

Junior Vet Academy:"Paws and Thought: How Critical Thinking Helps Vets Keep Pets Healthy!"
Title: "Paws and Thought: How Critical Thinking Helps Vets Keep Pets Healthy!"

In the world of veterinary medicine, critical thinking is like a superpower that helps veterinarians solve puzzles to keep our furry friends healthy and happy. Just like detectives, vets use their keen observation skills, logic, and knowledge to diagnose and treat animals. So, let's embark on an exciting journey to explore how critical thinking is the secret tool behind the scenes of veterinary care!
Understanding Critical Thinking in Veterinary Medicine:
1. Observation Skills: Just like Sherlock Holmes, veterinarians are expert observers. They pay attention to every detail - from a dog's wagging tail to a cat's meow - to detect signs of illness or injury.
2. Problem-Solving: Vets face mysteries every day. They gather clues by examining pets, asking questions, and using their knowledge to solve the puzzle of what might be wrong.
3. Analytical Thinking: Imagine vets as puzzle masters! They analyze symptoms, test results, and medical history to piece together the best treatment plan for each pet.
4. Decision Making: Making decisions is a crucial part of a vet's job. Using their critical thinking skills, they weigh options to choose the most effective and safest treatment for the animal.
Real-life Veterinary Adventures:
At Junior Vet Academy and Kids Vet Club you are the Vet. Together we walk through animal issues step by step. First recording observations, test results and owner input. Next we put on our thinking caps and anaylze the data. Then comes the hypothesis or as we vets say the "differential diagnosis" list. After additional exams and testing to prove our hypothesis we finish with a treatment plan to help our patient and its family.
2. Tales from the Examination Room: What is the physical exam and why is it so important? The physical exam is oftern the MOST important tool a veterinarain uses to help animals. Our patients ( excepts a few really smart birds) don't talk. How can we figure out the problem? The physical exam is oftern the answer. During this hands on exam we look the parient over from nose to tail or beak to tailfeather. It is with this valuable information we can find the source of the issue and createa plan to speed recovery.
Come join us on the farm and start building your veterinary diagnostic super powers.
Conclusion:
Critical thinking is the superhero tool in veterinary medicine. By nurturing these skills, kids can become keen observers and problem-solvers, ready to care for their pets or even consider a career in veterinary medicine. So, let's celebrate the power of critical thinking and the wonderful world of keeping our furry companions healthy and happy!
Remember, being a veterinarian isn't just about loving animals; it's also about using critical thinking to make a difference in their lives.
Amanda Mckee DVM
Recent Posts
"Keeping Your Furry Friends Safe: Holiday Pet Dangers"
Its a go for Santa's flight!
Kids Vet Club- Tips for Autumn from the Junior Vet Academy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Facilitating Development of Problem-Solving Skills in Veterinary Learners with Clinical Examples
Amanda (mandi) nichole carr.
1 Davies Livestock Research Centre, School of Animal and Veterinary Sciences, The University of Adelaide, Roseworthy, SA 5371, Australia
2 School of Animal and Veterinary Sciences, The University of Adelaide, Roseworthy, SA 5371, Australia
3 Australian Centre for Antimicrobial Resistance Ecology, School of Animal and Veterinary Sciences, The University of Adelaide, Roseworthy, SA 5371, Australia
Roy Neville Kirkwood
Kiro risto petrovski, associated data.
Not applicable.
Simple Summary
This review seeks to open discussion on the teaching of problem-solving skills in veterinary learners. Before a veterinary learn-er can solve a problem, they need to be able to recognize the problem. Then, information is gathered and economically viable solutions determined. To make problem-solving easier, we suggest a process with 5 elements: (1) define the problem list; (2) create an associated timeline; (3) describe the (anatomical) system involved or the pathophysiological principle applicable to the case; (4) propose management for the case; and (5) identify unique features of the case. In order to put the above into context, we end the review with an example case scenario showing the approach of teaching of problem-solving.
This paper seeks to open discussion on the teaching of problem-solving skills in veterinary learners. We start by defining the term problem before discussing what constitutes problem-solving. For veterinary medical learners, problem-solving techniques are similar to those of decision-making and are integral to clinical reasoning. Problem-solving requires the veterinary learner to organize information logically to allow application of prior or new knowledge in arriving at a solution. The decision-making must encompass choices that provide the most beneficial and economical approach. In a modification of an existing protocol, we suggest the inclusion of the 5 elements: (1) define the problem list; (2) create an associated timeline; (3) describe the (anatomical) system involved or the pathophysiological principle applicable to the case; (4) propose management for the case; and (5) identify unique features of the case. During problem-solving activities, the instructor should take the role of facilitator rather than teacher. Skills utilized in the facilitation of problem-solving by learners include coaching, differential reinforcement, effective feedback, modelling and ‘think out loud’. Effective feedback must inform learners of their progress and performance, as this is fundamental to continued learning and motivation to succeed. In order to put the above into context, we end with an example case scenario showing how we would approach the teaching of problem-solving to veterinary learners.
1. Introduction
One of the relatively common deficiencies in veterinary medical education is the lack of assisting of veterinary learners in the development of their clinical reasoning skills. However, if successful in the development of these skills it will make them more competitive in the employment market, an important outcome for modern education [ 1 , 2 ]. Indeed, developing clinical reasoning skills in learners is a requisite of any accreditation body for schools that are required to undergo accreditation [ 3 ]. For example, the Royal College of Veterinary Surgeons accreditation is based on Day One Competencies, and clinical reasoning and problem-solving competencies are clearly stated in the document (Competencies 22–25) [ 3 ]. From an educational perspective, clinical reasoning may be seen as skills in both complex problem resolution and a critical thinking. Utilizing case-based scenarios will provide suitable opportunities to assist veterinary learners in the development and implementation of their clinical reasoning. Solving of case-based scenarios should assist them in developing new skills of which, at a minimum, should stimulate self-directed (‘deep’) learning [ 4 , 5 ]. The case-based scenarios should be carefully chosen with the aim to encourage learners to incorporate knowledge from a variety of backgrounds, including basic, preclinical and clinical sciences [ 4 ].
Clinical reasoning during a clinical encounter consists of a few general steps: (1) collecting information; (2) analysis of the information; (3) management of the case; and (4) opportunistic promotion of animal health and welfare [ 6 , 7 , 8 , 9 , 10 , 11 ]. During each of these steps, the collected information may present elements that need to be solved (problem). For a positive outcome for the case, clinical reasoning should satisfactorily address each problem encountered.
While the human medical field provides pertinent literature concerning the development of problem-solving skills in medical learners [ 4 , 12 , 13 , 14 ], there is a dearth of such literature concerning veterinary learners with exceptions in some areas where emerging literature is available such in communication that includes some basic problem-solving skills. The present paper seeks to start to address this lack of literature related to teaching problem-solving skills related specifically to the veterinary medical field. In our current OneHealth world encompassing environmental, plant, animal and human health, and believing that teaching approaches are a transferrable skill, we will re-examine some human literature through a veterinary lens, and reinforce it with a veterinary clinical example. However, before addressing this issue, we must first define the meaning of the term problem and, more importantly, the nature of problem-solving.
2. Problem and Problem-Solving
2.1. what is a problem.
The term problem is difficult to clearly define and a plethora of explanations of the meaning of this term exist. Most common dictionary-based explanations related to problems in veterinary medicine would include something along the lines of a matter or situation regarded as unwelcome or harmful and needing to be dealt with and overcome. Problems may be ill-defined or well-defined. Problems with discrete presentation and clearly identifiable solutions are referred to as well-defined while problems with unclear presentation and/or many potential solutions are referred to as ill-defined [ 13 ].
2.2. What Is Problem-Solving
Problem solving should encourage the use of higher-order thinking skills to effectively manage and critically determine realistic solutions to problems. It is a basic skill or tool that is needed by employees for addressing workplace demands [ 1 , 15 ]. Problem-solving requires a complex set of attitudinal, behavioral and cognitive components, often used in a multiple-step process to arrive to the solution (i.e., collection, interpretation and integration of information) [ 14 , 16 ]. During the process of problem solving, a learner needs to combine old rules (cognition) and form new rules (cognition and metacognition; Figure 1 ). Each step in problem-solving can be seen as a decision tree [ 17 ] and may be approached using alternate pathways [ 18 ]. The pathway taken by the learner is usually one they have learned previously or a slight modification of it [ 18 ], and their personal preferences acquired during their studies and life experiences. Considering that problem-solving is only partly dependent on the context, problem solving skills can be utilized in future different and similar encounters [ 18 ]. For veterinary medical learners, problem-solving techniques are, in essence, similar to those of decision-making and are a key competence of learners/practitioners that is essential in clinical reasoning.

Problem-solving circle related to a veterinary medical problem.
Problem-solving should encourage learners to organize information in a logical manner [ 4 ] to allow them to apply a variety of prior learning (cognition) and new knowledge (metacognition) in the process of reaching a solution [ 4 , 13 , 15 ]. This should be accompanied by self-directed learning, including active listening, critical thinking and reflective practice [ 4 , 13 ].
2.3. What Is Decision-Making?
Decision-making requires a veterinary learner/practitioner to decide which course of action/issue/solution to pursue (extrapolated from [ 6 , 19 ]). The number of choices may be small or large. The decision-making process should select (compare and contrast) which choice would be most beneficial, economical and satisfactory for that particular situation for all involved parties, the client, the patient and the veterinary clinician ( Figure 2 ).

Decision-making process applicable to veterinary medical problem.
3. Teaching Problem-Solving
3.1. problem-solving techniques.
A plethora of problem-solving techniques have been described in a variety of scientific areas [ 4 , 16 , 20 ], including mathematics [ 21 , 22 ] and medical education [ 23 ]. In short, any teaching of problem solving is better than doing nothing, with the expectation that the learner will appreciate an ongoing need for further training [ 16 , 24 , 25 ]. This may be delivered as a specifically designed professional course or be adopted as a teaching principle within many disciplines. Problem-solving is discipline specific [ 20 , 22 ]. For medical education, it seems that a partially heuristic approach to problem-solving is acceptable [ 26 ]. Exposure to explicit instructions in problem solving has been reported to improve these skills in learners [ 4 , 15 , 16 , 18 , 23 , 27 ]. Explicit instruction should provide the learner with a ‘protocol’ (usually a decision tree) that can be applied to the problem solving [ 4 , 15 , 17 ]. Two frequently cited frameworks for teaching clinical reasoning are Clinical Reasoning Cycle [ 27 , 28 ] and Clinical Judgment Model [ 27 , 29 ]. However, for the problem-solving exercise, simplified problem-solving protocols may be more applicable.
Each step in the explicit instructions for problem-solving should lead to a maximum of 3–6 branches of a particular decision tree. If there is a likelihood that a particular step would result in more than 6 branches, it is advised that the particular step is further branched into smaller branches (steps) of the explicit instructions [ 17 ]. Then, this protocol can be applied to other scenarios [ 25 ]. The ‘protocol’ is often broadly discipline-dependent (e.g., computer software programming versus medical education) [ 19 ]. For the successful solving of the problem, the learner must approach the solving relying on some prior knowledge [ 18 , 21 ]. This is very important to note for learners in any of the medical education areas, including veterinary medicine since, without prior knowledge, problem-solving will be difficult or even impossible [ 30 ]. Hence, problem-solving activities must be tailored to the level of development of the learner (e.g., when learners are classified using the (O)RIME framework, different cases/clinical encounters are required for learners in R(eporter) compared to M(anager) levels) [ 31 ].
Meyer et al. [ 3 ] have proposed a problem-solving protocol applicable to case-based scenarios for medical disciplines that is composed of 4 elements: (1) define unfamiliar terms; (2) create a timeline associated with the problem; (3) describe the (anatomical) system involved; and (4) identify any unique features associated with the case. This protocol may be suitable for stimulation of deep learning in various disciplines and may be applicable to problem-solving in case-based scenarios related to clinical encounters. However, for applicability to clinical encounters, we propose changing the first element to ‘define the problem list’. As not all case-based scenarios can be solved by anatomical location (e.g., a problem related to a particular pathophysiologic principle or sign or syndrome, such as cough, diarrhea or mastitis), we propose the third element can be either what Meyer et al. [ 3 ] proposed, or be extended to ‘describe the (anatomical) system involved or the pathophysiological principle applicable to the case’. Finally, for applicability to case-based scenarios related to clinical encounters, the protocol needs a fifth element, which we propose to be ‘management for the case’. This element may address further data gathering and/or treatment and/or prevention of future cases of similar character.
Hence, our modified protocol applicable to clinical encounter-based case scenarios would include the following 5 elements: (1) define the problem list; (2) create a timeline associated with the problem; (3) describe the (anatomical) system involved or the pathophysiological principle applicable to the case; (4) propose management for the case; and (5) identify any unique features associated with the case.
3.2. Specific and Non-Specific Problems
Some problems detected during a clinical encounter are specific (distinguishing), others are not [ 32 , 33 ]. Specific problems, such as loss of menace response, mucus in feces or a swollen joint, assist the learner in making the decision (e.g., diagnosis). Non-specific problems such as pyrexia or loss of appetite, are less informative, or even non-informative, in the decision-making process. Making learners aware of the difference between specific and non-specific problems is very important [ 33 ] as this will allow them to minimize the amount of information handled at any given time.
3.3. Role of the Instructor in Teaching Problem-Solving
A problem in veterinary medical education is the frequent lack of educational training of the veterinary instructors [ 2 , 34 , 35 , 36 ]. Indeed, one of the medical areas mentioned as hugely deficient in 1970s was the instructor’s lack of educational training in problem-solving [ 37 ], and it remains true today.
The instructor should take more of the role of facilitator rather than teacher. Skills than can be utilized in the facilitation of problem-solving by learners include, but not limited to, coaching, differential reinforcement, effective feedback, modeling and ‘think out loud’ [ 17 , 26 ]. Effective feedback is essential to deep learning in medical, including veterinary medical, education [ 23 , 26 , 38 ]. Learners must be informed of their progress and performance as this is fundamental to continued learning and the motivation to succeed [ 38 ]. Learners should be stimulated to self-assess (i.e., reflect) on problem-solving activities as that is also essential to deep-learning [ 27 ].
3.4. Learner Benefits from Learning Problem-Solving Skills
The benefit of learning problem-solving skills is that they can then by applied to other similar or dissimilar problems encountered in clinical practice and, potentially, also in everyday life [ 2 , 4 , 7 ]. Once learned and repeatedly applied, problem-solving should become habitual and easily expanded [ 17 ]. The decrease in clinical errors after graduation is one of the outcomes that has been mentioned as an important benefit for learners [ 35 ]. The knowledge of the risk of introduction of false negative/positive test results should also benefit learners as it should decrease their reliance on laboratory data in the decision-making process [ 39 ].
4. Addressing Various Elements of Inadequate Problem-Solving
A learner may lack elements necessary for effective problem-solving during a clinical encounter ( Table 1 ; [ 11 , 12 , 26 , 27 , 33 , 35 , 40 , 41 , 42 , 43 ]). Similarly, this would also apply to case-related discussions, particularly when working in smaller groups. We do note that this table is not holistic and some areas are not addressed (e.g., a learner with inappropriate behavior and/or family/personal problems and/or lack of fitness to practice and/or lack of recognition of a learning opportunity and/or lack of self-esteem). We acknowledge the importance of these areas, however, they are beyond the scope of this writing. Although not a focus of the present paper, another important aspect that should be mentioned is the relative lack of general training of ‘soft skills’ in veterinary programs, including but not limited to communication, emotional intelligence, inter-personnel skills and professional behaviors. This is to the detriment of the teaching process when clinical disciplines are introduced. Therefore, learners do not know how to handle their emotions, stress, time pressure, being assessed and then even the best prepared didactic methodologies, as those presented in this paper fail to work. This writing concentrates on learners having problems with application of knowledge. For learners with problem-solving difficulties, they may show insufficient progress or may have difficulties with a particular problem-solving skill [ 43 ].
Addressing common elements of inadequate problem-solving by veterinary learners.
| Element Lacking/Parameter | Detection | Strategy to Assist the Learner | Example of Facilitating Discussion |
|---|---|---|---|
| Complex approach to a problem | Reflection ‘Think aloud’ | Purposeful questioning Team work | “Could we consider different ways to solve this problem?” |
| Inefficient data collection | Omission errors (e.g., Procedure/Process incomplete; Sticks to standardized protocol, disregarding clinical presentation) | Modelling of data collection followed by solicitation of new data presentation by the learner Providing more opportunities to practice (e.g., use of simulator/s) Purposeful observation of learners who are skilled in the particular omission | “Can we again go through the process of data collection in this case? I would like you to observe me doing the health interview and clinical exam. I would like you to think of what additional information or clarification would be helpful in this particular case that you may have omitted in your data collection.” |
| Presentation incomplete (e.g., Disregarding data judged as not important, Lack of identification of what is important) | Modelling of data collection followed by solicitation of new data presentation by the learner Providing more opportunities to practice | “Can we again go through the process of data collection in this case? I would like you to observe me doing the health interview and clinical exam. You should pay attention to the items used in obtaining information. Then we can re-discuss your findings.” | |
| Inefficient data reporting | Inability to create appropriate/prioritized list of differential diagnoses | Increased clinical exposure and requirement to present cases at rounds Modelling of data analysis and creating differential diagnosis list Purposeful questioning Providing more opportunities to practice Providing regular feedback ‘Think aloud’ | “Can you summarize what the main findings are in one to two sentences?” or “Can you write down the list of problems for this case?” . “Now, it will be good to hear a prioritized list of differentials considering rule-ins and rule-outs applicable to this case.” or “Please prioritize the list of problems detected in this case to assist us in creating an appropriate list of differentials.” |
| Reporting/Summarizing | “Let’s discuss further the data gathered. I think you summarized the case you presented as a calf with a fever, swelling of multiple joints, which are tender and, from the health interview you know that this calf had an episode of diarrhea some two weeks ago. In fact, that would be a very good summary. However, you also added a few elements which are very loosely connected to this case. For example, yearlings having diarrhea that seems to be related to parasitic burden. This led you to a conclusion that this calf may be suffering from parasitic gastroenteritis. Parasitic gastroenteritis may be the problem of yearlings which are on pasture. However, this 18-day old calf has been hand-reared. I would like you to think of two completely separate problems. Can we re-discuss your differential again?” “Please watch me discussing this with the client, particularly how I would put things together.” | ||
| Seek answer in ‘textbook’ presentations only | “Let’s discuss further the data you gathered. Now, it will be good to think of which diagnoses may fit some or a majority of these problems, although they may not be an exact match.” | ||
| Poor problem detection | Difficulty seeing the scope of a problem Lack of recognition of a particular clinical problem Lack of recognition of the effect of the problem on the client | Employ ‘Component opportunity’ Purposeful questioning | “Let’s discuss further the data gathered. You mentioned that in this cow you detected a fever, cough, purulent nasal discharge, abnormal lung sounds on the right cranio-ventral side and that she has calved some 7 days ago. You also mentioned that the client has given her oral calcium about 2 days after calving for suspected milk fever. You connected all detected clinical signs but skipped through the health interview information in your interpretation. I think, it is important to consider the health interview in your problem presentation. Can you think of the main pathophysiological mechanism of hypocalcemia and how that may be related to the current case?” |
| “Do you notice anything else that should be on the list of problems for this particular case?” | |||
| “Can we discuss the parameters you detected and list them separately into ‘normal’ and abnormal? We are all aware that these should be considered together with other findings but for the purpose of this exercise let’s consider them independently. Do you agree?” | |||
| Poor implementation of solutions | Lack of tailoring the solution to the particular circumstances/presentation | Purposeful questioning Modelling of ‘Think aloud’ | “Let’s discuss further the management you propose. You mentioned that this dairy enterprise has been under new management for a few months and there has been a rise in cases of left displaced abomasum. Can you think of management solutions for this enterprise that are a priority to prevent future cases from occurring rather than continue with surgical interventions ?” |
| Lack of suitable solutions (e.g., learner lacks understanding of what is the goal of the intervention) | “Can we go through the solution you are proposing? This farm has an individual cow with respiratory disease and you have recommended treatment with ceftiofur, a third-generation cephalosporin antimicrobial. I think it is important to consider responsible antimicrobial use in your treatment recommendation. Can you think of another antimicrobial that may be more suitable for an individual case and how that may be related to good antimicrobial stewardship?” | ||
| Proposed solution offensive | “I think we should discuss how you delivered your recommendations to the client? You mentioned that his management was poor and all his problems were due to this. It is important to consider how that made the client feel. We are aware that there are some management areas that need to be improved. However, the delivery of the message must be carefully crafted. It is important to praise the client for what they are currently doing well but also make suggestions on how to improve the current practices. Can you think of a way of doing this?” | ||
| Seeks ‘textbook’ solutions only | “Let’s discuss further the solutions you propose. It is good to think of tailoring solutions for this particular enterprise, even if they are not an exact match to each individual problem occurring on the farm.” | ||
| Poor evaluation of the outcome | Lack of holistic approach to the expected outcome |
We recognize that addressing problem-solving difficulties also requires some practice and experience by the instructor, inclusive of specific training. The starting point in addressing the difficulties in problem-solving, from an instructor’s view, is the recognition of the different types of difficulty in a learner. Based on this, appropriate intervention strategies can be implemented. Effective feedback should be used to assist the learner in developing better problem-solving clinical skills as part of developing appropriate clinical reasoning. We will use an example of guiding the clinical teaching of learners using the five microskills model [ 35 , 44 , 45 ]. Most of the elements lacking during the problem-solving can be addressed during the ‘Correct mistakes’ microskill. However, some elements may be addressed earlier, in the ‘Probe for supportive evidence’ and, less likely, the ‘Get a commitment microskill (provided instructors observe the learner during data collection).
Poor Problem Detection during Clinical Problem-Solving
A cornerstone of problem-solving is problem identification/recognition [ 24 ]. However, in veterinary medical education, anecdotal evidence exist that some learners do not recognize some problems (as observed by the authors). Indeed, the lack of problem detection is also reported in other disciplines [ 6 , 24 ]. Based on literature evidence [ 6 , 14 , 26 , 42 , 46 , 47 , 48 ], a lack of recognition of problems may partly be due to:
- Individual capacity and differences in mental problem-solving skills between people
- Differences in age and gender (variable reports; detected during exams but also in clinical practice) with females and more mature people showing usually better problem-solving skills
- Flows in data gathering, with people having problems in data gathering having poorer problem-solving skills
- Following strict guidelines with little to no adjustments to the particular circumstances/presentations, seeking ‘textbook’ answers and so failing to realize that complaints often do not express themselves clearly such as with poorly expressed signs and syndromes
- Lack of connection of involvement of multiple organ systems/pathophysiology
- Lack of capacity to deal with multiple activities and hypotheses at once (multitasking)
- Lack of lifelong learning/continuing education of veterinary instructors adversely impacting availability of current information and so effective teaching
- Learner inexperience in problem-solving in veterinary medical fields, but may be also generalized poor problem-solving
Therefore, prior to seeking solutions, problem-solving should start with helping the learner to identify/recognize the problem. One of the possible approaches to the lack of problem recognition is so-called ‘component opportunity’ [ 24 ] where the ‘bigger problem’ is split into smaller components, each with at least one ‘problem’ that needs solving. Due to the differences between people in the mental skills required to solve the ‘bigger problem’, splitting it into components is often more easily said than done as the instructor would need to be able to facilitate the learner to do this on their own.
5. Example Clinical Encounter
The following information is provided to the learners
- Case encounter occurs early morning
- Holstein-Friesian calf from an embryo transfer recipient cow
- Delivered 10 days ago without assistance
- Had high vigor until last night
- Sudden onset of diarrhea about 6- 8 h before being seen
- Now in sternal recumbency, semi-obtunded
- ○ Cardinal signs all at the lower end of ‘normal’
- ○ Mucous membranes tacky but relatively moist
- ○ Skin tent 8 s
- ○ Eyes sunken about 0.5 cm from the orbit
- ○ Lack of suck reflex
- ○ No alimentary sounds at the abdomen
5.1. What Should Problem-Solving Address?
Using our protocol, modified from Meyer et al. [ 3 ], the problem-solving should address the following
- What is missing on the learner’s problem list
- Can exclude relevant congenital problems
- Was OK up to last night
- Peracute to acute case
- Laboratory findings may be unreliable
- Loss of absorptive capacity
- Mechanical damage to the intestinal wall
- Overgrowth of unwanted bacteria and production of D-Lactate
- Dehydration
- Hypokalemia
- Neonatal calf diarrhea usually results in a metabolic acidosis, not a metabolic alkalosis
- May not be high on the list due to the lack of the toxic line on the gums
- Dehydration and hypovolemic shock
- Sepsis absent or compensated, plus toxemia
- Toxemia likely absent
- Excess D-Lactate
- Hypoglycemia
- Metabolic acidosis
- Lack of perfusion
- ±Toxemia
- Initially, intravenous due to lack of suck reflex and inability to absorb oral fluids
- Continue with oral
- Bolus in 1st hour
- On-going fluid therapy
- Re-introduction of milk
- All undifferentiated calf diarrhea should be considered infectious until proven otherwise
- Contagious or not
- Zoonotic or not
- Colostrum management
- Housing management
- Consider immune-compromised people
- Some of the acid-base (e.g., the excess of D-Lactate) and electrolyte imbalances (e.g., apparent hyperkalemia when the body suffers from absolute hypokalemia) may not be detected by laboratory tests
- Due to the very rapid development, some of the clinical findings may be unreliable (e.g., the real degree of dehydration may not be properly detected with estimation of enophthalmia and/or skin tent)
5.2. Assisting the Learner to Recognise Problems with Example Discussions
We provide a variety of examples of potential presentations of the learner’s problem-solving skills and, for each of the presentation, the potential advisory discussion to assist the learner in addressing the lack of problem-solving skills ( Table 2 ).
Using an example of undifferentiated calf diarrhea in assisting veterinary learners with problem recognition and the specific roles of each problem in the entire problem presentation during a case-based discussion or a clinical encounter.
| Item | Potential Causes/Importance | Example Assisting Discussion |
|---|---|---|
| Cardinal signs ‘normal’ | No sepsis, but may have toxemia | |
| Enophthalmos 0.5 cm | Used to estimate dehydration | “It would be useful to think of pathophysiologic mechanisms that may lead to enophthalmos.” |
| Lack of alimentary motility | Used to estimate D-lactate acidemia and hypokalemia | “Can you think of few factors that may result in decreased motility of the alimentary system (ileus) in this calf?” |
| Lack of suck reflex | Used to estimate D-lactate acidemia and hypokalemia | “Can you think of few factors that may result in loss of the suck reflex in this calf?” |
| Semi-obtunded | “If we know that lab results for some metabolites and electrolytes may not be reliable, we have to think about what may be the effects of some of these metabolites or electrolytes on the calf’s demeanor and on the parasympathetic system.” “Can you also think of what may be happening with the gut microbiota and what may be the effect of the changes if they occur?” | |
| Severe peracute diarrhea | Rapidly developing | “We have discussed the significance of the enophthalmos and the prolonged skin tent. Think of the speed of development of these signs and how they may be affected by the peracute development of diarrhea in this calf?” |
| Skin tent 8 sec | Used to estimate dehydration | “It would be good to think of the pathophysiologic mechanisms that may lead to prolonged skin tent.” |
| Sternal recumbency | “Can you think of a few factors that may result in sternal recumbency in this calf?” | |
| Hypokalemia | ||
| Metabolic acidosis | “We know that typically, diarrhea leads to alkalemia due to loss of electrolytes in feces. Indeed, this is true for mature cattle as well. However, this may not be the situation in neonates. Can you think of what electrolytes may be lost with the diarrhea in this calf? Then, please think of the outcome on the acid-base status and the expected electrolyte balance?” | |
| Unreliable laboratory findings | “It is important to realize that due to a few pathophysiological derangements, blood electrolytes and acid-base balance testing may not be reliable in neonatal calves. Can you think what electrolytes may not be represented correctly in the biochemistry panel in this calf and why?” “Can you think of what may be happening with the gut microbiota and what may be the effect of the changes, if they occur?” “Now, can you think of what form of lactate is normally produced in the body of mammals that is a subject of the laboratory analysis?” “Now, after we established these differences, could you think of reasons why D-Lactate concentrations not been reported with the biochemical tests?” “Some electrolytes in diarrhea shift from intracellular to extracellular. Can you give an example?” “Can you now think what would be the result of this shift of potassium on the serum biochemical test results?” | |
| 10-day old calf | Age-related etiology | “Can you think of the common causative agents associated with calf diarrhea?” “Now, can you think of the age at which these causative agents usually cause diarrhea in calves?” |
| Dairy | Not on dam | “Let’s think of the usual management of neonatal dairy calves. Can you think on the feature that differs from beef calves?” |
| Embryo-transfer product | Expensive | “Let’s think about the cost-benefit of treatment of this calf. Can you think what parameters should be accounted for before making the final decision?” |
| Prevention of further cases | Animal welfare Client frustration Economics Loss of genetics | “Can you tell me what you think should be done in future to prevent recurrence of this problem? What factors should be considered when making decisions on the prevention strategies? Can you explain why prevention is important for the client?” |
| Role of management | Colostrum management Environment Hygiene Stress | “Could you explain what management factors may contribute to the occurrence of diarrhea in this calf on this enterprise?” |
| Zoonotic potential | Public health | “We already mentioned the common pathogens associated with calf diarrhea. Can you think of what risks there are for people involved in management of this and other calves on the enterprise and discuss what specific factors need to be considered?” |
6. Conclusions
The teaching of effective problem solving is essential to ensure the clinical competence of veterinary learners. From the literature we have reviewed, we conclude that learners should be guided through 5 elements, namely define the problem list, create a time line for the problem, describe involved anatomical system/pathophysiology, propose case management, and identify unique case features. In common with all clinical teaching, while guiding learners through these elements the provision of appropriate feedback is required. If all this is done effectively, the developed problem-solving skills will be transferrable to other similar or dissimilar cases and even into everyday life.
7. Glossary
Case-based discussion —clinical teaching tool that consists of a structured approach to learners’ clinical reasoning around written case records and/or structured interview with a simulated client and patient.
Clinical encounter —any physical or virtual contact with a veterinary patient and client (e.g., owner, employee of an enterprise) with a primary responsibility to carry out clinical assessment or activity.
Clinical instructor —in addition to the regular veterinary practitioner’s duties, a clinical instructor should fulfil roles of assessor, facilitator, mentor, preceptor, role-model, supervisor, and teacher of veterinary learners in a clinical teaching environment. Apprentice/intern in the upper years, Resident, Veterinary educator/teacher, Veterinary practitioner.
Clinical reasoning —process during which a learner collects information, process it, comes to an understanding of the problem presented during a clinical encounter, and prepares a management plan, followed by evaluation of the outcome and self-reflection. Common synonyms include clinical acumen, clinical critical thinking, clinical decision-making, clinical judgment, clinical problem-solving, and clinical rationale.
Critical thinking —self-directed, self-disciplined, self-monitored, and self-corrective objective, unbiased analysis and evaluation of information form a variety of sources in order to form a judgement.
Deep learning —aiming for mastery of essential academic content; thinking critically and solving complex problems; working collaboratively and communicating effectively; having an academic mindset; and being empowered through self-directed learning.
Differential reinforcement —process in which a specific response is reinforced or not (i.e., positive or negative reinforcement) in a particular context with aim to address challenging of undesirable behavior.
Five microskills model —Instructor-centered model of clinical teaching: (1) Get a commitment; (2) Probe for supporting evidence; (3) Teach general rules; (4) Reinforce what was done well; and (5) Correct mistakes.
Heuristic —general methods used in problem-solving, applicable to problem in any content domain.
Higher order thinking skills —A series of competencies that can be utilized in analysis and evaluation of complex information, including categorization, manipulation, and connection of facts, conceptualization, troubleshooting for solutions and problem-solving. It is on a level that is higher than memorizing facts or recollection only.
Metacognition —This is a critical awareness of one’s thought processes and learning, and an understanding of the patterns of thinking and learning.
Self-directed learning —learners take charge of their own learning process by identifying learning needs, goals, and strategies and evaluating learning performances and outcomes. Learner-centered approach to learning.
Funding Statement
This research received no external funding.
Institutional Review Board Statement
Informed consent statement, data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Get access to all handy features included in the IVIS website
- Get unlimited access to books, proceedings and journals.
- Get access to a global catalogue of meetings, on-site and online courses, webinars and educational videos.
- Bookmark your favorite articles in My Library for future reading.
- Save future meetings and courses in My Calendar and My e-Learning .
- Ask authors questions and read what others have to say.
Clinical reasoning in veterinary practice
Clinical reasoning is the process by which veterinary surgeons integrate a multitude of clinical and contextual factors to make decisions about the diagnoses, treatment options and prognoses of their patients. The brain utilises two methods to achieve this: type one and type two reasoning. Type one relies on shortcuts such as pattern-recognition and heuristics to deduce answers without involving working memory. Type two uses working memory to deliberately compute logical analyses. Both reasoning methods have sources of errors, and research has shown that diagnostic accuracy is increased when they are used together when problem-solving. Despite this, it appears unlikely that clinical reasoning ‘skill’ can be improved; instead, the most effective way to improve reasoning performance experimentally appears to be by increasing and rearranging knowledge. As yet, there is no evidence that overall clinical reasoning error can be reduced in practice.
INTRODUCTION
Many times a day, practising veterinary surgeons in all domains have to make clinical decisions regarding the appropriate diagnosis, treatment and prognosis of their patients. Not only do these decisions rest on the clinical presentation of the animal before them, but also on a myriad of contextual factors including finances, available equipment, resources and client wishes (Everitt, 2011; and Durning et al . , 2012). The amalgamation and rationalisation of the clinical and contextual factors of a case into a decision is known as clinical reasoning. This article aims to explain the reasoning process used by veterinary surgeons and explore possible ways to improve our clinical decision-making skills.
How do veterinary surgeons perform clinical reasoning?
Clinical decisions are made in the same way that humans make hundreds of other, major and minor, decisions within their daily lives. To understand the mental processes that embody clinical reasoning, we must look towards cognitive psychology, the scientific study of cognitive abilities (Norman, 2005). Researchers in this field have determined that humans use two overarching reasoning methods, known as type one and type two reasoning. These two systems have their own unique advantages and disadvantages, hence our need for both.
The fundamental difference between the two types of reasoning is their utilisation of working memory (Stanovich & Toplak, 2012; and Evans & Stanovich, 2013). Working memory functions like a ‘whiteboard’ for our brain, it temporarily holds information to make it available for processing, and then either discards that information or stores it in long-term memory (Baddeley, 2003; and Van Merrienboer & Sweller, 2010). It is responsible for our reasoning activities and thus behaviours, but has a very limited capacity. You have probably experienced this when trying to remember an address, or a phone number; after a certain load is reached, you lose the ability to store or process information. Distractions play a key role in the effectivity of working memory, they take up space, and thus reduce the ability to reason. This includes both cognitive tasks and environmental distractions, both of which are common occurrences within a veterinary consultation (Mamede et al., 2017; and Norman et al., 2016).
Working memory involvement provides the distinction between the two reasoning methods (Stanovich, Toplak 2012). Let us first consider type two reasoning, which uses our working memory to process information and reach a decision. This system is usually slow, analytical and consciously directed by the clinician (Eva 2005). It is an important process as it allows us to think abstractly, and separate relevant and non-relevant elements of a problem. There are several specific reasoning modes we can use within this system, including hypothetico-deductive reasoning, where a hypothesis is tested (‘If there is an infection then I should find elevated leucocytes’) – and inductive reasoning, where data is used to reach a conclusion (‘There are elevated leucocytes therefore there could be an infection’) (Croskerry, 2009; and Evans & Stanovich, 2013). In addition to these modes, we can apply frameworks to assist with problem solving – for example, the use of decision analysis, whereby quantitative calculations are used to determine the treatment option most likely to succeed (Cockcroft 2007). This is also where evidence-based medicine can assist with decision-making, as the findings are incorporated into analytical processes.
In comparison, type one reasoning is defined by non-reliance on working memory (Stanovich, Toplak 2012). This means that type one strategies must occur without deliberate thought – usually making them quick and effortless (Croskerry, 2009). This allows us to make judgements in our daily life that we cannot afford to spend time computing – for example, reasoning that the animal coming towards you is very large, with big ears and a trunk and therefore must be an elephant. Rather than having to consciously calculate this, we can instantly recognise the pattern that is the ‘approaching elephant’ and act accordingly. If humans were unable to utilise type one reasoning for this purpose, we would struggle to achieve anything, as we would spend the majority of our time trying to decipher the world around us (Thammasitboon & Cutrer, 2013).
There are, again, several modes that can be implemented within the group of type one reasoning techniques (all selected and used unconsciously). These range from innate heuristics used by our brains to ‘save space’, to learned associations through repeated exposure until the point of automaticity (Croskerry, 2009). Pattern recognition (as per the elephant example above) is commonly used by clinicians (Eva, 2005; and May, 2013). This entails recognising patterns based on either a prototype (a previous case that matches) or an exemplar (amalgamation of experience of several cases that form a set of ‘general rules’)(Evans and Stanovich, 2013). The brain reacts to a trigger (often a case presentation) that stimulates retrieval of a relevant exemplar/prototype – for example, an 8-year-old entire bitch presenting with increased thirst and severe lethargy 6 weeks post-oestrus might trigger ‘pyometra’ exemplar retrieval without conscious thought by the clinician. Context has been shown to be very important in pattern recognition, with studies finding that non-contributing aspects of a condition can be stored within an exemplar (Hatala et al., 1999). For veterinary surgeons this might include characteristics such as coat colour or approachability, factors which often are not related to the clinical condition.
Another commonly used mode of type one reasoning is the unconscious application of heuristics. These are ‘shortcuts’ that our brains use to save energy and process problems more quickly (Croskerry, 2009a; Stanovich & Toplak, 2012). For example, when searching for a possible diagnosis, previous salient diagnoses (perhaps recent, or with a strong emotional impact) will be assumed to be more common and thus more likely – this is the availability heuristic (Norman et al. 2017). Stereotypes are another example of a heuristic that can impact clinical reasoning; have your assumptions of the likelihood that an owner will pay for a particular treatment, or the assumption that certain breeds of dog will be likely to be suffering from certain conditions, ever impacted on your decision-making? It may seem that the use of these heuristics would be detrimental to the reasoning process, however that is not necessarily the case, as they have developed from an evolutionary need to reason quickly and, for the most part, accurately (Croskerry, 2009a).
The key properties of the two types of reasoning are summarised in Table 1.
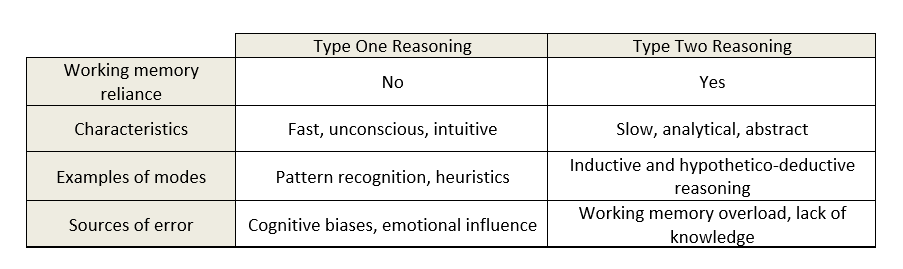
Table 1 . Types of reasoning: A comparison of features of type one and type two reasoning (Croskerry, 2009b; and Stanovich & Toplak, 2012)
Sources of error in reasoning
Both type one and type two reasoning have weaknesses that need to be managed in order to ensure successful use (Norman et al. 2017). We have already discussed the main limitations of type two reasoning, which are inherent in the nature of the process: time and working memory consumption (Eva 2005). Type one reasoning can be flawed by the shortcuts it relies on, which become known as cognitive biases when they fail (Klein 2005). The most significant of these within medical fields is premature closure (Graber, 2005), which occurs when other possible differentials are not considered once the first diagnosis is reached. Another example is the tendency for clinicians to search out information that confirms their working diagnosis, and disregard information that opposes it; this is known as confirmation bias (Eva & Norman, 2005). Type one processes are also highly context-bound and as such can be influenced by emotions, which under certain circumstances could cause reasoning error (Croskerry, Norman 2008; Slovic et al. 2004).
Interestingly, research examining the impact of educating clinicians to detect their own cognitive biases has shown no effect on diagnostic accuracy (Shimizu et al., 2013; and Sherbino et al., 2014). There is also no strong evidence to suggest that attempting to activate type two processes and slow the decision-making process down will improve diagnostic accuracy (Norman et al. 2017). In the past, type one reasoning was thought to be inaccurate and thus was discouraged, particularly in students. However, a multitude of research has now shown that type one is, at the very least, as accurate as type two reasoning; if not more so (Coderre et al., 2003; and Eva, 2005). The most effective strategy, however, has been shown to be a combination of the two – dual-process reasoning (Ark et al., 2006).
Dual-process reasoning
Dual-process reasoning, illustrated in Figure 1, is the use of both type one and type two reasoning to solve a problem. In reality, all reasoning that occurs in non-laboratory conditions is dual-process, as we cannot stop intuitive type one processes taking over when they are able to, nor use them when there are no pattern or heuristics triggered (Evans & Stanovich, 2013).
Dual-process reasoning starts when a stimulus (here, the clinical history and presentation of an animal) triggers type one methods to begin. There has been debate in the literature about whether it is possible to also trigger type two reasoning at the outset, but this seems unlikely due to the fast and unconscious nature of type one processes; they will, essentially, get there first (Croskerry, 2009a; and Evans & Stanovich, 2013). It is possible, however, that pattern recognition will not be able to offer a solution to the problem, in which case type two methods take over automatically. This would be the point at which the clinician would first be consciously aware of their thought processes, as they try and solve the problem analytically. As they do this, pattern recognition and heuristics will be still be used wherever possible, remembering that these are not controlled by the clinician. In fact, the most the clinician can do is be aware that heuristics have been used and ‘double-check’ the conclusions they suggest. This leads to a fluid system where clinicians change between the two systems of reasoning frequently, eventually reaching a conclusion. There may be any combination of periods of logical problem solving and periods of automaticity (Croskerry et al. 2014).
Dual-process reasoning allows for the weaknesses of both types of decision-making to be minimised; type one will prevent cognitive overload and save time, whilst type two will resist bias and lack of experience. However, it is important to be aware that the weaknesses of both methods can still impact decision-making, particularly in the face of lack of knowledge (Evans & Stanovich, 2013).

Figure 1 . Dual-process reasoning. The dual-process model of clinical reasoning in a diagnostic situation, adapted from Croskerry (2009a).
Improving clinical reasoning
Diagnostic error has been found to occur in 10–15% of medical cases (Graber et al., 2005; and Graber, 2013). It is likely that diagnostic error is a significant problem within veterinary medicine also (Oxtoby et al. 2015), but data is not available to estimate prevalence. This concerning figure has promoted much investigation into the improvement of clinical reasoning skills in both students and experienced clinicians. However, as previously noted, mechanisms to reduce error that initially seemed promising, removing cognitive biases and adopting analytical processes, have been shown not to impact diagnostic accuracy (Norman et al. 2017).
So how can clinical reasoning be improved? The answer is not particularly surprising; studies have indicated that the presence and arrangement of knowledge appears to have the biggest impact on improving medical reasoning performance (Norman, 1989; Dory et al., 2010; and Norman et al., 2017). This is supported by a phenomenon known as ‘content specificity’, whereby reasoning accuracy depends on the case knowledge and not on the level of ‘reasoning skill’ of the practitioner; i.e. performing well on one case does not predict performance on a different case (Norman, 2005; Dory et al., 2010). The implication is that there appears to be no shortcut to effective reasoning that we can employ as clinicians, or teach to students. What is required is extensive accessible knowledge, not the ‘heard it in a lecture once’ kind of knowledge (Norman et al., 2017).
The knowledge used for clinical reasoning resides within illness scripts, mental models of specific illnesses which are stored in long-term memory (Charlin et al., 2007; and Schmidt & Rikers, 2007). Veterinary surgeons have many of them; ranging from common disorders such as flea allergy, to rare but important diseases such as bovine spongiform encephalopathy. Information including signs, epidemiology and treatment options are stored together in this way. When presented with a new patient problem, the brain will automatically search through the bank of scripts until one that matches the patient’s condition is found. If there is a direct match, type one reasoning can process the script without the need for working memory involvement. If there are discrepancies between reality and the script, type two reasoning will be required to fill in the gaps (Cutrer et al., 2013). Illness scripts exist at varying levels of completion – for instance, a student that has only learnt about a particular disease in a lecture will have script that is mostly incomplete. A veterinary surgeon that has been practising for many years and has encountered the disease countless times with a variety of clinical presentations and outcomes will have, in comparison, a much more robust script.
It is therefore logical that veterinary students should focus on obtaining in-depth knowledge of the common conditions that they will be required to treat regularly in practice, including experiencing a range of possible clinical presentations and treatment options (May 2013). Having the necessary background knowledge allows for analytical processes (type two reasoning) to be used, particularly alongside reasoning frameworks. Refining this knowledge through clinical experience leads to development of more complete illness scripts, which allow for the benefits of type one reasoning to also be used.
But what about experienced veterinary surgeons, with knowledge sufficient to have built complex scripts? Several studies have indicated that rearrangement of knowledge may be effective in improving diagnostic accuracy in experienced practitioners (Norman et al. 2017). Research has focused on the use of structured reflection for this purpose; revisiting a conclusion (no matter which initial reasoning type was used) and re-evaluating the evidence leading to it, considering possible alternatives (Mamede et al., 2008). It is thought that the reflective process impacts upon the storage and retrieval of knowledge, however, the mechanism for this is not yet known. Based on this finding, other methods of retrieving and reorganising knowledge may also have a role in improving clinical reasoning through increasing script functionality; for example, the framework for problem-based inductive clinical reasoning developed by Maddison et al. (2015), which provides a logical approach to decision-making in practice.
The eventual goal should be to form complete illness scripts that allow type one reasoning, thus saving time and working-memory for other clinical tasks, such as communication and calculations. However, effective type two reasoning is vital to reach this point.
Problem solved?
Reducing error in clinical reasoning has been considered important to improve patient safety within medicine and, more recently, veterinary medicine (Oxtoby et al., 2015). However, evidence is lacking which demonstrates that errors in the process of clinical reasoning can be significantly reduced (Eva & Norman, 2005; and Norman et al., 2017). Thus, we may need to circumvent the inaccuracy of human reasoning to improve patient outcomes.
Evidence-based medicine (EBM) and decision support systems (DSS) provide two possible options for achieving this. The former uses clinical research findings to suggest a course of action, the latter uses databases consisting of qualitative and quantitative information and decision-making algorithms (Cockcroft & Holmes, 2008). Their ability to influence the daily practice of veterinary surgeons is as yet unconfirmed and their use is dependent upon sufficient time and resources being available (Vandeweerd et al. 2012). However, further research into the potential for EBM and DSS to improve clinical outcomes in veterinary patients is warranted.
There are two methods of clinical reasoning used by humans: type one, which does not rely on working memory, and type two, which does. The former is usually fast and unconscious, whereas the latter is usually slow and deliberate. Both methods have been found to be most effective when used in combination, as dual-process reasoning. Whilst we might be tempted to assume that type one reasoning leads to the majority of errors, this is not the case. In fact, the evidence suggests that increasing knowledge is the only way to reliably improve reasoning performance. There may also be a role for knowledge reorganisation in improving reasoning, although this needs further exploration. There is, as yet, no evidence that improving clinical reasoning will lead to reduced diagnostic error in practice.
Conflict of Interest
The author declares no conflicts of interest.
- Ark, T.K., Brooks, L.R. & Eva, K.W. (2006). ‘Giving Learners the Best of Both Worlds: Do Clinical Teachers Need to Guard Against Teaching Pattern Recognition to Novices?’, Academic Medicine , 81(4): 405–409. DOI: http://dx.doi.org/10.1097/00001888-200604000-00017
- Baddeley, A. (2003). ‘Working memory: Looking back and looking forward’, Nature Reviews Neuroscience , 4(10): 829–839. DOI: http://dx.doi.org/10.1038/nrn1201
- Charlin, B., Boshuizen, H.P.A., Custers, E.J. & Feltovich, P.J. (2007). ‘Scripts and clinical reasoning’, Medical Education , 41(12): 1178–84. DOI: http://dx.doi.org/10.1111/j.1365-2923.2007.02924.x
- Cockcroft, P. (2007). ‘Clinical reasoning and decision analysis’, Veterinary Clinics of North America: Small Animal Practice , 37(3): 499–520. DOI: http://dx.doi.org/10.1016/j.cvsm.2007.01.011
- Cockcroft, P. & Holmes, M. (2008). Handbook of evidence-based veterinary medicine . Wiley-Blackwell.
- Coderre, S., Mandin, H., Harasym, P.H. & Fick, G.H. (2003). ‘Diagnostic reasoning strategies and diagnostic success’, Medical education , 37(8): 695–703. DOI: http://dx.doi.org/10.1046/j.1365-2923.2003.01577.x
- Croskerry, P. (2009a). ‘A universal model of diagnostic reasoning’, Academic Medicine , 84(8): 1022–8. DOI: http://dx.doi.org/10.1097/ACM.0b013e3181ace703
- Croskerry, P. (2009b). ‘Clinical cognition and diagnostic error: Applications of a dual process model of reasoning’, Advances in Health Sciences Education , 14(1 SUPPL): 27–35. DOI: http://dx.doi.org/10.1007/s10459-009-9182-2
- Croskerry, P. & Norman, G. (2008). ‘Overconfidence in clinical decision making’, The American Journal of Medicine , 121(5): S24-9. DOI: http://dx.doi.org/10.1016/j.amjmed.2008.02.001
- Croskerry, P., Petrie, D.A., Reilly, J.B. & Tait, G. (2014). ‘Deciding about fast and slow decisions’, Academic Medicine , 89(2): 197–200. DOI: http://dx.doi.org/10.1097/acm.0000000000000121
- Cutrer, W., Sullivan, W. & Fleming, A. (2013). ‘Educational strategies for improving clinical reasoning’, Current Problems in Pediatric and Adolescent Health Care , 43(9): 248–57. DOI: http://dx.doi.org/10.1016/j.cppeds.2013.07.005
- Dory, V., Gagnon, R. & Charlin, B. (2010). ‘Is case-specificity content-specificity? An analysis of data from extended-matching questions’, Advances in Health Sciences Education , 15(1): 55–63. DOI: http://dx.doi.org/10.1007/s10459-009-9169-z
- Durning, S., Artino, A., Boulet, J., Dorrance, K., van der Vleuten, C. & Schuwirth, L. (2012). ‘The impact of selected contextual factors on experts’ clinical reasoning performance (does context impact clinical reasoning performance in experts?)’, Advances in Health Sciences Education , 17(1): 65–79. DOI: http://dx.doi.org/10.1007/s10459-011-9294-3
- Eva, K. (2005). ‘What every teacher needs to know about clinical reasoning’, Medical Education , 39(1): 98–106. DOI: http://dx.doi.org/10.1111/j.1365-2929.2004.01972.x
- Eva, K. & Norman, G. (2005). ‘Heuristics and biases--a biased perspective on clinical reasoning’, Medical Education , 39(9): 870–2. DOI: http://dx.doi.org/10.1111/j.1365-2929.2005.02258.x
- Evans, J.S.B.T. & Stanovich, K.E. (2013). ‘Dual-Process Theories of Higher Cognition: Advancing the Debate’, Perspectives on Psychological Science , 8(3): 223–241. DOI: http://dx.doi.org/10.1177/1745691612460685
- Everitt, S. (2011). Clinical Decision Making in Veterinary Practice . University of Nottingham.
- Graber, M.L. (2013). ‘The incidence of diagnostic error in medicine’, BMJ Quality and Safety , 22(SUPPL.2): 21–27. DOI: http://dx.doi.org/10.1136/bmjqs-2012-001615
- Graber, M.L., Franklin, N. & Gordon, R. (2005). ‘Diagnostic Error in Internal Medicine’, Archives of Internal Medicine , 165(13): 1493. DOI: http://dx.doi.org/10.1001/archinte.165.13.1493
- Hatala, R., Norman, G. & Brooks, L. (1999). ‘Influence of a Single Example on Subsequent Electrocardiogram Interpretation’, Teaching and Learning in Medicine , 11(2): 110–117. DOI: http://dx.doi.org/10.1207/S15328015TL110210
- Klein, J. (2005). ‘Five pitfalls in decisions about diagnosis and prescribing’, British Medical Journal , 330(7494): 781–783. DOI: http://dx.doi.org/10.1136/bmj.330.7494.781
- Maddison, J.E., Volk, H.A. & Church, D.B. (2015). Clinical Reasoning in Small Animal Practice . John Wiley & Sons Ltd.
- Mamede, S., Van Gog, T., Schuit, S.C.E., Van den Berge, K., Van Daele, P.L.A., Bueving, H., Van Van der Zee, T., Van den Broek, W.W., Van Saase, J.L.C.M. & Schmidt, H.G. (2017). ‘Why patients’ disruptive behaviours impair diagnostic reasoning: A randomised experiment’, BMJ Quality and Safety , 26(1): 13–18. DOI: http://dx.doi.org/10.1136/bmjqs-2015-005065
- Mamede, S., Schmidt, H. & Penaforte, J. (2008). ‘Effects of reflective practice on the accuracy of medical diagnoses’, Medical Education , 42(5): 468–475. DOI: http://dx.doi.org/10.1111/j.1365-2923.2008.03030.x
- May, S. (2013). ‘Clinical Reasoning and Case-Based Decision Making: The Fundamental Challenge to Veterinary Educators’, Journal of Veterinary Medical Education , 40(3): 200–209. DOI: http://dx.doi.org/10.3138/jvme.0113-008R
- Van Merrienboer, J. and Sweller, J. (2010). ‘Cognitive load theory in health professional education: design principles and strategies’, Medical Education , 44(1): 85–93. DOI: http://dx.doi.org/10.1111/j.1365-2923.2009.03498.x
- Norman, G. (1989). ‘The Development of Expertise in Dermatology’, Archives of Dermatology , 125(8): 1063. DOI: http://dx.doi.org/10.1001/archderm.1989.01670200039005
- Norman, G. (2005). ‘Research in clinical reasoning: past history and current trends’, Medical Education , 39(4): 418–427. DOI: http://dx.doi.org/10.1111/j.1365-2929.2005.02127.x
- Norman, G.R., Monteiro, S.D., Sherbino, J., Ilgen, J.S., Schmidt, H.G. & Mamede, S. (2017). ‘The Causes of Errors in Clinical Reasoning: Cognitive Biases, Knowledge Deficits, and Dual Process Thinking’, Academic Medicine , 92(1): 23–30. DOI: http://dx.doi.org/10.1097/ACM.0000000000001421
- Oxtoby, C., Ferguson, E., White, K. & Mossop, L. (2015). ‘We need to talk about error: Causes and types of error in veterinary practice’, Veterinary Record , 177(17): 438. DOI: http://dx.doi.org/10.1136/vr.103331
- Schmidt, H. & Rikers, R. (2007). ‘How expertise develops in medicine: knowledge encapsulation and illness script formation’, Medical Education , 41(12): 1133–1139. DOI: http://dx.doi.org/10.1111/j.1365-2923.2007.02915.x
- Sherbino, J., Kulasegaram, K., Howey, E. & Norman, G. (2014). ‘Ineffectiveness of cognitive forcing strategies to reduce biases in diagnostic reasoning: A controlled trial’, Canadian Journal of Emergency Medicine , 16(1): 34–40. DOI: http://dx.doi.org/10.2310/8000.2013.130860
- Shimizu, T., Matsumoto, K. & Tokuda, Y. (2013). ‘Effects of the use of differential diagnosis checklist and general de-biasing checklist on diagnostic performance in comparison to intuitive diagnosis’, Medical Teacher , 35(6). DOI: http://dx.doi.org/10.3109/0142159X.2012.742493
- Slovic, P., Finucane, M., Peters, E. & MacGregor, D. (2004). ‘Risk as Analysis and Risk as Feelings: Some Thoughts about Affect, Reason, Risk, and Rationality’, Risk Analysis , 24(2): 311–322. DOI: http://dx.doi.org/10.1111/j.0272-4332.2004.00433.x
- Stanovich, K.E. & Toplak, M.E. (2012). ‘Defining features versus incidental correlates of Type 1 and Type 2 processing’, Mind and Society , 11(1): 3–13. DOI: http://dx.doi.org/10.1007/s11299-011-0093-6
- Thammasitboon, S. & Cutrer, W. (2013). ‘Diagnostic Decision-Making and Strategies to Improve Diagnosis’, Current Problems in Pediatric and Adolescent Health Care , 43(9): 232–241. DOI: http://dx.doi.org/10.1016/j.cppeds.2013.07.003
- Vandeweerd, J., Kirschvink, N., Clegg, P., Vandenput, S., Gustin, P. & Saegerman, C. (2012). ‘Is evidence-based medicine so evident in veterinary research and practice? History, obstacles and perspectives’, The Veterinary Journal , 191(1): 28–34. DOI: http://dx.doi.org/%2010.1016/j.tvjl.2011.04.013
Ask the author
How to reference this publication (harvard system).


Copyright Statement
Readers also viewed these publications, diagnóstico por imagen – argos – n°259, junio 2024, manejo de la osteoartrosis canina y felina - argos - n°259 supl., junio 2024, 4 estrategias para mitigar el estrés térmico - albéitar - nº 266, mayo/junio 2024, analgesia - argos - n°258, mayo 2024, dermatología - argos - n°257, abril 2024, the vet symposium 2022 - royal canin (video recordings), caring for the senior pet - veterinary focus - vol. 33(3), dec. 2023, veterinary evidence - vol 9 n°1, jan-mar 2024, patología digestiva - argos n°256, marzo 2024, abordaje clínico de la leishmaniosis felina - argos n°255 supl., enero/febrero 2024, cardiología - argos - n°255, enero/febrero 2024, veterinary evidence - vol 8 n°4, oct-dec 2023, pacientes exóticos – argos – n°254, diciembre 2023, traumatología - argos nº 253, noviembre 2023, oncología - argos nº 252, octubre 2023, veterinary evidence - vol 8 n°3, jul-sep 2023, patología pediátrica - argos nº 251, septiembre 2023, topics in feline medicine - veterinary focus - vol. 33(2), aug. 2023, diagnóstico temprano: la clave frente al bvdv - albeitar - n°261, julio/agosto 2023, israel journal of veterinary medicine - vol. 78(2), june 2023, insuficiencia cardiaca - argos nº250 supl., julio/augosto 2023, oftalmología - argos n°250, julio/augosto 2023, bienestar y comportamiento - argos n°249, junio 2023, anestesia - argos n°248, mayo 2023, gastrointestinal topics - veterinary focus - vol. 33(1), apr. 2023.
Veterinary Evidence is an online, open access, peer-reviewed journal owned and published by RCVS Knowledge. If you would like to receive updates on recent publications, you can register here . If you would like to submit an manuscript for publication in the Veterinary Evidence journal, you can consult the Guidelines for Authors .

Evidence-based clinical decision support tools and calculators for veterinary professionals
What is VetEmCRIT?

VetEmCRIT is an online platform that was created to ignite critical thinking in veterinary emergency and critical care field. Our goal is to bring the most up-to-date evidence-based information related to the veterinary and human emergency medicine, critical care, trauma, and resuscitation. We aim to publish at least one blog post a month. Our mission is to induce a paradigm shift of what is considered possible in veterinary emergency and critical care field at the moment and promote the best quality cutting-edge care. We are going to advance critical thinking in one veterinary ICU at a time.
Share this:

Veterinary Science & Technology
ISSN: 2157-7579

Veterinary Critically Important Critical Thinking Skills
7 th international veterinary congress september 04-05, 2017 | paris, france.
Megan Brashear
VCA Northwest Veterinary Specialists, USA
Posters & Accepted Abstracts : J Vet Sci Technol
Critically Important Critical Thinking Skills: Veterinary nursing requires more than simply checking off boxes on treatment sheets, it involves thinking through the reasons for and the expectations from each treatment performed. This lecture will cover not only the importance of learning to think critically with every patient interaction, but uses case studies to allow the audience to practice these skills and think through how they can help in real life situations. An emphasis is placed on creating nursing plans and following through each step. Ideas for critical thinking exercises to be used in the practice will be discussed and attendees encouraged to implement ideas in their hospitals. Advanced Trauma Management Case Studies: Polytrauma, bleeding disorders, traumatic brain injury, penetrating thoracic wounds, intestinal evisceration, some trauma patients take a turn for the worse or present to the ICU requiring special care and knowledge. This lecture will cover Acute Traumatic Coagulopathy and discusses damage control resuscitation in appropriate patients. Multiple case studies will be utilized to allow the audience the opportunity to think through ��?what would you do� scenarios and discuss why and why not when it comes to fluid resuscitation, pain management, nursing care, and anticipating changes in each patient. Understanding Acid/Base and Blood Gas Measurements: The acid/base balance in the body is delicate and often challenging to understand. Beginning with the basics, this lecture will help veterinary nurses to understand why they should be concerned with their patient��?s acid/base status and how to anticipate and understand compensatory mechanisms. A fun and simple tic tac toe method will be taught that aids in determining primary disorders. Finally, anticipating oxygen needs using arterial blood gas results will be covered using real-life patient blood gas readings. Emergency Care for the Seizure Patient: Seizure disorders are frequently seen in the veterinary clinic. This lecture will cover seizure recognition including atypical and focal seizures, emergency care for status epilepticus including emergency drug doses and routes, and drugs utilized for maintenance therapy. The bulk of the time is spent discussing the nursing care necessary for monitoring these patients ensuring the nursing team can recognize changes in minimally responsive patients and nursing care for recumbent neurologic patients. The Highs and Lows of Electrolyte Disorders: Alterations in sodium, chloride, and potassium can cause dramatic changes in veterinary patients requiring careful monitoring and anticipating changes from the nursing team. This lecture will break down the reasons, physical signs, and treatments of electrolyte abnormalities placing an emphasis on recognition of physical signs. Nurses attending will gain confidence in which patients require closer monitoring for electrolyte disorder complications. A discussion of fluid therapy selection and reasoning will be included, along with case studies from the ICU.
Awards & Nominations
50+ million readerbase, journal highlights, google scholar citation report, citations: 4472.
Veterinary Science & Technology received 4472 citations as per Google Scholar report
Veterinary Science & Technology peer review process verified at publons
Related Links
Pmc/pubmed indexed articles, open access journals.
- Celebrate 35 years of personalized CE at Fetch Kansas City!
- Publications
Using Critical Thinking in Clinical Pathology: Vet Techs
David Liss, RVT, VTS, CVPM, program director at Platt College, discusses the need for critical thinking in clinical pathology.
Interview Transcript (slightly modified for readability)
“I think clinical pathology is all about critical thinking; for example, a patient comes in and they have blood drawn and a veterinary technician is looking under the microscope at the different cells. We cannot legally diagnose, but we can certainly assess what we are seeing. If we see an organism that we recognize or if we see signs of anemia or changes in the red blood cell color that indicate different diseases, there are two options that we can take. 1) Non-critical thinking: which would be to write down our findings on a chart, give it to the veterinarian and move on to the next thing. That chart may sit in the rack for an hour or two and the patient is sitting in the cage. 2) Critical thinking: [Recognize] this patient is anemic, let’s get some more bloodwork; what is their packed cell volume (PCV); do I need to prepare for a transfusion; let me alert the veterinarian—all of those pieces come together and that patient gets a lot higher quality care in a much shorter amount of time. Rather than the tradition of just writing down a finding and a line of things, and no thinking as to what does this mean; how can I help; what can I assist with; what do I need to prepare for [that could potentially] be happening.”

Rebuilding the GI barrier
Robin A Saar, RVT, VTS (Nutrition) discussed nutrients and fecal microbiota transplant in an interview at the 2024 AVMA Convention in Austin, Texas.

Breaking down the barriers to veterinary nursing as a sustainable career
A deep dive with VEG leaders

Common diseases in bees
At the 2024 AVMA Convention, beekeeper Kaitlyn Krebs, DVM, MBA, DABVP (Canine/Feline) addressed viruses and parasites that can affect the entire hive

Podcast CE: New guidelines in the management of canine parvovirus
Learn and earn CE credits online with dvm360 Flex

Unlocking paths beyond clinical practice
Dr Natalie Marks shares her tips on explore a career outside of a traditional veterinary role

Reaching patients affected by wildfire
Deb Zoran, DVM, PhD MS, director of the Texas A&M Veterinary Emergency Team, describes some of what wildfire response volunteers saw during their recent deployment, in an interview with dvm360®.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

The 6 Essential Skills of Emergency Vet Nurses and Technicians
Emergency vet nurses and technicians face a unique set of challenges in their daily work – discover their unique strengths and skills.

Share this post!
Emergency veterinary nurses and technicians play a crucial part in providing life-saving care to animals in the most critical conditions. Responsible for managing and treating animals during emergencies, vet nurses and techs ensure that pets receive timely and attentive care in a fast-paced and high-pressure environment. And to excel in this field of veterinary nursing, you’ll need to possess a unique combination of skills that enable you to think on your feet, remain calm under pressure, and provide compassionate care to both animals and their owners.
In this article, we’ll guide you through six essential skills required for emergency veterinary nurses and technicians. These qualities and competencies are needed to provide a high standard of patient care in a clinical emergency setting. Whether you’re considering a career in emergency veterinary care or want to enhance your existing veterinary nursing skills, this article will give you valuable insights into the abilities that are essential for success.
What are the essential skills of emergency vet nurses and technicians?
Emergency vet nurses & techs skill #1 – critical thinking.

Emergency Vet Nurses & Techs Skill #2 – Task Switching

Emergency Vet Nurses & Techs Skill #3 – Communication Skills

Emergency Vet Nurses & Techs Skill #4 – Compassion and Empathy

Emergency Vet Nurses & Techs Skill #5 – Technical Skills

Key technical skills in an emergency setting include monitoring and medication. Being able to monitor a patient’s vital signs and respond appropriately to changes in these values can be life-saving. This can also include the ability to perform various medical procedures, such as placing catheters (IV, arterial, nasal & urinary), intubation, and wound care. Emergency veterinary nurses and technicians must be able to work efficiently and effectively in a fast-paced, high-pressure environment, often performing multiple procedures across several patients.
Further education and training for vet nurses in technical skills are also crucial to stay up-to-date with advances in veterinary medicine and updated procedures and practices. As veterinary medicine continues to evolve, emergency veterinary nurses and technicians must be able to focus on the ongoing development of technical skills through continuing education such as workshops, seminars and veterinary events .
Emergency Vet Nurses & Techs Skill #6 – Adaptability

Working in a high-pressure and fast-paced environment by nature involves the ability to adapt. And while you won’t be able to learn how to adapt through reading it in a book, this skill will eventually come naturally with exposure to veterinary emergency. When a patient is critical, time is of the essence, and it can be necessary to quickly adapt to achieve the best possible outcome. So learn from your experienced team members who will support you on how to adapt and shift focus quickly. Emergency veterinary nurses and technicians face a unique set of challenges in their daily work, but harnessing these skills helps provide the necessary care and support to pets and their owners during times of crisis.
We also recommend

DrAndyRoark.com
Articles, Videos, & Training on Pets & Veterinary Medicine
The Biggest Myths about Vets and Nutrition
March 10, 2016 by Dr. Andy Roark Community

I’m a big believer that most “black and white” statements about nutrition are oversimplified, frequently to the point of being inaccurate; and that the longer, grayer story is really the better one.
While I could (and just might) write an entire series based on this introduction, today’s long-overdue post addresses a mostly inaccurate statement that is frequently made by those offering pet nutrition advice online, and even occasionally by veterinarians. I’m referring to the myth “veterinarians don’t know anything about nutrition.”
Nutrition Education in Vet School
First, some truths. All graduates of US veterinary schools, no matter when they graduated, have nutrition integrated into their curriculum, whether it was a required course labeled “Nutrition 407” or whether it was sprinkled into other aspects of medicine, it’s in there. Some nutrition knowledge is also requisite to pass examinations for veterinary graduates to practice in the US.
I’ll be the first to agree that some veterinary institutions don’t provide enough nutrition training; however, even those institutions have curriculum that incorporates critical thinking, research, and the importance of continuing education . To maintain licensure to practice, veterinarians are required to complete a certain amount of continuing education each year, and there are many options available for veterinarians to either brush up on nutrition or pick up where vet school left off. It’s just a matter of making an effort to do so. There really isn’t a good excuse for a veterinarian to be ignorant when it comes to nutrition.
All that said, I just revealed my feelings about black-and-white statements about nutrition, so I’ll also say that I absolutely have met a (very) few veterinarians who appear to have completely blocked nutrition from their memory and have no interest in learning something new. They exist, but they’re exceptionally rare. I do, however, stand behind the black-and-white statement that there just isn’t a good excuse for this. What can I say? No profession is perfect.

So, if (nearly) every veterinarian practicing in the US truly has some nutrition knowledge, how can it be that this myth is so prevalent, even to the point that some veterinarians say it about themselves?
While a study on veterinarians’ self-reported level of nutrition knowledge, comparing it to their educational records, and correlating these with how they approach nutrition in practice would be an amazing tool for improving nutrition care within US veterinary practices, and the best way to answer this question, it doesn’t exist, to my knowledge.
What I do have to offer, is my assessment of the situation, based on my own veterinary and residency training, my time spent teaching at veterinary universities, and several years of speaking with veterinarians and pet owners about their experiences. This is not a substitute for a more evidence-based approach, but it’s what we have.
The way I view veterinarians’ nutrition deficiencies focuses not on knowledge, but on communication.
Choices, Choices Choices
First, we have to go back 20-30 years to consider that things have changed relatively recently when it comes to nutrition. There were drastically fewer options for pet owners to choose from when it came to pet food, and pet food marketing was fairly simplistic. The body of knowledge about pet nutrition and diet formulation was much smaller, and internet access wasn’t a factor in people’s decision-making. Because of this, there was a tendency for pet owners to ask veterinarians for nutrition advice when it was needed, and to take that advice at face value. Easy.
Now, all of those factors have changed. Pet owners think about nutrition much more than they did in the past, largely due to the ease with which information is available now. There has been an explosion in the number of pet food options available, and along with this, some very smart marketing that has even managed to look like unbiased information has entered the pet food market.

In addition, science has progressed so that we now know much more about pet nutrition, and pet food and the internet has brought the general public a ton of information (some useful, some useless, much confusing). With all of these changes, people’s expectations of their veterinarian, when it comes to nutrition, have changed.
Pet owners are no longer asking for advice (even if they phrase it as such). They’re asking for a dialog. Rather than the basic instruction that would have been acceptable in the past, pet owners now want to know that their veterinarian recognizes their concerns and the energy that they’ve devoted to learning about the subject. They want the vet to be willing and able to engage in a conversation about it and they want to play an active role in determining the course of action.
Nutrition and Communication
Like most aspects of both veterinary medicine and life in general, having this conversation takes practice. Incidentally, it’s not something that gets talked about a lot, but one of the most important things that veterinary students in their clinical year, and new graduates, do is refine their explanations of common diseases and medical concepts. It takes time to figure out the most effective and efficient way to convey the most important information; and it’s different for everybody.
So, 20-30 years ago, veterinarians never had to be good at talking with pet owners about nutrition, because no one was asking if a grain-free diet would help their pet with diarrhea. No one was asking if a raw-meat-based diet would improve a skin problem, and no one was trying to balance a home-prepared diet using whole food ingredients. Again, black-and-white statements here- I don’t mean literally anyone, I just mean few enough people to justify not having to learn to have these conversations.
While nutrition is absolutely present in the veterinary curriculum in the US, talking about nutrition: not so much, with the exception of teaching by a few of my very proactive colleagues. It’s been up to vets to learn it on their own. By far, the vast majority of veterinarians that I talk to who’ll say that they “don’t know anything about nutrition” are actually able to make perfectly reasonable nutritional recommendations in most instances, but where they fall down is in answering the pet owner’s question about why they made the recommendation. They haven’t had the practice. It’s not a knowledge issue, it’s a communication issue.
False Information, Frustrated Vets

While the pet owner may be asking “is diet x good for my pet?” it’s not a yes-or-no question anymore. Veterinarians don’t usually recognize that exactly what and how a pet is fed can potentially say a lot about the pet owner, and the pet owner may have invested much energy in the subject and determined that diet x is the way to go. Some pet food marketing has given many pet owners some false ideas about what is and is not important in pet food, and when a veterinarian outright disagrees with the results of a pet owner’s research, it’s natural for that pet owner to be offended.
As a generally peaceful bunch, most veterinarians don’t enjoy being put in these situations, so it’s easy to see how “I don’t know” may be the easier (though incorrect) answer. Another scenario where “I don’t know” may incorrectly come up is in response to claims such as “feeding abc diet will cure your pet’s medical condition.” Veterinarians are trained in critical evaluation of information, so if there isn’t any valid evidence-based information on which the veterinarian can advise otherwise, “I don’t know” is the alternative to the full explanation of the importance of evidence-based medicine.
While I don’t believe that “I don’t know” is the right answer in either of these scenarios, when veterinarians are managing hospitalized patients and returning phone calls from worried pet owners in between running a hospital, surgeries, appointments that are never long enough, walk-in patients, and emergencies, with a little bit of perspective, it’s easy to understand how saying “I don’t know” and not having a 40-minute conversation about nutrition may be the answer that keeps the day on track.
I’ll try not to sound like a marriage counselor here, but if the problem is communication, then the solution is to understand the other person’s perspective and taking steps to accommodate it.
My Calls to Action
Veterinarians: Ask owners of pets requiring nutritional care or clients with concerns about feeding their pet to schedule an appointment to discuss nutrition. Consider that criticism of your client’s current feeding choices is indirectly criticism of your client and their lifestyle. Focus on providing background in evidence-based medicine and the medical basis for your recommendations. Point out the level of evidence that informs each idea being discussed.

Find a gentle (but honest) way to suggest making changes, and keep the focus on the fact that you both want to provide the best care possible to the pet.Contact a veterinary nutritionist if needed. Use this opportunity to develop your approach to talking about nutrition. You’ll say “umm” a lot and feel like it’s your first week in practice for a while, but it will become second-nature. Your client will leave with the impression that you care, that you listened, and that you do know something about nutrition.
Pet owners: It’s tricky to navigate pet nutrition advice. There’s a lot of it, and it ranges from excellent to terrible. Often terrible is cleverly disguised as excellent. There are resources for dog and cat owners that can help, but your vet is really the best person to help sort it out. However, understand that while “is diet x good for my pet?” sounds like a simple question, it isn’t. Not if you want an intelligent answer.
The answer actually involves your pet’s medical needs (the easy part because your veterinarian already has a handle on this); your pet’s current and possibly previous diets, and his/her response to them; and the logistics of feeding and lifestyle in your home. If you are honestly interested in your veterinarian’s opinion of your pet’s diet (you should be), it’s only fair that you give them an opportunity to give you a good answer.
Asking about nutrition as a “by the way” as your vet is leaving for her next appointment isn’t fair. You probably won’t be satisfied with the answer, and your veterinarian won’t get the chance to provide your pet with the best possible care. Just as you’d schedule an appointment with your vet if you had questions about your pet’s itchy skin, go ahead and schedule one for your questions about diet.
It’s not the easy way out (surprise), but between veterinarians’ expanding knowledge base in nutrition, more practice with talking about it, and a bit of perspective, the myth that veterinarians don’t know anything about nutrition can hopefully be put to rest.
This post originally appeared at Veterinary Nutrition Care .
The views and opinions expressed in this article are those of the author and do not necessarily reflect the position of the DrAndyRoark.com editorial team.

About the Author
Dr. Amy Farcas is one of only 84 veterinarians board-certified as a specialist in nutrition by the American College of Veterinary Nutrition.
Dr. Farcas earned her veterinary degree at the University of California-Davis, and then completed a rotating internship, followed by a year of practicing general and emergency medicine. By this time, she’d become fascinated with biochemistry and the effects of food on the body. She returned to the University of California-Davis for her residency in small animal clinical nutrition, and then earned a Master’s degree in nutritional biology. Dr. Farcas was the clinical nutritionist and acting service chief for the clinical nutrition service at the Matthew J. Ryan Veterinary Hospital at the University of Pennsylvania before returning to California to start Veterinary Nutrition Care; a nutrition specialty practice in the San Francisco Bay Area.
Dr. Farcas is passionate about families, teaching, and food. Her work as a veterinary nutritionist allow her to combine these to help people give pets their best.
Dr. Andy Roark Community
Read more posts by: Dr. Andy Roark Community
Connect With Us
- Privacy policy
- FOR VET CENTERS
- FOR TECH CENTERS
CRITICALTHINKING4VET NETWORK
Criticalthinking4vet is an european network that is made up of prestigious technology centers that develop cutting-edge projects in a wide variety of fields (biosanitary, smart materials, nanocomponents…) as well as VET centers. Both sectors collaborate together to create technical and labor training adapted not only to the needs of technology sector but also to the ones of students with obstacles.
From the network we believe that VET technicians have a fundamental role in the development of high technology projects, especially those young people with more obstacles that despite them demostrate a capability for improvement, dedication and learning that makes them overcome all their barriers. On the other hand, technology centers can play a fundamental role in these young people, providing them with a new experience that helps them access the labor market and developing fundamental skills for their social, professional and personal future.
PROJECTS OF THE NETWORK
In the resolution of the 2021 call for grants in the field of Vocational Training education of the Erasmus Plus Program, the project «TECHVETLAB: A SOLUTION FOR POSTCOVID-19 LABOR MARKET THROUGH A TECHNICAL TRAINING OF VET STUDENTS WITH OBSTACLES» has been awarded by the Spanish National Agency – SEPIE.
In the 2022 aid resolution in the educational field of Vocational Training of the Erasmus Plus Program, the Spanish National Agency -SEPIE has awarded us the project «BUILDING THE VOCATIONAL TRAINING OF THE FUTURE: COMPANIES AND EDUCATIONAL CENTERS FACING THE CHALLENGE OF THE ORGANIZATION AND INTEGRATION OF A MORE INCLUSIVE AND DIGITAL VET. (FUTURVET)”.
In the resolution of the call aid for 2020 in the educational field of the Erasmus Plus Programme, the project “VIRTUAL INTERNSHIPS IN TECH CENTERS: TRAINING VET STUDENTS WITH OBSTACLES INTO A INNOVATIVE DIGITAL METHODS OF REMOTE WORKING AND ELEARNING CREATED FROM COVID-19” was granted by the Spanish National Agency – SEPIE.
In the resolution of the 2021 call for grants in the field of Vocational Training education of the Erasmus Plus Program, the project «TVET STUDENTS INTO TECHNOLOGY COMPANIES» has been awarded by the Spanish National Agency – SEPIE.
In the call of March 2017 in the educational field of the Erasmus Plus Programme, it was granted by the Spanish National Agency – SEPIE the project CRITICAL THINKING AS A STEP FORWARD IN VET EDUCATION: VET students immersed in high technology teams.
ENTITIES OF THE NETWORK
News of the network, methodological guide, inted2024 – application accepted.
Coordinator: IKASIA TECHNOLOGIES SL
C/ Jesús y María, num 26 – bajo – 46008 (Spain)
mail:[email protected]
Web: www.ikasia.es
Chief editor: Luis Gómez Estrada, CEO Ikasia Technologies sl
This network has been cofunded with support from the European Commission. This publication reflects the views only of the author, and the Commission cannot be held responsible for any use which may be made of the information contained therein.
This publication is available in Open Access under the Attribution-ShareAlike 3.0 IGO (CC-BY-NC-ND 3.0 IGO) license (http:/ creativecommons.org/licenses/by-sa/3.0/igo/). By using the content of this publication, the users accept to be bound by the terms of use of the ERASMUS PLUS GUIDE 2020 and also of IKASIA TECHNOLOGIES SL.
All the images used are free of rights and have been made in the project or extracted from the web ttps: //unsplash.com/photos.

IMAGES
COMMENTS
Applying Critical Thinking to the Nursing Process "The nursing process is utilized much more frequently in human medicine, but there's no reason we shouldn't use it as well, especially with critically ill patients," said Brashear, explaining that the process breaks down into 5 steps. ... The Vet Blast Podcast kicks of Pride month with ...
Critical thinking is not something that we are born with--it is a skill that must be taught and practiced. In school, many of us are taught to memorize facts and regurgitate them on ... also veterinarians, assistants, client services, and especially pet owners. Participating in the nursing process will help to develop all of these skills and is ...
Effective clinical teaching is essential for the development of veterinary learners. Teaching clinical reasoning is a challenge for veterinary instructors as many lack adequate training in clinical teaching. In this paper, we propose the use of the five-microskills (FMS; also known as the one-minute preceptor) model of clinical teaching as a ...
Title: "Paws and Thought: How Critical Thinking Helps Vets Keep Pets Healthy!"In the world of veterinary medicine, critical thinking is like a superpower that helps veterinarians solve puzzles to keep our furry friends healthy and happy. Just like detectives, vets use their keen observation skills, logic, and knowledge to diagnose and treat animals.
Critical thinking is defined by Scriven and Paul as "the intellectually disciplined process of actively and skillfully conceptualizing, applying, analyzing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action." 3 Traditional veterinary curricula have usually consisted ...
around the world.WHAT IS. RITICAL THINKING?In human health care, critical thinking in nursing has been defined this way: "Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, open-mindedness, perseveranc.
Metacognition—This is a critical awareness of one's thought processes and learning, and an understanding of the patterns of thinking and learning. Self-directed learning—learners take charge of their own learning process by identifying learning needs, goals, and strategies and evaluating learning performances and outcomes. Learner ...
Eagleman presents 5 principles for encouraging creative thinking, and I'd like to suggest activities relevant to veterinary education that might follow 4 of the most implementable principles for veterinary instruction. "Bend, break, blend". Providing problems or questions that are formulaic and feeding slightly iterative problems back to ...
ABSTRACT. Clinical reasoning is the process by which veterinary surgeons integrate a multitude of clinical and contextual factors to make decisions about the diagnoses, treatment options and prognoses of their patients. The brain utilises two methods to achieve this: type one and type two reasoning.
Let's look at Masten's 5 recommendations for development of critical thinking and see how they might be interpreted for veterinary medicine, particularly in the context of case analysis exercises. 1. Accountable Talk: By structured discussion to demonstrated and practice evidence-based thinking.
Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge."1. That's a lot for a veterinary nurse to apply in a trauma care situation, but a veterinary nurse with critical thinking skills can adapt to new ...
Module Description. Learn about flipping content and blended learning, all with the goal of creating more time for instructor-student interaction over critical clinical thinking activities. This resource module is designed for a learner to understand the principles of this form of student-centered learning, and also designed for instructors to ...
To help develop reflective competence among future professionals, 30 veterinary students' reflective assignments were analysed by thematic text analysis. Theoretical frameworks were based on published criteria for critical and core reflection. Results
VetEmCRIT is an online platform that was created to ignite critical thinking in veterinary emergency and critical care field. Our goal is to bring the most up-to-date evidence-based information related to the veterinary and human emergency medicine, critical care, trauma, and resuscitation. We aim to publish at least one blog post a month. Our ...
Abstract : Critically Important Critical Thinking Skills: Veterinary nursing requires more than simply checking off boxes on treatment sheets, it involves thinking through the reasons for and the expectations from each treatment performed. This lecture will cover not only the importance of learning to think critically with every patient ...
More follow-up research would be useful to track whether and how such formats could have an impact in the veterinary context, and, specifically, whether the use of creative methods could help vets cope with the 'moral stress' they experience. 10 At the University of Nottingham, staff research leave meant that the competition was paused in ...
Veterinarians use critical thinking to stay resourceful and to have different approaches to situations. Sometimes, there are multiple procedures to treat a pet, but a veterinarian who thinks critically finds a treatment that best heals the animal. There may be instances where a veterinarian has to find a treatment for a challenging condition ...
1) Non-critical thinking: which would be to write down our findings on a chart, give it to the veterinarian and move on to the next thing. That chart may sit in the rack for an hour or two and the patient is sitting in the cage. 2) Critical thinking: [Recognize] this patient is anemic, let's get some more bloodwork; what is their packed cell ...
Furthermore, that these are necessary to move a novice clinician to an expert. Buur and colleagues (2012) showed that overall veterinary student performance on a general critical thinking skills tests (California Critical Thinking Skills Test) did not improve following a 2 year problem-based curriculum.
When a patient presents in an emergency, vet nurses and techs must work alongside veterinarians and use their critical thinking to stabilise the patient and determine the underlying cause of the symptoms. This may involve initial triage and patient history, performing diagnostic tests such as blood work or X-rays, and regularly assessing the ...
I'll be the first to agree that some veterinary institutions don't provide enough nutrition training; however, even those institutions have curriculum that incorporates critical thinking, research, and the importance of continuing education. To maintain licensure to practice, veterinarians are required to complete a certain amount of ...
Criticalthinking4vet is an european network that is made up of prestigious technology centers that develop cutting-edge projects in a wide variety of fields (biosanitary, smart materials, nanocomponents…) as well as VET centers. Both sectors collaborate together to create technical and labor training adapted not only to the needs of ...
2. Checking the accuracy of these assumptions by exploring as many different perspectives viewpoints, and sources as possible. 3. Making informed decisions that are based on research. I'll give an example of how I went through these three phases in regard to an assumption I held about fish.