prognosing the risk of COVID-19 death through a machine learning-based routine blood panel: a retrospective study in Brazil. Int J Med Inform 165:104835
Chiu HY, Chao HS, Chen YM (2022) Application of artificial intelligence in lung cancer. Cancers (Basel) 14(6):1370
Christie JR, Lang P, Zelko LM, Palma DA, Abdelrazek M, Mattonen SA (2021) Artificial intelligence in lung cancer: bridging the gap between computational power and clinical decision-making. Can Assoc Radiol J 72(1):86–97
Goncalves S, Fong PC, Blokhina M (2022) Artificial intelligence for early diagnosis of lung cancer through incidental nodule detection in low- and middle-income countries-acceleration during the COVID-19 pandemic but here to stay. Am J Cancer Res 12(1):1–16
CAS PubMed PubMed Central Google Scholar
Goldsmith I, Chesterfield-Thomas G, Toghill H (2021) Pre-treatment optimization with pulmonary rehabilitation in lung cancer: making the inoperable patients operable. EClinicalMedicine 31:100663
Shields MD, Chen K, Dutcher G, Patel I, Pellini B (2022) Making the rounds: exploring the role of circulating tumor DNA (ctDNA) in non-small cell lung cancer. Int J Mol Sci 23(16):9006
Abbosh C, Frankell AM, Harrison T, Kisistok J, Garnett A, Johnson L et al (2023) Tracking early lung cancer metastatic dissemination in TRACERx using ctDNA. Nature 616(7957):553–562
Zaman FY, Subramaniam A, Afroz A, Samoon Z, Gough D, Arulananda S, Alamgeer M (2023) Circulating tumour DNA (ctDNA) as a predictor of clinical outcome in non-small cell lung cancer undergoing targeted therapies: a systematic review and meta-analysis. Cancers (Basel) 15(9):2425
Jaffee EM, Dang CV, Agus DB, Alexander BM, Anderson KC, Ashworth A et al (2017) Future cancer research priorities in the USA: a lancet oncology commission. Lancet Oncol 18(11):e653–e706
Saji H, Okada M, Tsuboi M, Nakajima R, Suzuki K, Aokage K et al (2022) Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 399(10335):1607–1617
Nakada T, Noda Y, Kato D, Shibasaki T, Mori S, Asano H et al (2019) Risk factors and cancer recurrence associated with postoperative complications after thoracoscopic lobectomy for clinical stage I non-small cell lung cancer. Thorac Cancer 10(10):1945–1952
Bedetti B, Bertolaccini L, Rocco R, Schmidt J, Solli P, Scarci M (2017) Segmentectomy versus lobectomy for stage I non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis 9(6):1615–1623
Bertolaccini L, Prisciandaro E, Bardoni C, Cara A, Diotti C, Girelli L, Spaggiari L (2022) Minimally invasive anatomical segmentectomy versus lobectomy in stage IA non-small cell lung cancer: a systematic review and meta-analysis. Cancers (Basel) 14(24):6157
Wang P, Fu YH, Qi HF, He P, Wang HF, Li C, Liu XC (2023) Evaluation of the efficacy and safety of robot-assisted and video assisted thoracic surgery for early non-small cell lung cancer: a meta-analysis. Technol Health Care 32(2):511–523
Casiraghi M, Galetta D, Borri A, Tessitore A, Romano R, Diotti C et al (2019) Ten years’ experience in robotic-assisted thoracic surgery for early stage lung cancer. Thorac Cardiovasc Surg 67(7):564–572
Wang P, Wang S, Liu Z, Sui X, Wang X, Li X et al (2022) Segmentectomy and wedge resection for elderly patients with stage I non-small cell lung cancer: a systematic review and meta-analysis. J Clin Med 11(2):294
Bertolaccini L, Cara A, Chiari M, Diotti C, Glick N, Mohamed S et al (2023) Real-world survival outcomes of wedge resection versus lobectomy for cT1a/b cN0 cM0 non-small cell lung cancer: a single center retrospective analysis. Front Oncol 13:1226429
Bertolaccini L, Spaggiari L (2023) Is it time to cross the pillars of evidence in favor of segmentectomies in early-stage non-small cell lung cancer? Cancers (Basel) 15(7):1993
Zaraca F, Kirschbaum A, Pipitone MD, Bertolaccini L, Group PS (2023) Prospective randomized study on the efficacy of three-dimensional reconstructions of bronchovascular structures on preoperative chest CT scan in patients who are candidates for pulmonary segmentectomy surgery: the patches (prospective randomized study efficacy of three-dimensional reconstructions segmentecomy) study protocol. Trials 24(1):594
Komarnicki P, Musialkiewicz J, Stanska A, Maciejewski A, Gut P, Mastorakos G, Ruchala M (2022) Circulating neuroendocrine tumor biomarkers: past, present and future. J Clin Med 11(19):5542
Coudray N, Ocampo PS, Sakellaropoulos T, Narula N, Snuderl M, Fenyo D et al (2018) Classification and mutation prediction from non-small cell lung cancer histopathology images using deep learning. Nat Med 24(10):1559–1567
Biesinger M, Eicken N, Varga A, Weber M, Brndiar M, Erd G et al (2022) Lymph but not blood vessel invasion is independent prognostic in lung cancer patients treated by VATS-lobectomy and might represent a future upstaging factor for early stages. Cancers 14(8):1893
Asamura H, Nishimura KK, Giroux DJ, Chansky K, Hoering A, Rusch V, et al (2023) IASLC Lung Cancer Staging Project The New Database to Inform Revisions in the Ninth Edition of the TNM Classification of Lung Cancer. J Thorac Oncol 18(5): 564–575
Hardenberg MC, Patel B, Matthews C, Califano R, Garcia Campelo R, Grohe C et al (2022) The value of disease-free survival (DFS) and osimertinib in adjuvant non-small-cell lung cancer (NSCLC): an international Delphi consensus report. ESMO Open 7(5):100572
Wu YL, Tsuboi M, He J, John T, Grohe C, Majem M et al (2020) Osimertinib in resected EGFR-mutated non-small-cell lung cancer. N Engl J Med 383(18):1711–1723
Xu H, Baidoo AAH, Su S, Ye J, Chen C, Xie Y et al (2019) A comparison of EGFR mutation status in tissue and plasma cell-free DNA detected by ADx-ARMS in advanced lung adenocarcinoma patients. Transl Lung Cancer Res 8(2):135–143
Zou PC, Wang L, Liu B, Zhang HZ, Liu HC (2011) EGFR-targeted therapies combined with chemotherapy for treating advanced non-small-cell lung cancer: a meta-analysis. Diagnostics 9:38
Google Scholar
Solomon BJ, Bauer TM, Mok TSK, Liu G, Mazieres J, de Marinis F et al (2023) Efficacy and safety of first-line lorlatinib versus crizotinib in patients with advanced, ALK-positive non-small-cell lung cancer: updated analysis of data from the phase 3, randomised, open-label CROWN study. Lancet Respir Med 11(4):354–366
Hotta K, Hida T, Nokihara H, Morise M, Kim YH, Azuma K et al (2022) Final overall survival analysis from the phase III J-ALEX study of alectinib versus crizotinib in ALK inhibitor-naive Japanese patients with ALK-positive non-small-cell lung cancer. ESMO Open 7(4):100527
Shaw AT, Bauer TM, de Marinis F, Felip E, Goto Y, Liu G et al (2020) First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N Engl J Med 383(21):2018–2029
Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY et al (2016) Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 387(10027):1540–1550
Isaacs J, Stinchcombe TE (2022) Neoadjuvant and adjuvant systemic therapy for early-stage non-small-cell lung cancer. Drugs 82(8):855–863
John AO, Ramnath N (2023) Neoadjuvant versus adjuvant systemic therapy for early-stage non-small cell lung cancer: the changing landscape due to immunotherapy. Oncologist 28(9):752–764
Wakelee H, Liberman M, Kato T, Tsuboi M, Lee SH, Gao S et al (2023) Perioperative pembrolizumab for early-stage non-small-cell lung cancer. N Engl J Med 389(6):491–503
Kogure Y, Hashimoto H, Oki M (2021) A randomized phase iii study of pembrolizumab versus pembrolizumab-carboplatin-pemetrexed for locally advanced or metastatic nonsquamous non-small-cell lung cancer with PD-L1 50% or more (LAPLACE-50): study protocol. Clin Lung Cancer 11:921–924
Download references
Acknowledgements
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5x1000 funds.
Ministero della Salute, 5 × 1000, Ricerca Corrente.
Author information
Authors and affiliations.
Department of Thoracic Surgery, IEO, European Institute of Oncology IRCCS, Via Ripamonti 435, 20141, Milan, Italy
Luca Bertolaccini, Monica Casiraghi, Clarissa Uslenghi, Sebastiano Maiorca & Lorenzo Spaggiari
Department of Oncology and Hemato-Oncology, University of Milan, Milan, Italy
Monica Casiraghi & Lorenzo Spaggiari
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Luca Bertolaccini .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Bertolaccini, L., Casiraghi, M., Uslenghi, C. et al. Recent advances in lung cancer research: unravelling the future of treatment. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01841-3
Download citation
Received : 06 March 2024
Accepted : 24 March 2024
Published : 06 April 2024
DOI : https://doi.org/10.1007/s13304-024-01841-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lung cancer
- Comprehensive review
- Find a journal
- Publish with us
- Track your research
Masks Strongly Recommended but Not Required in Maryland
Respiratory viruses continue to circulate in Maryland, so masking remains strongly recommended when you visit Johns Hopkins Medicine clinical locations in Maryland. To protect your loved one, please do not visit if you are sick or have a COVID-19 positive test result. Get more resources on masking and COVID-19 precautions .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
News & Publications
Significant advances in lung cancer treatment bring hope.
Much is changing in the treatment of lung cancer and Susan Scott, M.D. , a fellowship-trained medical oncologist specializing in treating lung cancers at the Johns Hopkins Kimmel Cancer Center at Sibley Memorial Hospital, is very excited.
“More than 50% of patients with lung cancer are diagnosed at an early stage, before it's metastatic and has spread outside the chest,” says Dr. Scott. “These patients have been treated the same way for about 30 years, with little improvement. Just in the past year, we've had some exciting developments in how we help these patients.”
Historically, following diagnosis, patients with early-stage lung cancer had surgery sometimes followed by chemotherapy. A recent FDA-approved treatment that combines chemotherapy and immunotherapy, given before surgery, is bringing new hope.
Early Attack Before Surgery
This new treatment is given through an IV over the course of six to nine weeks. The patient receives a combination of two chemotherapies and one immunotherapy agent that work together to jumpstart the immune system to fight the cancer. When the patient is ready for surgery, their immune system is already primed to act as a surveillance mechanism to attack the cancer and prevent it from growing again. These targeted treatments before surgery provide an opportunity to start treating the cancer and shrinking the tumor while it is still in place.
“Even patients who are diagnosed before their disease spreads outside of the chest still have a high risk of the cancer coming back,” says Dr. Scott. “That is scary, and we want to minimize that risk as much as we can. The more can do at the beginning of treatment to essentially cure the cancer is where our research lies and where these exciting new changes come into play.”
Screening for Early Stage Lung Cancer
The identification of early stage lung cancer has increased significantly in the past five years because of low-dose CT screening for smokers. The U.S. Preventive Services Task Force recommends annual lung cancer screening with low-dose CT for people who:
- Have a 20 pack-year or more smoking history, and
- Smoke now or have quit within the past 15 years, and
- Are between 50 and 80 years old.
This screening often finds tumors before they spread outside the lung or cause any symptoms. Dr. Scott notes, “In the Washington, D.C., population we serve, about half of the patients we're seeing have never smoked.” For patients who don't smoke, lung cancer is sometimes found incidentally when they have a CT scan for another reason. Even though some patients present with symptoms, many of these patients will still have cancer that has not yet spread outside the chest and can benefit from this new therapy.
Hope for the Future
“Many lung cancer patients today are now managed like those who have a chronic disease,” says Dr. Scott. “The average life expectancy, even for patients with stage four disease, has tripled in the last several years. In 2021, there were more than 10 new drugs approved for lung cancer alone. That is astronomical for cancer. With clinical trials available at different stages of disease and different phases of treatment, and so many new approaches, we are providing more hope for our patients.”
The Sidney Kimmel Cancer Center at Sibley Memorial Hospital’s multidisciplinary team is comprised of thoracic surgeons, radiation oncologists, medical oncologists, interventional pulmonologists and pathologists who work together to develop a treatment plan tailored for each patient. For more information, visit hopkinscancerdc.org .
- Help & Support
- Lung Health & Diseases
- Lung Disease Lookup
- Lung Cancer
- Lung Cancer Basics
Lung Cancer Research
Why we need research.
Research provides hope and saves lives. This is especially true when it comes to lung cancer research. Lung cancer research can help develop better treatments, increasing the survival and quality of life for patients. Research can provide a better and longer future for those diagnosed with lung cancer as well and can also ultimately increase the number of survivors living with the disease.
The Lung Association supports lung cancer research so we can help prevent lung cancer cases, and failing that, prolong the lives of lung cancer patients. We have made some progress, but we plan to invest more, as lung cancer remains the leading cause of cancer deaths in the United States.
Our Lung Cancer Research Program
The American Lung Association is committed to funding lung cancer research. As part of our Awards and Grants Program , a large part of funds goes toward research on lung cancer prevention, treatment and quality of life. The primary goal of this lung cancer research program is simple: improve and save lives. The secondary goal is almost as important: To fund top-notch lung cancer researchers at important career crossroads to and gain long-term commitment to lung cancer research. Without the life-long dedication of lung cancer researchers and a large and active community of people trying to improve patients' lives, important and much-needed discoveries would be impossible.
What Research Is Being Done?
Thanks to the medical breakthroughs led by Lung Association researchers and their colleagues worldwide, our lung cancer researchers have made significant contributions to the field of lung cancer. For example, biomarker testing and targeted therapies have helped advance the area of personalized treatment (finding the unique genetic makeup of a person's tumor and developing and using drugs that are designed to be most effective for that patient).
Currently funded Lung Association researchers are:
- Finding out why some nonsmokers develop lung cancer
- Discovering new biomarkers as an early warning system to detect the spread of lung cancer
- Decoding the genetic mechanisms which cause lung cancer
- Understanding how the structure and regulation of chromosomes affect lung cancer
- Understanding sex-differences to customize lung cancer treatments
- Using next generation nanotechnology to target lung cancer
- Using a virus to treat lung cancer
- Overcoming obstacles for cellular immunotherapy against lung cancer
- Improving quality of life and access to healthcare for lung cancer patients after completing therapy
- Reversing drug resistance in lung cancers
- Identifying metabolic alterations in lung cancer-associated cachexia
- Testing methods to increase lung cancer screening among Quitline callers
Lung Cancer Researchers
Visit our Meet the Researchers section to view our lung cancer researchers and their studies.
Research Partnerships
Lung cancer interception dream team.
As a collaborative effort with Stand Up To Cancer and the LUNGevity Foundation, the Lung Cancer Interception Dream Team leverages a new approach to lung cancer prevention: cancer interception.
Learn more about the Dream Team .
How You Can Be a Part of Research
Lung cancer registry.
The Lung Cancer Registry is a database of medical information collected from thousands of lung cancer patients. Researchers study this health data to gain a better understanding of the disease, which can ultimately lead to better outcomes for patients. By participating in the Registry, you not only will help advance lung cancer research, but you will also be able to learn about new clinical trial opportunities that may help in your own treatment program.
Learn more about the Lung Cancer Registry and how to sign up.
Lung Cancer Clinical Trials
Read questions and answers about clinical trials and see our Lung Association listing of current trials .
Download our checklist to help you talk with your doctor about clinical trials.
You can also search the Lung Cancer Clinical Trials Matching Service , provided by a partnership between the American Lung Association and EmergingMed. Patients can search for clinical trials that match their specific diagnosis and treatment history.
Find a Clinical Trial
Learn more about clinical trial programs in your area by searching our list and be sure to discuss with your doctor whether a clinical trial is right for you.
Page last updated: June 7, 2024
A Breath of Fresh Air in Your Inbox
Want updates on the latest lung health news, including COVID-19, research, inspiring stories and health information?
You will now receive email updates from the American Lung Association.
Make a Donation
Your tax-deductible donation funds lung disease and lung cancer research, new treatments, lung health education, and more.
Become a Lung Health Insider
Join over 700,000 people who receive the latest news about lung health, including research, lung disease, air quality, quitting tobacco, inspiring stories and more!
Thank you! You will now receive email updates from the American Lung Association.
Select Your Location
Select your location to view local American Lung Association events and news near you.
Change Language
Lung helpline.
Talk to our lung health experts at the American Lung Association. Our service is free and we are here to help you.
1-800-LUNG-USA
(1-800-586-4872)
Ready to start planning your care? Call us at 800-525-2225 to make an appointment.
How Four Decades of Research Led to an Important Advance in Lung Cancer
Monday, May 24, 2021
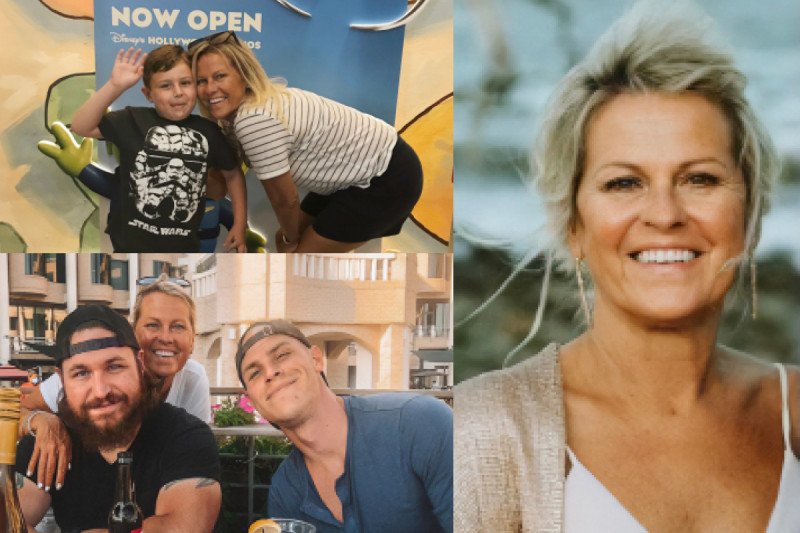
Clockwise, from upper left: Karen with her grandson, Giles, at Walt Disney World in July 2019, just before she started the trial for sotorasib; Karen at her son Zachary’s wedding in Georgia in October 2020; Karen with her sons Matthew (left) and Zachary Feiden in Washington, DC, in September 2020.
Update: On May 28, 2021, the US Food and Drug Administration granted accelerated approval to sotorasib (Lumakras TM ) for the treatment of advanced non-small cell lung cancer driven by the KRAS -G12C mutation in patients who have already received at least one other treatment. The approval was based on the clinical trials co-led by Memorial Sloan Kettering medical oncologist Bob Li.
Karen Milich got the surprise call at 7:30 on a Saturday night. It was Bob Li , her medical oncologist at Memorial Sloan Kettering, telling her that he had obtained a slot for her on a clinical trial of a brand-new experimental drug called sotorasib (AMG 510). “Dr. Li was so excited, and his excitement made me cry,” remembers Karen, who at that time had been living with advanced lung cancer for nearly a year and whose disease was continuing to spread despite other treatments.
She got up the next day, rented a car, and — together with her sister, brother-in-law, and nephew — drove 20 hours from her home in Florida to New York City. She arrived at Dr. Li’s office at 11:00 on Tuesday morning. About a week later, she started taking the drug.
That was August 2019. Since that time, Karen’s cancer has melted away. “I wake up every morning and take my AMG, just like other people take a daily aspirin,” says Karen, who previously had received chemotherapy, radiation, and immunotherapy. “I don’t feel any side effects from it at all.”
A Small Pill with a Big Story
Sotorasib looks like any other pill, but it represents a breakthrough in cancer science. In fact, the US Food and Drug Administration officially granted it a Breakthrough Therapy designation in December 2020. This means the drug has demonstrated substantial improvement over standard treatment and may be close to receiving approval for use beyond clinical trials.
A targeted therapy , sotorasib blocks a cancer-causing protein that results from a mutation in a gene called KRAS (pronounced “kay-rass”). KRAS , initially discovered in 1982 by scientists at the National Cancer Institute and multiple other academic centers, was one of the first cancer genes ever found. Mutations in KRAS and two related genes, HRAS and NRAS , are found in about 20% of all cancers.
Yet despite decades of research, scientists kept hitting roadblocks. That’s because the protein’s smooth, round shape lacked notches or grooves where drugs could attach. The mutant protein eventually was given a label by scientists: undruggable.
In the early 2000s, molecular testing for lung cancer started becoming commonplace. If doctors found certain mutations in patients’ tumors, they could prescribe drugs to go after those mutations. Finding a KRAS mutation in a tumor was like drawing the short straw: It meant that the promising targeted therapies that were being developed for other cancer genes would not work.
Looking for Better Treatments
When Karen was first diagnosed in the fall of 2018, receiving a drug to target her KRAS mutation was not an option. She initially was given chemotherapy and radiation at MSK Westchester .
After staying with her mother-in-law in New York for several months while receiving treatment, Karen was ready to return to her home in Florida. Dr. Li arranged for her see a doctor at the Miami Cancer Institute, where she received an immunotherapy drug. (The Miami Cancer Institute is a member of the MSK Cancer Alliance .)
Her cancer continued to grow. It spread to the peritoneum, which is the lining of the abdomen. At that point, she felt like she was running out of options. That’s when she learned she may be a candidate for the sotorasib trial.
Leading the Way in Lab Research
The trial came about thanks to years of hard work, much of it done at MSK. In a paper published in Science in 2016, MSK physician-scientists Piro Lito and Neal Rosen showed how it was possible to target KRAS in cancer cells. Their research built on early molecules that were originally developed by Kevan Shokat at University of California, San Francisco. These compounds inhibit the most common form of mutated KRAS in lung cancer called KRAS- G12C , which is found in about one in eight non-small cell lung cancers — including Karen’s.
Dr. Lito is a member of MSK’s Human Oncology and Pathogenesis Program and also is taking care of patients on the sotorasib trial. He’s played a key role in the development of these inhibitors, including a study published in Nature in early 2020 that showed on the molecular level why so many patients develop resistance to sotorasib and similar drugs as well as ways to overcome it.
“The clinical trials for KRAS inhibitors represent the efforts of many institutions,” Dr. Lito says. “But what really sets MSK apart in this area is the combination of preclinical and clinical development focused on understanding how these drugs work and the best way to administer them to patients.”
A Milestone for People with Lung Cancer
Today, scans show no sign of cancer in Karen’s lungs or anywhere else. In addition, liquid biopsies show no evidence of the cancer-causing mutation in her blood. Although many other patients in the trial eventually developed resistance to sotorasib, Karen has not. But if she does, MSK has additional trials under way that combine sotorasib with other drugs to overcome that resistance, based largely on Dr. Lito and Dr. Li’s research. MSK is also participating in trials of other drugs that target KRAS- G12C, currently led by medical oncologists Gregory Riely and Kathryn Arbour .
“Karen’s got a remarkable story, but she’s not the only one,” says Dr. Li, who is a member of MSK’s Early Drug Development Service , which focuses on early-stage clinical trials. “It’s a testament to what a milestone this is, to be able to target this protein that was previously considered to be really bad news.”
Karen, now 59, still lives in Florida, but since she started on the trial, she’s been staying in the New York City area. Because of her cancer diagnosis and the COVID-19 pandemic, she’s had to step back from her job as a restaurant manager. But that’s given her more time to spend with her 7-year-old grandson, Giles, who she calls “the apple of my eye and the love of my life.” This summer, they’ll be spending the entire month of July together, which has become a family tradition. “I’m thankful to God every day for Dr. Li, Sloan Kettering, and the trial,” Karen says. “They’re all incredible.”
She adds: “I’m also thankful for my whole family who supported me throughout treatment, especially my two sons.”
Dr. Li has served as an uncompensated advisor to Amgen, Genentech, Boehringer Ingelheim, Lilly, AstraZeneca, Daiichi Sankyo, and has received consulting fees from Guardant Health and Hengrui Therapeutics. He has received research grants to his institution from Amgen, Genentech, AstraZeneca, Daiichi Sankyo, Lilly, Illumina, GRAIL, Guardant Health, Hengrui Therapeutics, MORE Health, and Bolt Biotherapeutics. He has received academic travel support from Resolution Bioscience, MORE Health, and Jiangsu Hengrui Medicine. He is an inventor on two institutional patents at MSK (US62/685,057 and US62/514,661) and has intellectual property rights as a book author at Karger Publishers and Shanghai Jiao Tong University Press. Dr. Lito has served as a scientific advisor to Revolution Medicines and Black Diamond Therapeutics, and he has received grants to his institution from Amgen, Mirati, Revolution Medicines, Boehringer Ingelheim, and Vitrac Pharmaceuticals.
Related topics:

Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
Lung cancer
- Lung cancer is the leading cause of cancer-related deaths worldwide, accounting for the highest mortality rates among both men and women.
- Smoking is the leading cause of lung cancer, responsible for approximately 85% of all cases.
- Lung cancer is often diagnosed at advanced stages when treatment options are limited.
- Screening high risk individuals has the potential to allow early detection and to dramatically improve survival rates.
- Primary prevention (such as tobacco control measures and reducing exposure to environmental risk factors) can reduce the incidence of lung cancer and save lives.
Lung cancer is a type of cancer that starts when abnormal cells grow in an uncontrolled way in the lungs. It is a serious health issue that can cause severe harm and death.
Symptoms of lung cancer include a cough that does not go away, chest pain and shortness of breath.
It is important to seek medical care early to avoid serious health effects. Treatments depend on the person’s medical history and the stage of the disease.
The most common types of lung cancer are non-small cell carcinoma (NSCLC) and small cell carcinoma (SCLC). NSCLC is more common and grows slowly, while SCLC is less common but often grows quickly.
Lung cancer is a significant public health concern, causing a considerable number of deaths globally. GLOBOCAN 2020 estimates of cancer incidence and mortality produced by the International Agency for Research on Cancer (IARC) show as lung cancer remains the leading cause of cancer death, with an estimated 1.8 million deaths (18%) in 2020.
Smoking tobacco (including cigarettes, cigars, and pipes) is the primary risk factor for lung cancer but it can also affect non-smokers. Other risk factors include exposure to secondhand smoke, occupational hazards (such as asbestos, radon and certain chemicals), air pollution, hereditary cancer syndromes, and previous chronic lung diseases.
Lung cancer can cause several symptoms that may indicate a problem in the lungs.
The most common symptoms include:
- cough that does not go away
- shortness of breath
- coughing up blood (haemoptysis)
- weight loss with no known cause
- lung infections that keep coming back.
Early symptoms may be mild or dismissed as common respiratory issues, leading to delayed diagnosis.
Not smoking tobacco is the best way to prevent lung cancer.
Other risk factors to avoid include:
- secondhand smoke
- air pollution
- workplace hazards like chemicals and asbestos.
Early treatment can prevent lung cancer from becoming worse and spreading to other parts of the body.
Prevention of lung cancer include primary and secondary prevention measures. Primary prevention aims to prevent the initial occurrence of a disease through risk reduction and promoting healthy behaviour. In public health, these preventive measures include smoking cessation, promoting smoke-free environments, implementing tobacco control policies, addressing occupational hazards, and reducing air pollution levels.
Secondary prevention for lung cancer involves screening methods that aim to detect the disease in its early stages, before symptoms become apparent and can be indicated for high-risk individuals. In this population, early detection can significantly increase the chances of successful treatment and improve outcomes. The primary screening method for lung cancer is low-dose computed tomography (LDCT).
Diagnostic methods for lung cancer include physical examination, imaging (such as chest X-rays, computed tomography scans, and magnetic resonance imaging), examination of the inside of the lung using a bronchoscopy, taking a sample of tissue (biopsy) for histopathology examination and definition of the specific subtype (NSCLC versus SCLC), and molecular testing to identify specific genetic mutations or biomarkers to guide the best treatment option.
Treatment and care
Treatments for lung cancer are based on the type of cancer, how much it has spread, and the person’s medical history. Early detection of lung cancer can lead to better treatments and outcomes.
Treatments include:
- radiotherapy (radiation)
- chemotherapy
- targeted therapy
- immunotherapy.
Surgery is often used in the early stages of lung cancer if the tumour has not spread to other areas of the body. Chemotherapy and radiation therapy can help shrink the tumour.
Doctors from several disciplines often work together to provide treatment and care of people with lung cancer.
Supportive care is important for people with lung cancer. It aims to manage symptoms, provide pain relief, and give emotional support. It can help to increase quality of life for people with lung cancer and their families.
Stages of care
a) Early stage disease : The primary treatment for early stage lung cancer (i.e. tumour limited to the lung, with no metastatic dissemination to distant organs or lymph nodes) is surgical removal of the tumour through procedures such as lobectomy, segmentectomy, or wedge resection. Neoadjuvant therapy (chemotherapy and/or radiation therapy before surgery) can help reduce tumour size, making it more manageable for surgical removal. Adjuvant treatment (chemotherapy and/or radiation therapy) is very often recommended after surgery to reduce the risk of cancer recurrence. In cases where surgery is not feasible, radiation therapy or stereotactic body radiation therapy (SBRT) may be used as the primary treatment. Targeted therapy and immunotherapy may also be considered based on specific tumour characteristics. Individualized treatment plans should be discussed with healthcare professionals.
b) Advanced disease: The treatment for metastatic stage lung cancer, where the cancer has spread to distant organs or lymph nodes, is based on various factors, including the patient's overall health, the extent and location of metastases, histology, genetic profile, and individual preferences. The primary goal is to prolong survival, alleviate symptoms, and improve quality of life. Systemic therapies, such as chemotherapy, targeted therapy, and immunotherapy, play a crucial role in the treatment of metastatic lung cancer.
Chemotherapy is often the first-line treatment for the majority of patients around the world and involves the use of drugs that circulate throughout the body to kill cancer cells. Combination chemotherapy regimens are commonly used, and the choice of drugs depends on factors such as the histological type of the cancer and the patient's general health conditions. Targeted therapy, designed to block the signalling pathways that drive the growth of cancer cells, is an important option for patients with specific genetic mutations or biomarkers identified in their tumour. Immunotherapy, specifically immune checkpoint inhibitors, has revolutionized the treatment of metastatic lung cancer. These drugs help to stimulate the immune system to recognize and attack cancer cells. Local treatments, such as radiation therapy and surgery, may be used to manage specific metastatic sites or alleviate symptoms caused by tumour growth.
Clinical Trials
Clinical trials offer opportunities to access novel treatments or experimental therapies for patients. Participation in clinical trials helps advance medical knowledge and potentially offers new treatment options.
WHO response
WHO recognizes the significant impact of lung cancer on global health and has implemented several initiatives to address the disease comprehensively. The WHO's response focuses on tobacco control, cancer prevention, early detection, and improving access to quality treatment and care. WHO supports countries in implementing evidence-based tobacco control policies, including increasing tobacco taxes, enforcing comprehensive bans on tobacco advertising, promotion, and sponsorship, and implementing strong graphic health warnings on tobacco products.
The Organization also promotes cancer prevention strategies by advocating for healthy lifestyles, including regular physical activity, a healthy diet, and minimizing exposure to environmental risk factors. Additionally, WHO supports early detection programs and encourages countries to implement screening measures for high-risk populations to detect lung cancer at earlier stages when treatment options are more effective. Last, WHO works towards ensuring access to quality treatment and care for lung cancer patients by providing technical guidance to member states, promoting equitable access to essential cancer medicines, and fostering international collaboration to share best practices and improve cancer care outcomes.
International Agency for Research on Cancer: Lung cancer
WHO's work on tobacco cessation
WHO's work on cancer
ESMO Clinical Practice Guidelines: Lung and Chest Tumours
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Lung cancer.
Faraz Siddiqui ; Sarosh Vaqar ; Abdul H. Siddiqui .
Affiliations
Last Update: May 8, 2023 .
- Continuing Education Activity
Lung cancer or bronchogenic carcinoma refers to tumors originating in the lung parenchyma or within the bronchi. It is one of the leading causes of cancer-related deaths in the United States. Since 1987, lung cancer has been responsible for more deaths in women than breast cancer. It is estimated that there are 225,000 new cases of lung cancer in the United States annually, and approximately 160,000 die because of lung cancer. It is interesting to note that lung cancer was a relatively rare disease at the beginning of the 20th century. Its dramatic rise in later decades is attributable primarily to the increase in smoking among both males and females. This activity reviews the causes, pathophysiology, and presentation of lung cancer and highlights the role of the interprofessional team in its management.
- Describe the pathophysiology of lung cancer.
- Review the causes of lung cancer.
- Summarize the different types of lung cancers.
- Outline the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by lung cancer.
- Introduction
Lung cancer or bronchogenic carcinoma refers to tumors originating in the lung parenchyma or within the bronchi. It is one of the leading causes of cancer-related deaths in the United States. Since 1987, lung cancer has been responsible for more deaths in women than breast cancer. It is estimated that there are 225,000 new cases of lung cancer in the United States annually, and approximately 160,000 people die because of lung cancer. It is interesting to note that lung cancer was a relatively rare disease at the beginning of the 20th century. Its dramatic rise in later decades is mostly attributable to the increase in smoking among both males and females. [1] [2]
Smoking is the most common cause of lung cancer. It is estimated that 90% of lung cancer cases are attributable to smoking. [3] The risk is highest in males who smoke. The risk is further compounded with exposure to other carcinogens, such as asbestos. There is no correlation between lung cancer and the number of packs smoked per year due to the complex interplay between smoking and environmental and genetic factors. The risk of lung cancer secondary to passive smoking increases by 20 to 30%. [3] Other factors include radiation for non-lung cancer treatment, especially non-Hodgkins lymphoma and breast cancer. [4] Exposure to metals such as chromium, nickel, arsenic, and polycyclic aromatic hydrocarbons is also associated with lung cancer. Lung diseases like idiopathic pulmonary fibrosis increase the risk of lung cancer independent of smoking. [5]
Asbestos and radon are established risk factors for lung cancer as well. Asbestos exposure, particularly occupational exposure, increases the risk for lung cancer in a dose-dependent manner but varies according to the type of asbestos fiber. Nonoccupational asbestos exposure risk is less defined. However, the United States Environmental Protection Agency (EPA) has set standards for low-level acceptable nonoccupational asbestos exposure, stating that the health risk to occupants of a building in which asbestos is undisturbed without respirable particles is not significant. [6] Radon exposure in uranium miners was associated with a small but significant risk of lung cancer. [7] Radon has also been shown to accumulate in homes as a decay product of uranium and radium. A meta-analysis of European studies reported appreciable hazards from residential radon, particularly for smokers, and was responsible for approximately 2% of all deaths from lung cancer in Europe. [8]
- Epidemiology
Lung cancer is the most commonly diagnosed cancer worldwide, accounting for approximately 12.4% of all cancers diagnosed worldwide, and is the leading cause of cancer-related deaths. [9] The American Cancer Society estimates an annual incidence of more than 234,000 new lung cancer cases and over 154,000 lung cancer-associated deaths in the United States. [9] According to the Global Cancer Statistics report from 2020, lung cancer remained the leading cause of cancer death worldwide, with an estimated 1.8 million deaths. [10]
Historically, the lung cancer epidemic seems to involve the developed world only. Recent data suggest that the incidence of lung cancer is dramatically rising, with nearly half of new cases, 49.9%, diagnosed in the underdeveloped world. [11] In the United States, mortality is high in men compared to women. Overall, there is no racial difference in the incidence of lung cancer, but the age-adjusted mortality rate is higher in African American males than their Caucasian counterparts. No such distinction exists between women. [3]
- Pathophysiology
The pathophysiology of lung cancer is very complex and incompletely understood. It is hypothesized that repeated exposure to carcinogens, such as cigarette smoke leads to dysplasia of lung epithelium. If the exposure continues, it leads to genetic mutations and affects protein synthesis. [12] This, in turn, disrupts the cell cycle and promotes carcinogenesis. The most common genetic mutations responsible for lung cancer development are MYC , BCL2 , and p53 for small cell lung cancer (SCLC) and EGFR , KRAS , and p16 for non-small cell lung cancer (NSCLC). [13] [14]
Histopathological classification of lung cancers is based on cellular and molecular subtypes, which is an essential part of diagnosing and managing lung cancers. The 2021 World Health Organization (WHO) classification system of lung tumors divides the lung cancers as follows:
- Precursor glandular lesions
- Adenocarcinomas
- Adenosquamous carcinomas
- Squamous precursor lesions
- Squamous cell carcinomas
- Large cell carcinomas
- Sarcomatoid carcinomas
- Lung neuroendocrine neoplasms
- Salivary gland-type tumors
- Neuroendocrine tumors
- Neuroendocrine carcinomas
- And other epithelial tumors
According to the WHO, identifying histologic features, measuring the depth of invasion, and mode of spread is of prognostic value. For example, they state that tumor spread through air spaces is associated with a higher recurrence rate after limited resections and should be reported on pathological evaluation. Also, the previously described clear cell, rhabdoid, and signet ring subtypes have been discontinued by the most recent WHO classification as they appear to be cytologic features that can occur in any adenocarcinomas. The WHO classification places significant emphasis on immunohistochemical staining to classify cancers that may not have typical cytologic features on light microscopy. In the 2015 WHO classification system, poorly differentiated carcinomas were reclassified as squamous cell carcinomas if they had p40 expression; as adenocarcinomas with solid subtype if they had thyroid transcription factor 1 expression; and neuroendocrine carcinomas if they had chromogranin and synaptophysin positivity.
Precursor Glandular Lesions
These include atypical adenomatous hyperplasia (AAH) and adenocarcinoma in situ. AAH is a preinvasive lesion for lung adenocarcinoma and generally measures 5 mm or less. Adenocarcinoma in situ can be mucinous or nonmucinous and is generally a localized lesion of less than or equal to 3 cm. It shows a "lepidic" growth pattern defined as growth-restricted along the alveolar structures. It is noninvasive and shows intact alveolar septae.
Adenocarcinoma
Adenocarcinoma pathology consists of either neoplastic gland formation, pneumocyte marker expression (thyroid transcription factor 1 (TTF-1) with or without napsin expression, or intracytoplasmic mucin. It is further classified based on the extent and architecture of the neoplastic gland formation as mucinous or nonmucinous. Acinar, papillary, micropapillary, lepidic, and solid are nonmucinous subtypes. Pathological identification of these subtypes is important for prognosis. Solid, micropapillary, and cribriform (a subtype of acinar nonmucinous adenocarcinoma) patterns have adverse prognostic significance. [15] Although mucinous adenocarcinomas can have papillary, micropapillary, solid, and cribriform architecture, the WHO does not make any grading recommendations for mucinous carcinomas based on the growth patterns in a tumor. Other less frequent forms of adenocarcinoma include colloid, enteric-like, lymphoepithelial, and fetal.
Minimally invasive adenocarcinoma (MIA) is a small, solitary adenocarcinoma less than or equal to 3 cm with minimal invasion (less than 5 mm) and a predominant lepidic growth pattern, resembling other similar precursor glandular lesions. If the invasion is greater than 5 mm, it is defined as lepidic-predominant adenocarcinoma. Invasive mucinous adenocarcinoma, previously described as mucinous bronchioloalveolar carcinoma, comprises mucinous lesions that cannot be classified as MIA. If more than 10% of mucinous and nonmucinous growth patterns are present, the lesion should be classified as mixed adenocarcinoma.
Adenosquamous Carcinoma
Adenosquamous carcinomas are lung tumors with more than 10% glandular and squamous components. This is an uncommon and highly aggressive lung tumor, and current recommendations propose adjuvant chemotherapy even in Stage I radically resected tumors with whole-brain postoperative prophylactic radiotherapy due to the high risk of recurrence and brain metastasis with this subtype. [16]
Squamous Cell Carcinoma
Squamous cell pathology is defined by the presence of keratin and/or intercellular desmosomes on cytology or by immunohistochemistry (IHC) evidence of p40, p63, CK5, CK5/6, or desmoglein expression. Subtypes of squamous cell carcinoma include nonkeratinizing, keratinizing, and basaloid. Squamous cell carcinomas show extensive central necrosis with resulting cavitation. Squamous cell cancers can present as Pancoast tumors and hypercalcemia. A Pancoast tumor is a tumor in the superior sulcus of the lung. The brain is the most common site of recurrence postsurgery in cases of Pancoast tumors.
Large Cell Carcinoma
Large cell carcinoma (LCC) is a malignant epithelial neoplasm that does not have cytologic features consistent with glandular, squamous, or neuroendocrine cancers. They do not typically express p40 and TTF-1 on immunohistochemistry and lack cytologic features of small cell carcinoma. Typically LCC is comprised of round to polygonal cells with prominent nucleoli. The cells are large with abundant cytoplasm that does not have any defining features. LCC is a diagnosis of exclusion. [17]
Sarcomatoid Carcinoma
These are rare carcinomas that exhibit malignant epithelial components and features that suggest sarcomas. Subtypes include pleomorphic carcinoma, carcinosarcoma, and pulmonary blastoma.
Small Cell Carcinoma
Small cell carcinoma (SCLC) is composed of round, oval, or angulated cells, with a small amount of cytoplasm and size roughly that of a resting lymphocyte. No distinct nucleoli are seen. SCLCs are extensively necrotic. They usually stain positive with chromogranin or synaptophysin. The WHO previously classified SCLC into three cell subtypes: oat cell, intermediate cell, and combined cell (SCLC with NSCLC component, squamous, or adenocarcinoma). However, studies have shown that such classification does not have much clinical significance or prognostic value. [18]
- History and Physical
No specific signs and symptoms exist for lung cancer. Most patients already have advanced disease at the time of presentation. Lung cancer symptoms occur due to local effects of the tumor, such as cough due to bronchial compression by the tumor due to distant metastasis, stroke-like symptoms secondary to brain metastasis, paraneoplastic syndrome, and kidney stones due to persistent hypercalcemia. [19]
Cough is present in 50 to 75% of patients with lung cancer. [2] Cough productive of large volumes of thin, mucoid secretions is seen in mucinous adenocarcinoma. In some cases, especially those with exophytic bronchial masses, a cough may signify secondary post-obstructive pneumonia. Hemoptysis is present in 15 to 30% of patients with lung cancer. [2] Chest pain is present in approximately 20 to 40% of patients with lung cancer, and dyspnea may be present in as many as 25 to 40% of the cases at the time of diagnosis. [2] These symptoms, however, may be primarily due to lung cancer or due to underlying bronchopulmonary disease.
Pleural involvement in lung cancer can manifest as pleural thickening/nodules or a malignant pleural effusion. During the course of their illness, approximately 10 to 15% of patients with lung cancer will have a malignant pleural effusion, with some showing a unilateral pleural effusion as the only presenting feature. [20] Bronchogenic carcinoma with associated ipsilateral malignant pleural effusion is considered unresectable; however, it must be noted that not all pleural effusions in patients with lung cancer are malignant. [21] A benign pleural effusion may occur due to lymphatic obstruction, post-obstructive pneumonitis, or atelectasis. If two consecutive cytology specimens are negative for malignancy in patients with bronchogenic carcinoma, surgical thoracoscopy or medical pleuroscopy is recommended to evaluate the pleural space before surgical resection of a primary lesion. [22] Medical pleuroscopy has a sensitivity of greater than 90% for detecting malignancy when present in patients with bronchogenic carcinomas. [23]
Superior vena cava syndrome with dilated neck veins, edema of the face, neck, and upper extremities, and a plethoric appearance is a common feature of small cell lung cancer. It might be the primary presentation of the disease. The chest radiograph will show widening of the mediastinum or a right hilar mass. [24] As stated above, lung cancers in the superior sulcus present as Pancoast syndrome. This presents as shoulder pain, Horner syndrome, and evidence of bony destruction, with atrophy of hand muscles.
Metastasis from lung cancer to bone is frequently symptomatic, and patients may present with bone pain at the site of metastasis in the setting of elevated serum alkaline phosphatase and hypercalcemia. Up to 20% of the patients with non-small cell lung cancer may have bone pain secondary to metastasis on initial presentation; [25] whereas the percentage is as high as 30 to 40% in patients with small-cell lung cancer. [26] Imaging usually reveals osteolytic lesions with vertebral bodies as the most common site of metastasis. Adrenal metastases also occur in lung cancer, but they are rarely symptomatic and are usually seen on staging. However, not all adrenal lesions are malignant lesions, and positron emission tomography (PET) scanning is recommended to differentiate benign from malignant adrenal lesions. [27] Brain metastasis is another common feature of lung cancer in small cell lung cancers (SCLC) and non-small cell lung cancers (NSCLC). In SCLC, brain metastases may be present in as high as 20 to 30% of the patients at diagnosis. [28] Other common sites of metastases in lung cancer include the liver, which is usually only symptomatic in advanced disease.
Paraneoplastic Syndromes Associated with Lung Cancer
Symptomatic hypercalcemia secondary to lung cancer may be due to secretion of the parathyroid hormone-related protein or due to extensive bony metastases. They present with anorexia, nausea, constipation, and lethargy as typical symptoms of hypercalcemia and have an overall poor prognosis as they tend to be associated with advanced disease. [29] The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is associated with SCLC and presents with symptoms of hyponatremia.
Neurologic paraneoplastic syndromes are immune-mediated syndromes associated with SCLC and include Lambert-Eaton myasthenic syndrome (LEMS), encephalomyelitis, limbic encephalitis, cerebellar ataxia, sensory neuropathy, and autonomic neuropathy. [30] Ectopic adrenal corticotropin production can cause Cushing syndrome and is associated with SCLC, large cell neuroendocrine carcinoma, and carcinoid tumors of the lung, and it portends a worse prognosis. [31] Other extrapulmonary clinical manifestations of lung cancers include hypertrophic pulmonary osteoarthropathy, dermatomyositis, and polymyositis.
Lung cancer is the leading cause of death in both men and women. NSCLC accounts for 85% of diagnosed lung cancer cases in the United States. [3] The overall goal is a timely diagnosis and accurate staging. As per the American College of Chest Physicians (ACCP) guidelines, the initial evaluation should be complete within six weeks in patients with tolerable symptoms and no complications. Only 26% and 8% of cancers are diagnosed at stages I and II, respectively, whereas 28% and 38% are diagnosed at stages III and IV respectively. Therefore, curative surgery is an option for only a minority of patients.
Lung cancer evaluation can be divided as:
- Radiological staging
- Invasive staging
Goals of Initial Evaluation
- Clinical extent and stage of the disease
- Optimal target site and modality of 1st tissue biopsy
- Specific histologic subtypes
- Presence of co-morbidities, para-neoplastic syndromes
- Patient values and preferences regarding therapy
Radiologic Staging
Every patient suspected of having lung cancer should undergo the following tests:
- Contrast-enhanced CT chest with extension to upper abdomen up to the level of adrenal glands
- Imaging with PET or PET-CT directed at sites of potential metastasis when symptoms or focal findings are present or when chest CT shows evidence of advanced disease.
Intravenous (IV) contrast enhancement is preferable as it may distinguish mediastinal invasion of the primary tumor or metastatic lymph nodes from vascular structures.
The significant advantage of CT is that it provides an accurate anatomic definition of the tumor within the thorax, which helps clinicians decide the optimal biopsy site.
CT can also identify the following:
- Tumor-related atelectasis
- Post obstructive pneumonitis
- Intra- or extrathoracic metastatic disease
- Co-existing lung disease
The main objective of a CT scan is to identify the extent of the tumor, its anatomical location, and the lymph node involvement. TNM staging relies heavily on lymph node involvement. Therefore, most societies in Europe and the United States agree to regard a lymph node of 1 centimeter or more in the short axis to be considered highly suspicious for malignancy. Lymph nodes can be enlarged secondary to acute inflammation, such as congestive heart failure exacerbation or recent viral infection. The overall sensitivity and specificity of CT scan to identify malignancy are 55% and 81%, respectively. Hence, CT is not a good test for lung cancer staging.
Radiological Groups
The American College of Chest Physicians (ACCP) has proposed grouping patients based on tumor extent and lymph node involvement. Although CT is not the right staging tool, it helps the clinician select the site for tissue biopsy. In other words, based on these groups, further staging via non-invasive or invasive methods is planned.
- Patients with bulky tumors encircling/invading mediastinal structures cannot distinguish remote lymph nodes from the primary tumor.
- Mediastinal invasion is implied; therefore, no need for LN sampling. Tissue diagnosis suffices.
- Patients with discrete lymph node enlargement greater than 1 centimeter such that an isolated lymph node can be distinguished from the primary tumor
- Lymph node sampling is required for pathologic confirmation before curative intent therapy.
- Patients with a central tumor and an elevated risk of nodal disease despite normal-sized nodes, such as a high risk for N2/N3 disease.
- Lymph node sampling is needed even if CT/PET is negative due to a high N2/N3 disease risk.
- Patients with low risk of N2/N3 involvement or distant metastatic disease, such as peripheral T1 tumors.
- Invasive testing is not done routinely except if suspicion of N1 disease is high or the patient is not a candidate for surgery but going for stereotactic body radiation therapy (SBRT).
PET scanning allows in vivo determination of metabolic and pathologic processes. It provides limited anatomic resolution but provides information on the primary tumor's metabolic activity, mediastinal involvement, and potential distant metastases. The new integrated PET/CT scanners have eliminated the problem of unclear anatomy. The primary advantage of PET scanning is that it has reduced the number of futile thoracotomies by accurately identifying metastasis and thus excluding curative surgery as an option. PET scan is also helpful in excluding recurrent tumors after initial therapy. It also can identify recurrence versus metabolic changes post radiation therapy. False positives occur in patients with active infection and inflammation with increased glycolysis. In cases of recent lymph node sampling, a PET scan may be falsely positive. False-negative PET scans occur when there is impaired blood flow and low metabolic activity, such as with carcinoid tumors and some adenocarcinomas, and smaller lymph nodes.
PET scan has a sensitivity of 80% and specificity of 88%, which is higher than CT but not sufficient to stage lung cancer independently. Therefore, the ACCP recommends that a positive PET does not obviate the need for lymph node sampling except for group A disease.
Invasive Staging [32]
After CT and PET scans, the next step is to obtain tissue or pathologic confirmation of malignancy, confirm the staging and histological differentiation of cancer. One of the following procedures achieves this.
- Bronchoscopic endobronchial ultrasound-transbronchial needle aspiration (TBNA)
Endoscopic-TBNA
Mediastinoscopy
- Thoracoscopy or video-assisted thoracoscopy(VATS)
A CT-guided transthoracic biopsy is an option for peripheral lesions with a low risk of pneumothorax. Certain older procedures, such as the Chamberlain procedure, are sometimes required. [33]
Bronchoscopic TBNA
- Convex probe-endobronchial ultrasound-guided (CP-EBUS)-TBNA
- Radial probe-EBUS-TBNA (RP-EBUS)
- Navigation bronchoscopy
CP-EBUS Bronchoscopy
This is a bronchoscopic technique in which a miniature convex ultrasound of 7.5 MHZ is attached to the tip of the bronchoscope. It provides direct visualization of structures in the mediastinum or lung parenchyma through the bronchial wall. A biopsy is performed in real-time. It is mainly used to sample the mediastinal and hilar lymph nodes. The image can be frozen and measured, and there is also a Doppler available to identify blood vessels. It is the procedure of choice for this purpose. CP-EBUS is also the procedure of choice postinduction chemotherapy before surgery to confirm complete remission. CP-EBUS can be used to sample upper and lower paratracheal nodes as well as stations 10, 11, and 12. Stations 3, 5, and 6 are not accessible via CP-EBUS.
RP-EBUS Bronchoscopy
Instead of a convex probe, there is a miniature (20 to 30 MHz) probe. The advantages are that smaller lesions or more peripheral lesions can be reached, and it provides a 360-degree view of lung parenchyma. A real-time biopsy cannot be performed.
Navigation Bronchoscopy
The concept is to construct a navigational map of airways using either a CT scan or an electromagnetic field. After the map is constructed, the software creates the path to reach the location of the nodule. The bronchoscopist can create the pathway, and the software then navigates the bronchoscopist to the biopsy site.
Endoscopic ultrasonography (EUS) is becoming an increasingly useful tool for diagnosing and staging lung cancer. It can sample lymph nodes through the esophageal wall and provides a real-time sampling of stations 2, 4, 7, 8, and 9. The latter two stations cannot be sampled by endobronchial ultrasound (EBUS). It has the same sensitivity and specificity as EUS, 89%, and 100% respectively. There is also a growing trend to combine EBUS and EUS as minimally invasive lung cancer staging techniques. [33]
Mediastinoscopy was formerly the gold standard for lung cancer diagnosis and staging. It is mainly used to sample lymph nodes after negative needle technique and when the patient is still at high risk for cancer due to lymph node size or FDG uptake on a PET scan. Most commonly, para-tracheal lymph nodes are sampled. Alternatively, an anterior mediastinoscopy (Chamberlain procedure) can be performed to access subaortic and para-aortic nodes, stations 5 and 6, respectively. Mediastinoscopy has a sensitivity of 78% and specificity of 100%. Like all surgical procedures, mediastinoscopy has some risks. General anesthesia is required, and the procedure carries a mortality risk of 0.08%. [32] [34]
Thoracoscopy
Traditionally, thoracoscopy was performed by dividing the ribs and opening the chest cavity. Like laparoscopic surgery, it has largely replaced open abdominal surgeries. Video-assisted thoracoscopy surgery (VATS) has replaced thoracoscopy. It is used to treat several chest wall, pleural, pulmonary, and mediastinal conditions. Mediastinal lymph node sampling and full dissection during lung resection for cancer can be performed with VATS. A newer version of VATS is called RATS (robotic-assisted thoracoscopy). There are no trials comparing VATS and RATS for mediastinal lymph node biopsy.
- Treatment / Management
Treatment of Non-Small Cell Lung Cancer (NSCLC)
Surgery is the mainstay of treating stage 1 NSCLC. The procedure of choice is either lobectomy or pneumonectomy with mediastinal lymph node sampling. The 5-year survival is 78% for IA and 53% for IB disease. In patients who do not have the pulmonary reserve to tolerate pneumonectomy or lobectomy, a more conservative approach with wedge resection or segmentectomy can be done. The disadvantage is a higher local recurrence rate, but survival is the same. Local postoperative radiation therapy or adjuvant chemotherapy has not been shown to improve outcomes in stage I disease.
The survival of stage IIA and IIB lung is 46% and 36%, respectively. The preferred treatment is surgery followed by adjuvant chemotherapy. If the tumor has invaded the chest wall, then an en-bloc resection of the chest wall is recommended. Pancoast tumor is a unique tumor of stage II. It arises from the superior sulcus and is usually diagnosed at a higher stage, IIB or IIIA. The treatment of choice in cases of Pancoast tumor is neoadjuvant chemotherapy, usually with etoposide and cisplatin and concurrent radiotherapy followed by resection. Overall survival is 44% to 54% depending on postsurgery presence or absence of microscopic disease in the resected specimen.
This is the most heterogeneous group, consisting of a wide variety of tumor invasion and lymph node involvement.
In stage IIIA disease with N1 lymph nodes, surgery with curative intent is the treatment of choice. Unfortunately, a significant number of patients are found to have an N2 disease at the time of resection. The current consensus is to perform surgery as planned, followed by adjuvant chemotherapy. There is no agreement on treatment for patients with stage IIIA tumors with N2/N3 lymph nodes. If the patient has good performance status and no weigh-loss, then concurrent chemo-radiotherapy affords the best outcome. However, concurrent chemo-radiotherapy is not as tolerated and can cause severe esophagitis. Sequential therapy is better tolerated. Survival is 40% to 45% in the first two years, but five-year survival is only 20%.
T4 tumors are usually treated exclusively with chemoradiation. Surgery may be an option in T4 N0-1 tumors with carinal involvement. The operative mortality of carinal resection is 10% to 15%, and survival is approximately 20%. If a tumor is T4 due to ipsilateral nonprimary lobe nodules with no mediastinal involvement, then surgery alone renders five-year survival of 20%
Stage IIIB tumors are treated the same way unresectable IIIA cancers are treated, with concurrent chemo-radiotherapy. For a select few patients, post-induction chemo-radiotherapy, surgery might be an option. The trials on the survival of patients with IIIB tumors also included inoperable IIIA tumors; therefore, the survival in IIIB patients is unknown.
Stage IV disease is considered incurable, and therapy is aimed at improving survival and alleviating symptoms. Only 10% to 30% of patients respond to chemotherapy, and only 1% to 3% survive five years after diagnosis. Single or double drug-based chemotherapy is offered to patients with functional performance status. There is a small survival benefit from chemotherapy.
In highly select patients, non-squamous NSCLC without brain metastasis or hemoptysis might benefit from the addition of bevacizumab, a vascular endothelial growth factor (VEGF) inhibitor. [35]
Targeted Therapy for NSCLC
In the early 2000s, researchers discovered that specific mutations encode critical proteins for cell growth and replication. These mutations were named “driver mutations.” It was proposed that blocking these mutation pathways may improve survival in lung cancer patients. The current practice is to check for the following mutations in every advanced NSCLC. Each of these mutations has a specific inhibitor available:
- EGFR (epidermal growth factor receptor) is a mutation inhibited by tyrosine kinase inhibitors erlotinib, gefitinib, and afatinib. [36]
- ALK (Anaplastic lymphoma kinase) includes the specific inhibitors crizotinib, ceritinib, and alectinib. A structurally similar mutation is ROS-1. The FDA recently approved crizotinib for treating cancers expressing ROS-1 mutation.
Immunotherapy for NSCLC
Immunotherapy boosts the immune system and helps it recognize cancer cells as foreign, and increases their responsiveness. There are several check-points to decrease autoimmunity and autodestruction of the body’s cells by the immune system. Malignant cells co-opt these check-points and create tolerance in the immune system. Of these check-points, programmed-death receptor 1 (PD-1) has been of particular interest recently. PD-1 plays an important role in down-regulating T-cells and promotes self-tolerance. However, it also renders the immune system less effective against tumor cells. PD-1 interacts with two proteins: PD-L1 and PD-L2. This binding results in the inactivation of activated T-cells. At the moment, there are antibodies approved for PD-1 and its ligand, PD-L1 only. They inhibit the PD-1 receptor directly or bind to PD-L1, thus preventing it from inactivating the activated T-cell.
Nivolumab is an IgG4 monoclonal antibody against PD-1. It is approved by the FDA for squamous and non-squamous NSCLC that has progressed after platinum-based chemotherapy. It can be used in patients with high or low PD-L1 expression status. Pembrolizumab is also an IgG4 monoclonal antibody against PD-1. It is approved for pre-treated metastatic NSCLC with greater than 50% expression of PD-L1 and does not harbor EGFR and ALK mutations. It is also combined with pemetrexed and carboplatin for metastatic non-squamous NSCLC with less than 50% expression of PD-L1. Atezolizumab is an IgG1 antibody against PD-L1. It is approved for use in metastatic, progressive NSCLC during or following treatment with platinum-based chemotherapy. It can be used in patients who express EGFR and ALK mutations and fail targeted therapy. Bevacizumab is not considered immune therapy. It is an anti-angiogenesis antibody that inhibits vascular endothelial growth factor A (VEGF-A). It is primarily used in combination with platinum-based chemotherapy to treat non-squamous NSCLC. It is contraindicated in squamous cell NSCLC due to the risk of severe and often fatal hemoptysis. It is also used to treat breast, renal, colon, and brain cancers. [37] [13]
Small Cell Lung Cancer Treatment
SCLC is very sensitive to chemotherapy, but unfortunately, has a very high recurrence rate. Treatment for SCLC is according to the stage of the disease.
Treatment of Limited-stage Small Cell Lung Cancer
Stage I limited-stage small cell lung cancer (LS-SCLC) is lobectomy followed by adjuvant chemotherapy. These include SCLC presenting as peripheral nodules without mediastinal or hilar lymphadenopathy. Care should be taken in completely ruling out lymph node involvement. This is done by PET-CT followed by lymph node sampling by EBUS bronchoscopy or mediastinoscopy even if PET-CT was negative for lymph node size or FDG uptake.
LS-SCLC with mediastinal or hilar lymph node involvement is 4 to 6 cycles of chemotherapy followed by radiation therapy. Radiation therapy is indicated to avoid recurrence since nearly 80% of SCLC will recur locally without radiation therapy. There are multiple approaches to treatment, including concurrent and alternate chemo-radiotherapy or sequential treatments. Concurrent and alternative paths have slightly better outcomes, although they are more toxic than other approaches. Sequential therapy is much better tolerated.
In patients who achieve remission, prophylactic whole brain radiation is also done. This significantly reduces symptomatic brain metastasis and increases overall survival.
Treatment of Extensive-stage Small Cell Lung Cancer (ES-SCLC)
Extensive stage small cell lung cancer (ES-SCLC) includes distant metastasis, malignant pleural or pericardial effusions, contralateral hilar, or supraclavicular lymph node involvement. Treatment is with platinum-based chemotherapy. Up to 50% to 60% of patients show remission and should be offered radiation therapy followed by prophylactic whole-brain irradiation. Median survival from the time of diagnosis of ES-SCLC is only 8 to 13 months, and only about 5% of patients survive two years postdiagnosis.
- Differential Diagnosis
- Bacterial pneumonia
- Mycoplasmal pneumonia
- Pleural effusion
- Pneumothorax
- Tuberculosis
- Viral pneumonia
- Fungal pneumonia
Lung Cancer Staging
After a lung cancer diagnosis, the most crucial step is to stage the disease because the state dictates treatment options, morbidity, and survival. It is of paramount importance that this is done with utmost vigilance. Staging is primarily done for NSCLC using the TNM classification. SCLC also can be staged in the same way, but a much more straightforward approach is used for limited disease and extensive disease.
Tumor, node, metastasis staging of non-small cell lung cancer
Tumor (T), node (N), and metastasis (M) is internationally accepted way of staging NSCLC. It is comprehensive in defining tumor size and extent, location, and distant spread, which helps clinicians draw meaningful conclusions regarding the best treatment, avoid unnecessary surgeries and provide a timely referral to palliative care if the cure is not an option. The most recent TNM classification is the eighth edition, and it is effective in the United States from January 1, 2018. Outside the United States, it was accepted on January 1, 2017, by the Union of International Cancer Control (UICC).
For the eighth edition, Ithe International Association of the Study of Lung Cancer (IASLC) studied and analyzed data from 16 countries, including approximately 95,000 patients from 1999 to 2010. [38]
A primary tumor is divided into five categories, and each category is then further subdivided depending on the size, location, and invasion of surrounding structures by the tumor.
- No primary tumor
- T Carcinoma in situ
T1 (less than 3 cm)
- T1mi: minimally invasive tumor
- T1a: superficial tumor confined to central airways (tracheal or bronchial wall)
- T1a: Less than 1 cm
- T1b: Greater than 1 cm but less than 2cm
- T1C: Greater than 2 cm but less than 3cm
- T2: Greater than 3 cm but less than 5 cm
- T2a: Greater than 3 cm but less than 4cm
- T2b: Greater than 4 cm but less than 5cm
- Also considered a T2 tumor if involving main bronchus but not carina, visceral pleura or causes atelectasis to the hilum.
- T3: Greater than 5 cm but less than 7 cm)
- T3 Inv: invasion of the chest wall, pericardium, or phrenic nerve
- T3 Satell: separate tumor nodules in the same lobe
- Also considered T3 tumor if involving the pericardium, phrenic nerve, chest wall, or separate tumor nodules in the same lobe
- T4: Greater than 7 cm)
- T4inv: Invading the above structures
- T4Ipsi nod: Nodules in an ipsilateral lobe
It is also considered T4 tumor if it involves the heart, esophagus, trachea, carina, mediastinum, great vessels, recurrent laryngeal nerve, spine or tumor nodules in the different ipsilateral lobe. Invasion of the diaphragm is now considered a T4 tumor compared to a T3 tumor in the seventh edition of TNM classification. [39]
Thoracic Lymph Nodes
Lung cancer staging also depends upon the extension of cancer to the lymph nodes corresponding to the primary tumor as well as the opposite hemithorax. It is imperative to rule out lymph node metastasis before attempting curative surgery. Lung resection in itself carries high morbidity and mortality. Therefore, it should not be attempted if a cure is not possible.
Historically, thoracic lymph nodes were first classified in the 1960s by Naruke. This map was accepted by North America, Europe, and Japan. Later, in the 1980s and early 90s, further refinements were made to improve imaging and invasive testing improvements. Hence, two lymph node maps gained popularity in North America.
- American thoracic society (ATS-Map)
- American Joint Committee on Cancer (AJCC). This was an adaptation of the Naruke map.
In 1996, the differences in the above two were resolved in the Mountain-Dressler modification, MD-ATS Map. It was accepted in North America but only sporadically in Europe.
The International Association of Study of Lung Cancer (IASLC) attempted to resolve the differences between the MD-ATS and the Naruke maps. The IASLC lymph node map is now the most widely accepted lymph node classification system utilized worldwide.
Thoracic lymph nodes can be divided into mediastinal or N2 and hilar or N1 lymph nodes. N2 nodes are more important because they differentiate in cancer stages and, therefore, treatment options.
Much care has been taken in defining the N2 nodes in all the lymph node maps. We will attempt to explain the classification under the broad headings of the mediastinal and hilar groups and then further explain the individual mediastinal stations per the IASLC map.
Mediastinal Lymph Nodes
They are subdivided into the following groups or stations: [40]
- Supraclavicular nodes, station 1
- Superior mediastinal nodes, station 2 to 4
- Aortic nodes, station 3
- Inferior mediastinal lymph nodes, station 4
Supraclavicular Nodes (Station 1)
It includes lower cervical, supraclavicular and sternal notch nodes. Lymph nodes are further divided into 1R and 1L, corresponding to the right and left sides of the body, respectively. The distinction between 1R and 1L is an imaginary midline of the trachea that serves as the boundary. Below station 1, the left tracheal border is considered the boundary is differentiating between right and left-sided lymph nodes.
Superior Mediastinal Lymph Nodes (Station 2 to 4)
These lymph nodes occupy the superior mediastinum, hence, named accordingly. They are further subdivided into the following groups:
Upperparatracheall (station 2R and 2L)
- 2R nodes extend to the left lateral border of the trachea.
This extends from the upper border of the manubrium to the intersection of the caudal margin of the innominate (left brachiocephalic) vein with the trachea.
- 2L nodes extend from the upper border of the manubrium to the superior border of the aortic arch. 2L nodes are located to the left of the left lateral border of the trachea
Pre-vascular (station 3A)
These nodes are not adjacent to the trachea like the nodes in station 2, but they are anterior to the vessels.
Pre-vertebral (station 3P)
Nodes not adjacent to the trachea like the nodes in station 2, but behind the esophagus, which is pre-vertebral
Lower para-tracheal (station 4R and 4L)
- 4R nodes extend from the intersection of the caudal margin of the innominate (left brachiocephalic) vein with the trachea to the lower border of the azygos vein. 4R nodes extend from the right to the left lateral border of the trachea.
- 4L nodes extend from the upper margin of the aortic arch to the upper rim of the left main pulmonary artery
Aortic Lymph Nodes (5 and 6)
This group includes:
Sub-aortic nodes (station 5)
These nodes are located lateral to the aorta and pulmonary trunk in the so-called AP window.
Para-aortic node (station 6)
These are ascending aorta or phrenic nodes lying anterior and lateral to the ascending aorta and the aortic arch.
Inferior Mediastinal Lymph Nodes (Station 7 to 9)
This group includes sub-carinal and para-esophageal nodes:
Sub-carinal nodes (station 7)
They extend in a triangular fashion from the division of carina superiorly to the lower border of the bronchus intermedius on the right and the upper border of the lower lobe bronchus on the left.
Para-esophageal nodes (station 8)
These nodes are situated adjacent to the right and left sides of the esophageal wall. Both stations 7 and 8 are located below the carina.
Pulmonary Ligament (station 9) They are located within the pulmonary ligaments extending from the inferior pulmonary vein up to the diaphragm.
Hilar Lymph Nodes (Station 10 to 14)
These are all N1 nodes. These include nodes adjacent to the main stem bronchus and hilar vessels. On the right, they extend from the lower rim of the azygos vein to the interlobar region. On the left, from the upper rim of the pulmonary artery to the inter-lobar region.
Lymph Node Classification (N)
N0: No lymph node involvement
N1: Involvement of ipsilateral hilar nodes
- N1a: single station N1 nodes
- N1b: multiple-station N1 nodes
N2: Involvement of mediastinal nodes
- N2a1: Single station N2 nodes without N1 involvement (skip metastasis)
- N2a2: Single station N2 nodes with N1 involvement
- N2b: Multiple station N2 involvement
N3: Involvement of contralateral mediastinal or hilar lymph nodes [41]
Metastasis (M)
- M0: No distant metastasis
- M1a: Malignant pleural / pericardial effusion or nodules
- M1b: Single extra-thoracic metastasis
- M2: Multiple extra-thoracic metastases
Tumor Node Metastasis Staging of Lung Cancer
Occult cancer: TX N0 M0
Primary cancer not found; no lymph node or distant metastasis.
- T is N 0 M 0
- T1mi N 0 M 0
- T1a N 0 M 0
- T1b N 0 M 0
- T1c N 0 M 0
- T2a N 0 M 0
- T2b N 0 M 0
- T1a / T1b / T1c N 1 M 0
- T2a / T2b N 1 M 0
- T1a / T2b / T2c N 2 M 0
- T2a / T2b N2 M 0
- T4 N 0 / N 1 M0
- T1a / T1b / T1c N 3 M 0
- T2a / T2b N 3 M0
- Any T / Any N M1a or M1b
- Any T / Any N M1c
Staging for all Small Cell Lung Cancer
- SCLC staging can be done using the TNM system, but since SCLC is considered a systemic disease, a more straightforward classification has been used successfully since the 1950s. There is a growing body of evidence that TNM rating may better define SCLC, but there is no consensus on this approach yet.
- SCLC is classified as LS-SCLC and ES-SCLC small cell based on the Veterans Affairs Lung study group (VALSG) classification.
- LS-SCLC is confined to the ipsilateral hemithorax and local lymph nodes, both mediastinal and hilar and supraclavicular nodes can be included in a single tolerable radiotherapy port (corresponding to TNM stages I through IIIB).
- ES-SCLC has tumors beyond the boundaries of limited disease, including distant metastases, malignant pericardial or pleural effusions, and contralateral supraclavicular and contralateral hilar involvement. [14]
Prognosis of NSCLC
The TNM stage at presentation in patients with NSCLC has the most significant impact on prognosis. A higher TNM stage correlates with advanced disease and poor outcomes. Other factors indicative of poor prognosis include performance status at the time of diagnosis, anorexia, weight loss, and the presence of liver or skin metastases. [42] Molecular studies have revealed that patients with activating mutations of EGFR in patients with adenocarcinoma have a better prognosis than those without EGFR mutations. [43]
Prognosis of SCLC
The extent of disease and the stage at presentation is the most important prognostic factor for SCLC. Patients with the limited-stage disease have a five-year survival rate of 10 to 13%, whereas patients with the extensive-stage disease have a five-year survival rate of 1 to 2%. [44] Similar to NSCLC, performance status and weight loss are independent prognostic factors for SCLC, where patients with poor performance status and/or weight loss at the time of diagnosis have a decreased survival rate.
- Complications
Complications of lung cancer such as thrombosis and paraneoplastic syndromes are discussed above. Common complications seen in patients undergoing treatment for lung cancer include:
- Chemotherapy-induced nausea and vomiting
- Weight loss
- Neutropenia
- Nephrotoxicity (especially in patients receiving cisplatin-based therapies)
- Neurotoxicities
- Deterrence and Patient Education
The single most important preventive measure is smoking cessation in all individuals. Patients should be advised about the clinical correlation of lung cancer with smoking at every clinician visit. Another important method of decreasing the morbidity and mortality associated with lung cancer is effective screening. A low-dose helical computed tomography (LDCT) is indicated for high-risk individuals for primary prevention. Smokers between the ages of 66 to 80 years benefit more from screening than those aged 55 to 64 years. [45]
Patients without a history of smoking do not benefit from lung cancer screening. Multiple other models incorporating clinical factors such as a history of lung disease, family history of lung cancer, and asbestos exposure have been developed. They can be applied to determine at-risk individuals who may benefit from screening. Current guidelines by the United States Preventive Services Task Force (2021) recommend an annual LDCT for patients aged 50 to 80 years who are at high risk of lung cancer due to their smoking history. [46] High-risk individuals are defined as those who have a greater than or equal to 20 pack-year smoking history and are either actively smoking or have quit within the past 15 years.
- Pearls and Other Issues
Palliative Care in Lung Cancer
All therapeutic options, surgery, chemotherapy, and radiation have a role in managing pain and other symptoms in terminal lung cancer patients.
Surgery results in better outcomes in patients with at least three months of expected survival and good performance status. Surgical procedures for palliation include tumor bypass procedures, partial resection of the tumor, and removal of metastasis. Surgical intervention may be beneficial in patients with lung cancer if there is airway obstruction, hemoptysis, pleural or pericardial exudate, or metastases to the brain or bone. Almost 30% of lung cancer patients experience central airway occlusion, and bronchoscopic laser destruction followed by stent placement provides immediate relief in such patients. [47] Chemotherapy helps alleviate symptoms of pain and cough and may prolong survival. Palliative radiation provides symptomatic relief in 41% to 95% of lung cancer patients. Almost 60% of lung cancer patients, regardless of type and stage, receive radiation treatments during their course of illness. Radiation plays a crucial role in alleviating pain symptoms due to metastasis, particularly brain and bone metastasis. Endoscopic treatment, such as brachytherapy, helps control symptoms due to airway narrowing. [48] [49]
- Enhancing Healthcare Team Outcomes
Despite all the advances, the outcomes for lung cancer remain abysmal. The key reason is that most patients are diagnosed with advanced-stage disease. To improve outcomes, an interprofessional team approach with close communication between the members may perhaps lead to earlier diagnosis and treatment.
Most patients with lung cancer are first seen by the primary care provider, nurse practitioner, or internist. These clinicians need to have a high suspicion of lung cancer in smokers and others with occupational exposures and order the appropriate imaging tests when indicated. Referral to a thoracic surgeon should be done on a timely basis.
The thoracic surgeon's definitive diagnosis and management plan for lung cancer are made in collaboration with the radiologist and pathologist.
After surgery, nurses usually monitor the patients for oxygenation, ventilation, and pain. Since many of these patients are smokers, they also have other comorbidities like heart disease and peripheral vascular disease, which often present with symptoms in the post-operative period. Thus, nurses must be extra vigilant for physical abnormalities and communicate with the surgeon.
After surgery, patients need prolonged rehabilitation. Some may need chemotherapy and radiation, and hence the oncology nurse should educate the patients on the procedures and protocols. The specialized oncology pharmacist should educate the patient on the chemotherapeutic drugs, their benefits, and their adverse effects. Oncology board-certified pharmacists can consult with the oncologist on the regimens for chemotherapy and the alternatives based on patient response.
Due to high incidence and mortality, there has been a worldwide interest in developing a screening program for lung cancer. A landmark study, the National Lung Screening Trial, showed an overall decrease in mortality of 6.7% with screening. Currently, lung cancer screening is offered to men and women 55 years or older who have smoked 30 pack-years or more or have quit smoking less than 15 years ago. [50] [51]
Lung cancer screening uses a low-dose helical CT scan of the chest which takes less than 25 seconds. A significant drawback of screening is the detection of benign lesions, resulting in a relatively high number of unnecessary biopsies, surgeries, or continued radiological follow-ups. [5] The key is for the interprofessional team to communicate and determine the best course of action. A collaborative interprofessional team can greatly improve clinical outcomes for this disease. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
CT image of carcinoma lung Contributed by Sunil Munakomi, MD
Disclosure: Faraz Siddiqui declares no relevant financial relationships with ineligible companies.
Disclosure: Sarosh Vaqar declares no relevant financial relationships with ineligible companies.
Disclosure: Abdul Siddiqui declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Siddiqui F, Vaqar S, Siddiqui AH. Lung Cancer. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Annual summary of vital statistics: trends in the health of Americans during the 20th century. [Pediatrics. 2000] Annual summary of vital statistics: trends in the health of Americans during the 20th century. Guyer B, Freedman MA, Strobino DM, Sondik EJ. Pediatrics. 2000 Dec; 106(6):1307-17.
- Epidemiology of lung cancer. [Semin Thorac Cardiovasc Surg. ...] Epidemiology of lung cancer. Friedberg JS, Kaiser LR. Semin Thorac Cardiovasc Surg. 1997 Jan; 9(1):56-9.
- An epidemiological study of risk factors for lung cancer in Guangzhou, China. [Lung Cancer. 1996] An epidemiological study of risk factors for lung cancer in Guangzhou, China. Du YX, Cha Q, Chen XW, Chen YZ, Huang LF, Feng ZZ, Wu XF, Wu JM. Lung Cancer. 1996 Mar; 14 Suppl 1:S9-37.
- Review Cancer, cigarette smoking and premature death in Europe: a review including the Recommendations of European Cancer Experts Consensus Meeting, Helsinki, October 1996. [Lung Cancer. 1997] Review Cancer, cigarette smoking and premature death in Europe: a review including the Recommendations of European Cancer Experts Consensus Meeting, Helsinki, October 1996. Boyle P. Lung Cancer. 1997 May; 17(1):1-60.
- Review Tobacco use and its contribution to early cancer mortality with a special emphasis on cigarette smoking. [Environ Health Perspect. 1995] Review Tobacco use and its contribution to early cancer mortality with a special emphasis on cigarette smoking. Shopland DR. Environ Health Perspect. 1995 Nov; 103 Suppl 8(Suppl 8):131-42.
Recent Activity
- Lung Cancer - StatPearls Lung Cancer - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 18 November 2020
Research round-up: lung cancer
- Bianca Nogrady
You can also search for this author in PubMed Google Scholar
Genes predict effect of immunotherapy
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 587 , S8-S9 (2020)
doi: https://doi.org/10.1038/d41586-020-03153-z
This article is part of Nature Outlook: Lung cancer , an editorially independent supplement produced with the financial support of third parties. About this content .
Related Articles

- Therapeutics
- Medical research

Breast cancer blocked by multiple natural lines of defence
News & Views 04 SEP 24

Mechanisms that clear mutations drive field cancerization in mammary tissue
Article 04 SEP 24

A pathology foundation model for cancer diagnosis and prognosis prediction

Found: a brain-wiring pattern linked to depression
News 04 SEP 24

The hepatitis C virus envelope protein complex is a dimer of heterodimers

How rival weight-loss drugs fare at treating obesity, diabetes and more
News 03 SEP 24
Blocking an inflammatory protein slows the pace of ageing
News & Views 29 JUL 24

A Trojan horse for thirsty tumours
Outlook 11 JUL 24

Faecal transplants can treat some cancers — but probably won’t ever be widely used
Outlook 04 JUL 24
Faculty Positions in School of Engineering, Westlake University
The School of Engineering (SOE) at Westlake University is seeking to fill multiple tenured or tenure-track faculty positions in all ranks.
Hangzhou, Zhejiang, China
Westlake University
Postdoctoral Associate- Genetic Epidemiology
Houston, Texas (US)
Baylor College of Medicine (BCM)
NOMIS Foundation ETH Postdoctoral Fellowship
The NOMIS Foundation ETH Fellowship Programme supports postdoctoral researchers at ETH Zurich within the Centre for Origin and Prevalence of Life ...
Zurich, Canton of Zürich (CH)
Centre for Origin and Prevalence of Life at ETH Zurich
13 PhD Positions at Heidelberg University
GRK2727/1 – InCheck Innate Immune Checkpoints in Cancer and Tissue Damage
Heidelberg, Baden-Württemberg (DE) and Mannheim, Baden-Württemberg (DE)
Medical Faculties Mannheim & Heidelberg and DKFZ, Germany
Postdoctoral Associate- Environmental Epidemiology
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
September 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Immunotherapy before and after lung cancer surgery reduces death risk and disease recurrence, research finds
by Johns Hopkins University School of Medicine

People with operable non-small cell lung cancers may fare better over the next few years by receiving immunotherapy treatments before and after surgery instead of only before surgery, according to a new analysis by Johns Hopkins Kimmel Cancer Center investigators.
For the study, researchers compared health outcomes among 147 participants in the CheckMate 816 study—in which patients received three cycles of the immunotherapy nivolumab plus chemotherapy before surgery (neoadjuvant)—with results of 139 participants in the CheckMate 77T trial, in which patients received up to four cycles of nivolumab plus chemotherapy before surgery and up to 13 cycles of nivolumab after surgery. They followed participants for up to four years following surgery.
They observed a 40% reduction in the risk of disease recurrence or death after surgery in patients who received at least one dose of nivolumab following immunotherapy/chemotherapy and surgery. A similar benefit was seen regardless of patients' baseline cancer stage.
Reductions in disease recurrence and death were also seen more in people who had less than 1% tumor expression of the protein PD-L1 (which allows cells to escape an attack by the immune system ) compared with a 1% or greater expression. Immunotherapy before and after surgery was observed to be beneficial in patients who did not achieve a complete pathological response (absence of cancer cells) from pre-surgical treatment and surgery.
These results are to be presented on Sunday, September 8, at the IASLC (International Association for the Study of Lung Cancer) 2024 World Conference on Lung Cancer in San Diego.
"There's been a big migration in lung cancer and in melanoma treatment in the last few years from doing surgery upfront and giving postoperative immunotherapy, to giving immunotherapy prior to surgery," explains Patrick Forde, M.B.B.Ch., an adjunct professor of oncology at the Johns Hopkins University School of Medicine. "But our analysis in individual patients in these two trials suggests that there is likely a further benefit from receiving additional immunotherapy treatment after surgery ."
The abstract title is "Perioperative vs. Neoadjuvant Nivolumab for Resectable NSCLC: Patient-Level Data Analysis of CheckMate 77T vs. CheckMate 816" (presentation #3589). The studies referenced in the abstract were sponsored by Bristol-Myers Squibb, manufacturer of nivolumab , and conducted at Johns Hopkins and other clinical sites.
Explore further
Feedback to editors

Low-impact yoga and exercise found to help older women manage urinary incontinence
Sep 7, 2024

Missouri patient tests positive for bird flu despite no known exposure to animals

Falling for financial scams? It may signal early Alzheimer's disease
Sep 6, 2024

Cognitive behavioral therapy enhances brain circuits to relieve depression

New molecular sensor enables fluorescence imaging for assessing sarcoma severity

Noninvasive focused ultrasound show potential for combating chronic pain

Study finds TGF-beta and RAS signaling are both required for lung cancer metastasis

Research team successfully maps the brain-spinal cord connection in humans

Alzheimer's study reveals critical differences in memory loss progression based on the presence of specific proteins

Chemical screen identifies PRMT5 as therapeutic target for paclitaxel-resistant triple-negative breast cancer
Related stories.

Pre- and post-surgical immunotherapy improves outcomes for patients with operable lung cancer, Phase III study finds
May 15, 2024

Pre- and post-surgical immunotherapy improves outcomes for patients with operable lung cancer
Oct 22, 2023

Immunotherapy plus chemotherapy before surgery improves outcomes for lung cancer patients
Apr 11, 2022

Immunotherapy after surgery found to provide significant, durable benefit for high-risk bladder patients
Feb 17, 2023

Immunotherapy after bladder cancer surgery shows excellent cancer-free survival rates
May 15, 2022

Neoadjuvant immunotherapy for early stage melanoma shows positive results
Jun 3, 2024
Recommended for you

Age-related changes in male fibroblasts increase treatment-resistant melanoma, study finds
Study finds dysfunctional white blood cells linked to heightened melanoma risk.

Researchers develop mechanism that predicts severity of aggressive form of breast cancer
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Select "Patients / Caregivers / Public" or "Researchers / Professionals" to filter your results. To further refine your search, toggle appropriate sections on or off.
Home > Patients, Caregivers, and Advocates > About Cancer > Cancers > Lung Cancer
Lung Cancer

Lung and bronchus cancer is the second most commonly diagnosed cancer among both men and women — prostate cancer is more commonly diagnosed among men, and breast cancer is more commonly diagnosed among women.
However, lung cancer is by far the most frequent cause of cancer death among both men and women because the rate of death from lung cancer is much higher than from prostate cancer or breast cancer.
According to the National Cancer Institute , approximately 234,580 people will be diagnosed with lung and bronchus cancer in the United States in 2024, and about 125,070 people will die of the disease – 65,790 men and 59,280 women. The five-year survival rate for these cancers is 26.7 percent.
There are two main forms of lung cancer – small cell lung cancer and non-small cell lung cancer.
There are several types of non-small cell lung cancer characterized by different kinds of cancer cells. The cancer cells of each type grow and spread in different ways. The most common types of non-small cell lung cancer are squamous cell carcinoma that begins in the thin, flat squamous cells; large cell carcinoma; and adenocarcinoma, which begins in the cells that line the alveoli. Other less common types of non-small cell lung cancer are: pleomorphic, carcinoid tumor, salivary gland carcinoma, and unclassified carcinoma.
There are two types of small cell lung cancer – small cell carcinoma, also called oat cell cancer, and combined small cell carcinoma.
Smoking cigarettes, pipes, or cigars is the most common cause of lung cancer. Other risk factors for lung cancer include being exposed to secondhand smoke, having a family history of lung cancer, being treated with radiation therapy to the breast or chest, exposure to asbestos, chromium, nickel, arsenic, soot, or tar in the workplace, and exposure to radon. When smoking is combined with other risk factors, the risk of lung cancer is increased.
Source: National Cancer Institute

You can support the AACR's mission by contacting your representatives and senators and advocating for increased funding for lifesaving cancer research.

Continuing the Conversation on Cancer Disparities

Living with Metastatic Lung Cancer
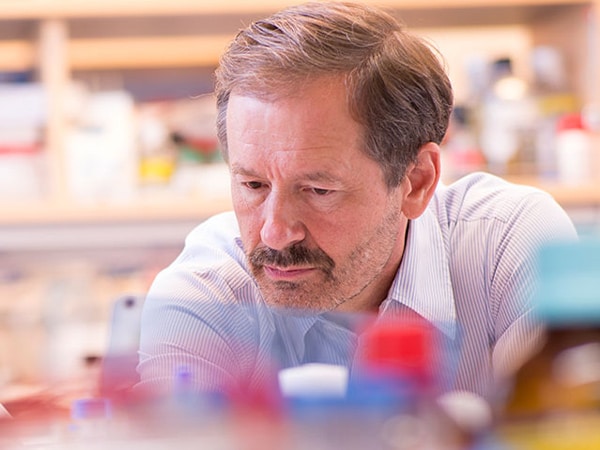
Pioneering Personalized Medicine
- Confronting Stage 3 Lung Cancer With Immunotherapy
- November is Lung Cancer Awareness Month
- Non-Small Cell Lung Cancer Treatment (PDQ®)
- Patient Care & Health Information
- Diseases & Conditions
- Lung cancer
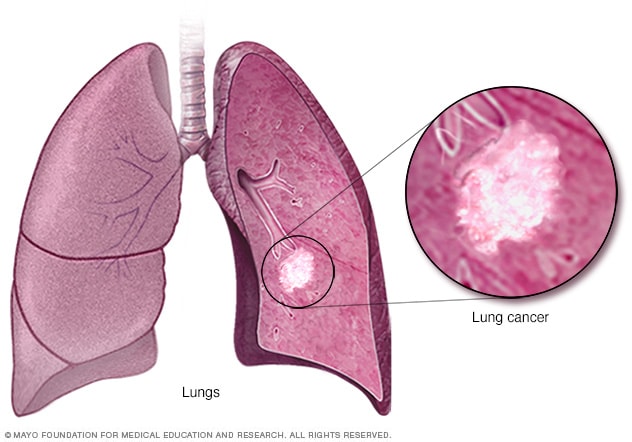
Lung cancer begins in the cells of the lungs.
Lung cancer is a kind of cancer that starts as a growth of cells in the lungs. The lungs are two spongy organs in the chest that control breathing.
Lung cancer is the leading cause of cancer deaths worldwide.
People who smoke have the greatest risk of lung cancer. The risk of lung cancer increases with the length of time and number of cigarettes smoked. Quitting smoking, even after smoking for many years, significantly lowers the chances of developing lung cancer. Lung cancer also can happen in people who have never smoked.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Lung cancer typically doesn't cause symptoms early on. Symptoms of lung cancer usually happen when the disease is advanced.
Signs and symptoms of lung cancer that happen in and around the lungs may include:
- A new cough that doesn't go away.
- Chest pain.
- Coughing up blood, even a small amount.
- Hoarseness.
- Shortness of breath.
Signs and symptoms that happen when lung cancer spreads to other parts of the body may include:
- Losing weight without trying.
- Loss of appetite.
- Swelling in the face or neck.
When to see a doctor
Make an appointment with your doctor or other healthcare professional if you have any symptoms that worry you.
If you smoke and haven't been able to quit, make an appointment. Your healthcare professional can recommend strategies for quitting smoking. These may include counseling, medicines and nicotine replacement products.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get Mayo Clinic cancer expertise delivered to your inbox.
Subscribe for free and receive an in-depth guide to coping with cancer, plus helpful information on how to get a second opinion. You can unsubscribe at any time. Click here for an email preview.
Error Select a topic
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth coping with cancer guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest about cancer news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Lung cancer happens when cells in the lungs develop changes in their DNA. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Smoking causes most lung cancers. It can cause lung cancer in both people who smoke and in people exposed to secondhand smoke. But lung cancer also happens in people who never smoked or been exposed to secondhand smoke. In these people, there may be no clear cause of lung cancer.
How smoking causes lung cancer
Researchers believe smoking causes lung cancer by damaging the cells that line the lungs. Cigarette smoke is full of cancer-causing substances, called carcinogens. When you inhale cigarette smoke, the carcinogens cause changes in the lung tissue almost immediately.
At first your body may be able to repair this damage. But with each repeated exposure, healthy cells that line your lungs become more damaged. Over time, the damage causes cells to change and eventually cancer may develop.
Types of lung cancer
Lung cancer is divided into two major types based on the appearance of the cells under a microscope. Your healthcare professional makes treatment decisions based on which major type of lung cancer you have.
The two general types of lung cancer include:
- Small cell lung cancer. Small cell lung cancer usually only happens in people who have smoked heavily for years. Small cell lung cancer is less common than non-small cell lung cancer.
- Non-small cell lung cancer. Non-small cell lung cancer is a category that includes several types of lung cancers. Non-small cell lung cancers include squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
Risk factors
A number of factors may increase the risk of lung cancer. Some risk factors can be controlled, for instance, by quitting smoking. Other factors can't be controlled, such as your family history.
Risk factors for lung cancer include:
Your risk of lung cancer increases with the number of cigarettes you smoke each day. Your risk also increases with the number of years you have smoked. Quitting at any age can significantly lower your risk of developing lung cancer.
Exposure to secondhand smoke
Even if you don't smoke, your risk of lung cancer increases if you're around people who are smoking. Breathing the smoke in the air from other people who are smoking is called secondhand smoke.
Previous radiation therapy
If you've had radiation therapy to the chest for another type of cancer, you may have an increased risk of developing lung cancer.
Exposure to radon gas
Radon is produced by the natural breakdown of uranium in soil, rock and water. Radon eventually becomes part of the air you breathe. Unsafe levels of radon can build up in any building, including homes.
Exposure to cancer-causing substances
Workplace exposure to cancer-causing substances, called carcinogens, can increase your risk of developing lung cancer. The risk may be higher if you smoke. Carcinogens linked to lung cancer risk include asbestos, arsenic, chromium and nickel.
Family history of lung cancer
People with a parent, sibling or child with lung cancer have an increased risk of the disease.
Complications
Lung cancer can cause complications, such as:
Shortness of breath
People with lung cancer can experience shortness of breath if cancer grows to block the major airways. Lung cancer also can cause fluid to collect around the lungs and heart. The fluid makes it harder for the affected lung to expand fully when you inhale.
Coughing up blood
Lung cancer can cause bleeding in the airway. This can cause you to cough up blood. Sometimes bleeding can become severe. Treatments are available to control bleeding.
Advanced lung cancer that spreads can cause pain. It may spread to the lining of a lung or to another area of the body, such as a bone. Tell your healthcare professional if you experience pain. Many treatments are available to control pain.
Fluid in the chest
Lung cancer can cause fluid to accumulate in the chest, called pleural effusion. The fluid collects in the space that surrounds the affected lung in the chest cavity, called the pleural space.
Pleural effusion can cause shortness of breath. Treatments are available to drain the fluid from your chest. Treatments can reduce the risk that pleural effusion will happen again.
Cancer that spreads to other parts of the body
Lung cancer often spreads to other parts of the body. Lung cancer may spread to the brain and the bones.
Cancer that spreads can cause pain, nausea, headaches or other symptoms depending on what organ is affected. Once lung cancer has spread beyond the lungs, it's generally not curable. Treatments are available to decrease symptoms and to help you live longer.
There's no sure way to prevent lung cancer, but you can reduce your risk if you:
Don't smoke
If you've never smoked, don't start. Talk to your children about not smoking so that they can understand how to avoid this major risk factor for lung cancer. Begin conversations about the dangers of smoking with your children early so that they know how to react to peer pressure.
Stop smoking
Stop smoking now. Quitting reduces your risk of lung cancer, even if you've smoked for years. Talk to your healthcare team about strategies and aids that can help you quit. Options include nicotine replacement products, medicines and support groups.
Avoid secondhand smoke
If you live or work with a person who smokes, urge them to quit. At the very least, ask them to smoke outside. Avoid areas where people smoke, such as bars. Seek out smoke-free options.
Test your home for radon
Have the radon levels in your home checked, especially if you live in an area where radon is known to be a problem. High radon levels can be fixed to make your home safer. Radon test kits are often sold at hardware stores and can be purchased online. For more information on radon testing, contact your local department of public health.
Avoid carcinogens at work
Take precautions to protect yourself from exposure to toxic chemicals at work. Follow your employer's precautions. For instance, if you're given a face mask for protection, always wear it. Ask your healthcare professional what more you can do to protect yourself at work. Your risk of lung damage from workplace carcinogens increases if you smoke.
Eat a diet full of fruits and vegetables
Choose a healthy diet with a variety of fruits and vegetables. Food sources of vitamins and nutrients are best. Avoid taking large doses of vitamins in pill form, as they may be harmful. For instance, researchers hoping to reduce the risk of lung cancer in people who smoked heavily gave them beta carotene supplements. Results showed the supplements increased the risk of cancer in people who smoke.
Exercise most days of the week
If you don't exercise regularly, start out slowly. Try to exercise most days of the week.
Lung cancer care at Mayo Clinic
- Non-small cell lung cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1450. Accessed Dec. 4, 2023.
- Small cell lung cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1462. Accessed Dec. 4, 2023.
- Niederhuber JE, et al., eds. Cancer of the lung: Non-small cell lung cancer and small cell lung cancer. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 4, 2023.
- Non-small cell lung cancer treatment (PDQ) – Patient version. National Cancer Institute. https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq. Accessed Dec. 4, 2023.
- Small cell lung cancer treatment (PDQ) – Patient version. National Cancer Institute. https://www.cancer.gov/types/lung/patient/small-cell-lung-treatment-pdq. Accessed Dec. 4, 2023.
- Lung cancer – non-small cell. Cancer.Net. https://www.cancer.net/cancer-types/lung-cancer/view-all. Accessed Dec. 4, 2023.
- Lung cancer – small cell. Cancer.Net. https://www.cancer.net/cancer-types/33776/view-all. Accessed Dec. 4, 2023.
- Detterbeck FC, et al. Executive Summary: Diagnosis and management of lung cancer, 3rd ed.: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; doi:10.1378/chest.12-2377.
- Palliative care. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1454. Accessed Dec. 4, 2023.
- Lung cancer. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/lung-cancer. Accessed Dec. 4, 2023.
- Cairns LM. Managing breathlessness in patients with lung cancer. Nursing Standard. 2012; doi:10.7748/ns2012.11.27.13.44.c9450.
- Warner KJ. Allscripts EPSi. Mayo Clinic. Jan. 13, 2020.
- Brown AY. Allscripts EPSi. Mayo Clinic. July 30, 2019.
- Searching for cancer centers. American College of Surgeons. https://www.facs.org/search/cancer-programs. Accessed Dec. 4, 2023.
- Temel JS, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. New England Journal of Medicine. 2010; doi:10.1056/NEJMoa1000678.
- Dunning J, et al. Microlobectomy: A novel form of endoscopic lobectomy. Innovations. 2017; doi:10.1097/IMI.0000000000000394.
- Leventakos K, et al. Advances in the treatment of non-small cell lung cancer: Focus on nivolumab, pembrolizumab and atezolizumab. BioDrugs. 2016; doi:10.1007/s40259-016-0187-0.
- Dong H, et al. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nature Medicine. 1999;5:1365.
- Aberle DR, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. New England Journal of Medicine. 2011; doi:10.1056/NEJMoa1102873.
- Infographic: Lung Cancer
- Lung cancer surgery
- Lung nodules: Can they be cancerous?
- Super Survivor Conquers Cancer
Associated Procedures
- Ablation therapy
- Brachytherapy
- Bronchoscopy
- Chemotherapy
- Lung cancer screening
- Positron emission tomography scan
- Proton therapy
- Radiation therapy
- Stop-smoking services
News from Mayo Clinic
- Science Saturday: Study finds senescent immune cells promote lung tumor growth June 17, 2023, 11:00 a.m. CDT
- Era of hope for patients with lung cancer Nov. 16, 2022, 03:00 p.m. CDT
- Mayo Clinic Q&A podcast: Survivorship after surgery for lung cancer Nov. 15, 2022, 01:30 p.m. CDT
- Mayo Clinic Minute: Understanding lung cancer Nov. 02, 2022, 04:00 p.m. CDT
- Lung cancer diagnosis innovation leads to higher survival rates Nov. 02, 2022, 02:30 p.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been recognized among the top Pulmonology hospitals in the nation for 2024-2025 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
For the best browsing experience please enable JavaScript. Instructions for Microsoft Edge and Internet Explorer , other browsers

- About cancer
- Get involved
- Our research
- Funding for researchers
- Cancer types
- Cancer in general
- Causes of cancer
- Coping with cancer
- Health professionals
- Do your own fundraising
- By cancer type
- By cancer subject
- Our funding schemes
- Applying for funding
- Managing your research grant
- How we deliver our research
- Find a shop
- Shop online
- Our eBay shop
- Our organisation
- Current jobs
- Cancer news
Lung cancer
Lung cancer starts in the windpipe (trachea), the main airway (bronchus) or the lung tissue. Cancer that starts in the lung is called primary lung cancer. There are different types of primary lung cancer. The most common type is non small cell lung cancer. The treatment you need depends on which type you have.
If cancer spreads to your lungs from somewhere else in your body, it is called secondary lung cancer.
- Read more about secondary lung cancer
What is lung cancer?
Lung cancer starts in the windpipe (trachea), the main airway (bronchus) or the lung tissue. Cancer that starts in the lung is called primary lung cancer.
Symptoms of lung cancer
Lung cancer doesn't always cause symptoms in its early stages. Symptoms can include a cough that won't go away, coughing up blood and breathlessness.
Getting diagnosed with lung cancer
You usually start by seeing your GP, and they might refer you to a specialist and organise tests. Or you might be referred to a specialist and further tests if screening for lung cancer or a lung health check showed that you might have lung cancer.
Survival for lung cancer
Survival depends on many factors including the stage and type of your lung cancer.
Treatment for lung cancer
Your treatment depends on several factors. These include what type of lung cancer you have, how big it is and whether it has spread (the stage). It also depends on your general health.
Stages and types of lung cancer
The stage of a cancer tells you how big it is and whether it has spread. The type tells which type of cell the cancer started from.
Metastatic lung cancer
Metastatic lung cancer means that the cancer has spread from where it started in the lung to other parts of the body. It is also called advanced lung cancer.
Research and clinical trials for lung cancer
Current research is looking at ways to improve the diagnosis and treatment of lung cancer.
Living with lung cancer
There is support available during and after treatment to help you cope. This includes support from your clinical nurse specialist, cancer charities, community services, and family and friends.
Risks and causes of lung cancer
Certain factors can increase your risk of developing lung cancer, such as smoking or exposure to certain chemicals.
It’s a worrying time for many people and we want to be there for you whenever - and wherever - you need us. Cancer Chat is our fully moderated forum where you can talk to others affected by cancer, share experiences, and get support. Cancer Chat is free to join and available 24 hours a day.
Visit the Cancer Chat forum
About Cancer generously supported by Dangoor Education since 2010.

Find a clinical trial
Search our clinical trials database for all cancer trials and studies recruiting in the UK
Cancer Chat forum
Talk to other people affected by cancer
Nurse helpline 0808 800 4040
Questions about cancer? Call freephone 9 to 5 Monday to Friday or email us
Switch language:

Data Insights
Sonidegib phosphate by sun pharma advanced research for non-small cell lung cancer: likelihood of approval.

- Share on Linkedin
- Share on Facebook
Sonidegib phosphate is under clinical development by Sun Pharma Advanced Research and currently in Phase I for Non-Small Cell Lung Cancer. According to GlobalData, Phase I drugs for Non-Small Cell Lung Cancer have an 80% phase transition success rate (PTSR) indication benchmark for progressing into Phase II. GlobalData’s report assesses how Sonidegib phosphate’s drug-specific PTSR and Likelihood of Approval (LoA) scores compare to the indication benchmarks. Buy the report here.
Smarter leaders trust GlobalData
Data insights likelihood of approval and phase transition success rate model - sonidegib phosphate in non-small cell lung cancer.
Buy the Report
The gold standard of business intelligence.
Find out more
Related Company Profiles
Sun pharma advanced research company ltd.
GlobalData tracks drug-specific phase transition and likelihood of approval scores, in addition to indication benchmarks based off 18 years of historical drug development data. Attributes of the drug, company and its clinical trials play a fundamental role in drug-specific PTSR and likelihood of approval.
Sonidegib phosphate overview
Sonidegib phosphate (Odomzo) is an anticancer agent. It is formulated as a hard gelatin capsules for oral route of administration. Odomzo is indicated for the treatment of adult patients with locally advanced basal cell carcinoma (BCC) that has recurred following surgery or radiation therapy, or those who are not candidates for surgery or radiation therapy. It is under development for the treatment of adenocarcinoma of the gastroesophageal junction and newly diagnosed medullablastoma. It was under development for the treatment of acute lymphocytic leukemia, acute myelocytic leukemia, child-pugh A cirrhosis, pancreatic adenocarcinoma, platinum-resistant or refractory or recurrent epithelial ovarian, fallopian tube or primary peritoneal carcinoma, myelofibrosis, post essential thrombocythemia myelofibrosis, post polycythemia vera myelofibrosis, adenocarcinoma of esophagus or gastroesophageal junction, extensive stage small-cell lung cancer, advanced or metastatic hepatocellular carcinoma, relapsed or refractory multiple myeloma, Gorlin syndrome, sporadic superficial nodular skin basal cell carcinomas, medulloblastoma, solid tumor, hematologic malignancies and chronic myelocytic leukemia, hedgehog pathway-mutated myelodysplastic syndrome, recurrent glioblastoma multiforme, estrogen receptor negative and HER2 negative breast cancer, metastatic colorectal cancer, castration-resistant prostate cancer, steroid-refractory chronic graft versus host disease (GVHD) after allogeneic HSCT.
Sun Pharma Advanced Research overview
Sun Pharma Advanced Research (SPARC), a subsidiary of Shanghvi Finance Pvt Ltd, provides biopharmaceutical clinical research and development services. The company develops active pharmaceutical ingredients, formulations and drug delivery technologies for the treatment of cancer and inflammatory diseases. Its research category consists of therapeutic focus, delivery technologies, research programs and research and development pipeline. SPARC’s therapeutic focus comprises oncology, neurodegeneration, ophthalmology, dermatology and abuse-deterrent formulations. SPARC is headquartered in Mumbai, Maharashtra, India.
For a complete picture of Sonidegib phosphate’s drug-specific PTSR and LoA scores, buy the report here.
This content was updated on 16 July 2024
Blending expert knowledge with cutting-edge technology, GlobalData’s unrivalled proprietary data will enable you to decode what’s happening in your market. You can make better informed decisions and gain a future-proof advantage over your competitors.
Be better informed
GlobalData , the leading provider of industry intelligence, provided the underlying data, research, and analysis used to produce this article.
GlobalData’s Likelihood of Approval analytics tool dynamically assesses and predicts how likely a drug will move to the next stage in clinical development (PTSR), as well as how likely the drug will be approved (LoA). This is based on a combination of machine learning and a proprietary algorithm to process data points from various databases found on GlobalData’s Pharmaceutical Intelligence Center .
More Relevant
Br-6002 by boryung pharmaceutical for duodenal ulcer: likelihood of approval, br-6002 by boryung pharmaceutical for gastric ulcers: likelihood of approval, br-6002 by boryung pharmaceutical for cardiovascular disease: likelihood of approval, yr-001 by yirui pharmaceutical technology for atopic dermatitis (atopic eczema): likelihood of approval, sign up for our daily news round-up.
Give your business an edge with our leading industry insights.
Sign up to the newsletter: In Brief
Your corporate email address, i would also like to subscribe to:.
Pharma Technology Focus : Focus (monthly)
Thematic Take (monthly)
I consent to Verdict Media Limited collecting my details provided via this form in accordance with Privacy Policy
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
Lung Cancer
There are different types of lung cancer. Knowing which type you have is important because it affects your treatment options and your outlook (prognosis). If you aren’t sure which type of lung cancer you have, ask your doctor so you can get the right information.
About Lung Cancer
Lung cancer causes, risk factors, and prevention, lung cancer early detection, diagnosis, and staging, treating non-small cell lung cancer, treating small cell lung cancer, after lung cancer treatment, easy reading, if you have non-small cell lung cancer.
If you’ve been diagnosed with non-small cell lung cancer, read this short and simple guide on non-small cell lung cancer to learn more.
If You Have Small Cell Lung Cancer
Read this short and simple guide about small cell lung cancer that covers diagnosis, treatment, questions to ask your doctor, and follow-up visits after treatment is complete.
Downloadable PDFs
- About and Key Statistics [PDF]
- Causes, Risks, Prevention [PDF]
- Detection, Diagnosis, Staging [PDF]
- Non-small Cell Lung Cancer Treatment [PDF]
- Small Cell Lung Cancer Treatment [PDF]
- Next Steps After Treatment [PDF]
Lung Pathology
Understanding your lung pathology report.
Find information that can help you understand the medical terms you might find in your lung pathology report after a lung biopsy.
This information is possible thanks to people like you.
We depend on donations to keep our cancer information available for the people who need it most.
Tools & Resources
Quiz: how much do you know about lung cancer.
Don’t be fooled by rumors and misinformation. Test your knowledge of 6 common beliefs about lung cancer.
Lung Cancer Videos
These videos will help you understand the different options around lung cancer screening and treatment.
Stay Away from Tobacco
Quitting smoking isn't easy, but we can help. Get tips, tricks, and information to help you kick the tobacco habit and live a healthier lifestyle.
Personal Health Manager
Organize your cancer journey with the American Cancer Society Personal Health Manager.
Caregiver Resource Guide
A helpful tool for people who are caring for someone with cancer. View the complete guide here.
News & Stories
Lung cancer news, stories of hope, lung cancer research highlights, help us end cancer as we know it, for everyone..

If this was helpful, donate to help fund patient support services, research, and cancer content updates.

IMAGES
VIDEO
COMMENTS
Advances in Lung Cancer Research - NCI
The Lung Cancer Master Protocol, or Lung-MAP, is a precision medicine research study for people with advanced non-small cell lung cancer that has continued to grow after treatment. Patients are assigned to different study drug combinations based on the results of genomic profiling of their tumors.
Lung cancer - The Lancet ... Lung cancer
Lung cancer arises in tissues of the lung, usually in the cells lining air passages. The two main types are small-cell lung cancer and non-small-cell lung cancer, according to the shape of cells ...
Current and Future Development in Lung Cancer Diagnosis
The global burden of lung cancer: current status and future ...
Lung cancer, a multifaceted disease, demands tailored therapeutic approaches due to its diverse subtypes and stages. This comprehensive review explores the intricate landscape of lung cancer research, delving into recent breakthroughs and their implications for diagnosis, therapy, and prevention. Genomic profiling and biomarker identification have ushered in the era of personalised medicine ...
Lung cancer is the commonest cancer globally. Reflecting patterns of smoking and other risk factor exposures, both the incidence of and mortality from lung cancer are highest in economically ...
Abstract. Despite a global pandemic that continued to inflict chaos and confusion on the world, resulting in fewer cancer screenings and delayed surgeries, remarkable lung cancer treatment advancements were made in 2021. From immunotherapy in the adjuvant setting to the approval of the first-in-class, highly selective inhibitor of KRAS G12C ...
Most People with Lung Cancer Smoked
The more can do at the beginning of treatment to essentially cure the cancer is where our research lies and where these exciting new changes come into play." Screening for Early Stage Lung Cancer. The identification of early stage lung cancer has increased significantly in the past five years because of low-dose CT screening for smokers.
Lung Cancer Research
Yet despite decades of research, scientists kept hitting roadblocks. That's because the protein's smooth, round shape lacked notches or grooves where drugs could attach. The mutant protein eventually was given a label by scientists: undruggable. In the early 2000s, molecular testing for lung cancer started becoming commonplace.
Help us end cancer as we know it, for everyone. Donate with Confidence. Cancer information, answers, and hope. Available every minute of every day. Get an overview of the types of lung cancer, recent key statistics, and learn more about lung cancer research.
Lung cancer - World Health Organization (WHO) ... Lung cancer
Lung Cancer - StatPearls
Prevention offers the greatest opportunity to fight lung cancer. Decades have passed since the link between smoking and lung cancers became clear, but smoking is still responsible for most lung cancer deaths. Research is continuing on: Ways to help people quit smoking and stay tobacco-free through counseling, nicotine replacement, and other ...
After 8 years of follow-up, there was a 59% lower cumulative rate of death from lung cancer. Of the male scans, 2.1% were positive, picking up 203 lung cancers, and 1.2% of screens delivered a ...
Lung Cancer Research. As one of the world's largest cancer research centers, MD Anderson is leading the investigation into new methods of lung cancer diagnosis and treatment. Each patient benefits from the most advanced research, delivered as rapidly as possible. Our current lung cancer research efforts include:
Citation: Immunotherapy before and after lung cancer surgery reduces death risk and disease recurrence, research finds (2024, September 8) retrieved 8 September 2024 from https://medicalxpress.com ...
According to the National Cancer Institute, approximately 234,580 people will be diagnosed with lung and bronchus cancer in the United States in 2024, and about 125,070 people will die of the disease - 65,790 men and 59,280 women. The five-year survival rate for these cancers is 26.7 percent.
Lung cancer - Symptoms and causes
Lung cancer starts in the windpipe (trachea), the main airway (bronchus) or the lung tissue. Cancer that starts in the lung is called primary lung cancer. Find out more. ... Cancer Research UK is a registered charity in England and Wales (1089464), Scotland (SC041666), the Isle of Man (1103) and Jersey (247). A company limited by guarantee.
Sonidegib phosphate is under clinical development by Sun Pharma Advanced Research and currently in Phase I for Non-Small Cell Lung Cancer. According to GlobalData, Phase I drugs for Non-Small Cell Lung Cancer have an 80% phase transition success rate (PTSR) indication benchmark for progressing into Phase II.
All Research Areas Cancer Prevalence and Cost of Care Health Disparities Native American Initiatives Natural Language Processing (NLP) Statistical Genetics Survey Methodology, ... to drop; (2) female lung cancer mortality has ... case-control association studies on a genome-wide basis." ... Contact: Eric J. (Rocky) Feuer, Ph.D., Chief ...
Lung Cancer Guide | What You Need to Know